Experimental Study on Anatomic Reduction of Lateral Pterygoid Muscle (Simulated Manipulation Fracture Reduction) and Condylar Free Reduction for Condylar Fracture
2023-10-31JunyiYOUXiaofengSHENQihanMAGuoqiangLIANG
Junyi YOU, Xiaofeng SHEN, Qihan MA, Guoqiang LIANG
Suzhou TCM Hospital Affiliated to Nanjing University of Chinese Medicine, Suzhou 215009, China
Abstract [Objectives] To compare the fracture healing of keeping lateral pterygoid muscle anatomic reduction (simulated manipulation fracture reduction) with condylar free reduction in the treatment of condylar fractures. [Methods] Twenty-four New Zealand rabbits were randomly divided into two groups to mandibular condylar neck fracture model was established. one team keep the lateral pterygoid muscle, the other excise it. Cervical vascular perfusion was done with ink before animals executed after operation 2, 4, 6 and 8 weeks. Bilateral anteroposterior and mediolateral condylar diameters measured. Changes of operation side condylar proliferating layer, microvessel number and bone parameters were observed and analyzed after slices and HE staining. [Results] The mediolateral condylar diameters of operation side were significantly smaller than health side in condylar free reduction group at the 4, 6, 8 weeks (P<0.05), but there was no statistical difference in the anteroposterior condylar diameters at each time point (P>0.05). There were no significant differences in the anteroposterior and mediolateral condylar diameters of the anatomic reduction lateral pterygoid muscle group compared between the operation side and health side (P>0.05). The number of microvessel in condylar free reduction group were smaller than those in anatomic reduction lateral pterygoid muscle group (P <0.05). There were significant differences in BV/TV, Tb.Th, Tb.Sp between the condylar free reduction group and the anatomic reduction lateral pterygoid muscle group (all P<0.05), and the Tb. N were significantly differences between two groups at the 4, 6, 8 weeks (P<0.05). [Conclusions] When the condyle is fractured it should keep lateral pterygoid muscle (manipulation fracture reduction) as possible, which is important in the fracture healing and functional recovering of mandibular.
Key words Condylar fracture, Anatomic reduction lateral pterygoid muscle, Condylar free reduction, Blood supply reconstruction, Fracture healing
1 Introduction
The trauma and surgical treatment of condylar fracture are difficult, and if not handled properly, it can lead to various clinical complications, affecting the function and facial shape of the temporomandibular joint in patients[1]. The main purpose of surgical treatment is to restore the maxillofacial appearance and temporomandibular joint function[2]. Surgical reduction methods mainly include anatomical reduction of the lateral pterygoid muscle and free reduction of the condyle[3]. Previous studies have mostly compared the clinical efficacy of two reduction methods, with little experimental research, especially on the healing process. This study used New Zealand white rabbits to construct an animal model of transverse fracture of the condyle neck, and performed anatomical reduction of the lateral pterygoid muscle (simulating the principle of manual fracture reduction) and free reduction of the condyle, respectively. Through condylar measurement and histological analysis, a comparative study was conducted on the healing process of the two reduction methods, providing practical basis for clinical work.
2 Material and methods
2.1 Experimental animals and groups24 healthy adult New Zealand white rabbits with a body weight of 2.4-2.6 kg were purchased from Zhaoyan (Suzhou) New Drug Research Center Co., Ltd. The experimental animal license number is SCXK (Suzhou) 2023-0004. The rats were divided into a condylar free reduction group and a lateral pterygoid muscle anatomical reduction (simulated manual reduction) group using a completely randomized method, with 12 rats in each group. Ethical batch number (2022 Lunyan 050).
2.2 Establishment of animal modelAnimals were weighed. The indwelling needle washed with heparin normal saline (10 U/mL) established ear vein channel. 1% propofol was slowly injected intravenously with an initial dose of 1 mL/kg. The anesthesia was successful when the Corneal reflex disappeared. During the operation, corneal reflex recovered, and 0.2 mL/kg of anesthetic was added. Made an incision in front of the eardrum, separate layer by layer, and exposed the mandibular ramus and condyle. Performed a transverse osteotomy with a TF-11 car needle 1 cm below the condyle. The condyle free reduction group carefully peeled off the soft tissue, removed the condyle, and completely restored it to its original implant site; the external pterygoid muscle anatomical reduction group confirmed the fracture and gently pulled the bone segment on the condyle side to simulate the joint cavity damage caused by clinical fractures. TF-11 car needle drilling through bone to prepare nail holes, micro titanium plate fixation, penicillin physiological saline flushing of the surgical cavity, and suturing[4]. After surgery, no intermaxillary fixation was performed and 300 000 units of penicillin were injected into the muscles daily for 3 d. After one week of soft food feeding, it was changed to regular feed. After 7 d of surgery, the suture was removed, and no animal died unexpectedly during the experiment.
2.3 Detection indicators and methodsVascular ink perfusion and condylar measurement: After 2, 4, 6, and 8 weeks of anesthesia, three animals from each group were anesthetized and bilateral carotid and venous catheterization was performed. Heparin physiological saline (10 U/mL) is slowly injected into the arterial tube. After the liquid from the venous tube is clear, the vein is ligated and ink is slowly injected. The bilateral condyles were dissected after the animals’ heads were evenly blackened, and the anterior and posterior diameters, internal and external diameters of the bilateral condyles were measured with Vernier scale (accuracy: 0.02 mm)[5].
After sacrifice, the operative condyle were removed and fixed in 10% buffered formalin. The samples were decalcified in 10% ethylene diamine tetraacetic acid (EDTA), paraffin-embedded and routinely processed. Semi-serial, 5-mm thick coronal sections were obtained and stained with hematoxylin and eosin (H&E) to perform light microscopic histological and histomorphometric analyses. The sites from all of the groups were studied at the same magnification, and the qualitative data observed included the fracture site and temporomandibular joint evaluations[6].
2.4 Statistical analysisThe results were analyzed using SPSS 21.0. The data obtained were tested using the Kruskale Wallis test to check for possible differences between the two groups, when compared concomitantly, among the variables of interest. When statistically significant differences were found the Manne Whitney test was applied, adjusted by the Bonferroni correction, to identify which groups differed from the others in pairwise comparisons. The level of significance was set atP<0.05.
3 Results and analysis
3.1 Condylar measurementsComparison of the internal diameter and anteroposterior diameter of the condyle between the surgical and healthy sides of each group of animals: The internal and external diameter of the condyle decreased in the free reduction group at 4, 6, and 8 weeks on the surgical side (P<0.05), and there was no statistically significant difference (P>0.05) between the anatomical reduction group of the lateral pterygoid muscle at different time points. There was no statistically significant difference (P>0.05) between the two groups in the anterior and posterior diameter of the condyle, as shown in Table 1.

Table1 The results of condyle specimens were compared (n=3,
3.2 Observation and comparison of the proliferative layer of condyle on the operative sideThe condylar free reduction group showed no significant changes in the proliferative layer at 2 weeks postoperatively. It began to thicken at 4 weeks postoperatively, and significantly thickened and densely packed cells at 6 weeks postoperatively compared to 4 weeks. The proliferative layer remained relatively thick at 8 weeks postoperatively. In the anatomical reduction group of the lateral pterygoid muscle, the proliferative layer thickened and the number of cells increased 2 weeks after surgery, and the thickening became more pronounced 4 weeks after surgery. The thickness of the proliferative layer was slightly thinner at 6 weeks after surgery, and it basically returned to normal at 8 weeks after surgery. The indication is that the anatomical reduction group of the lateral pterygoid muscle started the repair and reconstruction of the condyle earlier, as shown in Fig.1.
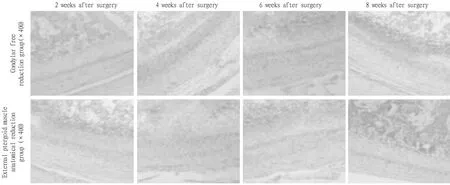
Fig.1 The proliferative layer of condyle after operation
3.3 The number of microvessels in each groupThree sections were randomly selected from the surgical specimens. Low magnification mirror (×400) Select three areas with high ink distribution in the slices, and collect images of these areas under high-power microscopy before counting the number of microvessels. The number of microvessels in the anatomical reduction group of the lateral pterygoid muscle was higher than that in the free reduction group of the condyle at all postoperative weeks (P<0.05), as shown in Table 2 and Fig.2.
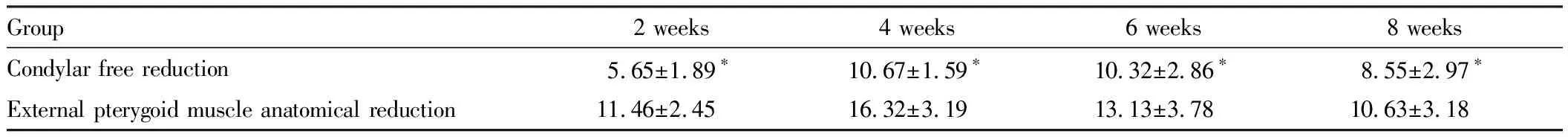
Table 2 The number of microvessels in each group after operation
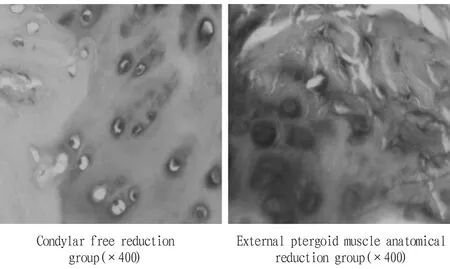
Fig.2 HE staining results in both groups at two weeks after surgery
3.4 Comparative analysis of bone parametersRandomLy select 3 sections from the surgical side specimens and observe them under light microscopy (×100). Measure the bone area (B. Ar, μm2), total tissue area (T. Ar, μm2) and bone trabecular circumference (B. Pm, μm). According to the Parfitt method, the bone parameters can be calculated by using the data: bone volume fraction (BV/TV)=(B. Ar/t. Ar)×100%, and higher values are conducive to bone repair; the average thickness of trabecular bone (TB.Th)=(B.Ar/B.Pm) (π/2), and the decrease of numerical value indicates osteoporosis; Number of trabeculae (Tb.N)=(B.Pm/T.Ar)×1000, the larger the value, the more bone mass; Trabecular bone dispersion (Tb.Sp)=(T.Ar-B.Ar)/B.Pm. The larger the value, the greater the bone resorption. After operation, the bone volume fraction and average trabecular thickness of the two groups were smaller in the condylar free reduction group than in the lateral pterygoid muscle anatomical reduction group at each time point (P<0.05); there was no significant difference in the number of trabeculae between the two groups at 2 weeks (P>0.05), and the anatomic reduction group of lateral pterygoid muscle in other weeks was greater than the free reduction group of condyle (P<0.05); the bone trabecular dispersion of the condylar free reduction group was greater than that of the lateral pterygoid muscle anatomical reduction group at each time point (P<0 05), as shown in Fig.3 and Table 3.

Table 3 Bone parameters were measured after operation (n=27,
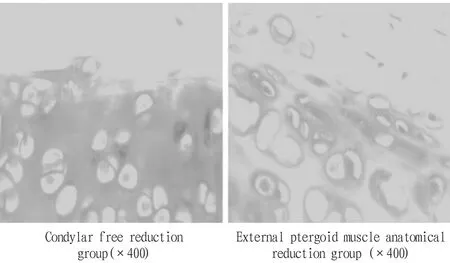
Fig.3 HE staining of the trabeculae and surrounding osteoblasts of the condyle in both groups at 8 weeks after surgery
4 Discussion
The anatomical reduction of the lateral pterygoid muscle and the free reduction of the condyle are the basic methods of condylar fracture surgery, and the main difference is whether to reduce the lateral pterygoid muscle. Appropriate surgical approaches and reduction methods can help patients recover joint movement and function faster and better[7]. The function and movement of the temporomandibular joint are coordinated by a complex composed of joint fossa, joint disc, condyle, ligament, and lateral pterygoid muscle. The lateral pterygoid muscle not only directly pulls the condylar movement, but also enters the joint disc capsule complex and the condyle to form the disc condyle complex, which plays an important role in opening and closing mouth movements. Due to its important position in the blood supply of the temporomandibular joint, its functional activity is also closely related to condylar proliferation[8]. Due to the location and direction of external forces causing the fracture, the fracture end being pulled by surrounding muscles and pushed by the mandibular branch, the condylar fracture is complex and diverse, and the anatomical structure around the condyle is complex. Therefore, the anatomical reduction of the lateral pterygoid muscle is more precise and difficult than the free reduction of the condyle. Due to the complexity of condylar fractures and the difficulty of surgical reduction, there is currently no unified standard for the selection of reduction methods.
This study compares the healing status of two reduction methods after condylar fracture, and proves that anatomical reduction of the lateral pterygoid muscle after condylar fracture can restore a certain blood supply earlier and initiate the repair and reconstruction of the temporomandibular joint. Because the healing and reconstruction of fracture is closely related to the number of microvessels, and the blood supply needs to be reconstructed after condylar free reduction, the fracture healing speed of condylar free reduction is slower than that of lateral pterygoid muscle anatomical reduction, and bone resorption is more obvious. Retaining the lateral pterygoid muscle in clinical practice is of great significance for fracture healing and temporomandibular joint function recovery. However, for those who are difficult to preserve, free reduction of the condyle is also a method.
杂志排行
Medicinal Plant的其它文章
- Quality Control of Zhuang Medicine Xiaoyan Zhiyang Lotion
- Research Progress and Ideas on the Anti-liver Fibrosis Effect of Ethnic Medicine Plumbagin Based on microRNAs/TLR4/NF-κB and NLRP3 Inflammasome Activation
- Gastroprotective Effect of Alpinia zerumbet (Pers.) Burttet Smith on Ethanol-induced Gastric Ulcers in vivo and vitro
- Exploring the Mechanism of Blumea balsamifera (L.) DC in Preventing and Treating Alzheimer’s Disease Based on HPLC-ESI-HRMS and Network Pharmacology
- Observation on Therapeutic Effect of Erxian Decoction on Relieving Low Back Pain after PVP of PMOP-derived Vertebral Fracture
- Effects of Early-stage Phased Rehabilitation Training on Acute Respiratory Distress Syndrome: A Systematic Review and Meta-analysis
