Prognostic value of hematological parameters in older adult patients with acute coronary syndrome undergoing coronary intervention: a single centre prospective study
2023-09-27UmarHafizKhanMurtazaRashidPalaImranHafeezAfshanShabirAmritDharHilalAhmadRather
Umar Hafiz Khan ,Murtaza Rashid Pala ,Imran Hafeez ,Afshan Shabir ,Amrit Dhar ,Hilal Ahmad Rather
1.Geriatric Medicine,Department of Internal Medicine,Sher-i-Kashmir Institute of Medical Sciences,Srinagar,India;2.Department of Internal Medicine,Sher-i-Kashmir Institute of Medical Sciences,Srinagar,India;3.Department of Cardiology,Sher-i-Kashmir Institute of Medical Sciences,Srinagar,India;4.Department of Internal and Pulmonary Medicine,Sher-i-Kashmir Institute of Medical Sciences,Srinagar,India
ABSTRACT BACKGROUND Cardiovascular disease is a significant contributor to the disease burden in geriatric patients.Underlying systemic inflammation is thought to be the cause of age-related changes in the bone marrow and a major risk factor for atherosclerosis.The purpose of the study was to assess the accuracy of these hematological biomarkers in predicting 30-day mortality in older patients with acute coronary syndrome (ACS).METHODS This was a prospective observational study of 601 older adult patients (age > 60 years) with ACS who underwent percutaneous coronary intervention over two years (2017-2019).The relationship between baseline hematological parameters and mortality was assessed during the 30-day follow-up.Logistic regression analysis and receiver operating characteristic curve analysis were done to evaluate for diagnostic accuracy of various hematological parameters.RESULTS The mean age of presentation was 77 ± 17 years.The mean neutrophil-lymphocyte ratio (NLR) value was 5.07 ± 4.90 and the mean platelet-lymphocyte ratio (PLR) value was 108.65 ± 85.82.On univariate analysis,total leucocyte count [odds ratio (OR)=0.85,P=0.021],hematocrit (OR=0.91,P=0.018),NLR (OR=1.10,P=0.001) and PLR (OR=1.05,P=0.001) were associated with mortality.On receiver operating characteristic curve analysis,NLR predicted mortality with 68.1% and PLR with 65.7% accuracy.On multivariate analysis,NLR (OR=1.096,95% CI: 1.006-1.15,P=0.035) was an independent predictor of 30-day mortality.CONCLUSIONS For the risk classification of all elderly ACS patients,we highly advise using NLR rather than the total white blood cell count.
With 30.3% of the total disease burden among those 60 years and older,cardiovascular illnesses most frequently brought on by atherosclerosis are the major contributors to disease burden in the older population.[1]Older patients frequently present with atypical symptoms of coronary artery disease (CAD) making diagnosis difficult and may partially increase morbidity and mortality.[2]The increasing occurrence of clonal hematopoiesis of indeterminate potential,driven by interleukin-6 signalling and/or inflammasome activation,is a process promoted by age-related changes in the bone marrow and is a key risk factor for atherosclerosis.[3]In a mouse model of induced myocardial infarction (MI),the sympathetic nervous system is activated.This causes the release of hematopoietic stem cells from bone marrow niches,which further stimulates atherosclerotic plaques and leads to atherogenesis.[4]
Hematological indices have recently attracted a lot of attention since they may offer independent information on pathophysiology and risk stratification.[5]The neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) is useful in predicting short-and long-term mortality in patients with ST-segment elevation MI (STEMI) and non-ST-segment elevation MI (NSTEMI),respectively.[6,7]Indirect inflammatory indicators of atherosclerosis,such as increased NLR and PLR,can predict major detrimental cardiovascular outcomes.[8,9]
The fundamental benefit of hematological indicators is their low cost,making them widely and conveniently accessible in routine clinical practice.Therefore,this study aimed to evaluate how well these hematological biomarkers predicted 30-day mortality in older patients with acute coronary syndrome (ACS).
METHODS
This was a single centre prospective observational study carried out on patients with ACS who were admitted to a 1200-bedded tertiary university teaching hospital in North India over two years (2017-2019) and underwent percutaneous coronary intervention (PCI).601 consecutive patients were included in this study and were approved by the Institutional Ethics Committee.Informed written consent was obtained from the patients.Inclusion criteria included patients more than 60 years of age,presenting to emergency with ACS.Exclusion criteria included patients with stable ischemic heart disease on outpatient follow-up,and patients with underlying hematological diseases (myeloproliferative neoplasm,hematological malignancies,vitamin B12 deficiency,immune thrombocytopenia,drug-induced thrombocytopenia) were excluded.The study population was divided into two groups: the young-old group (60-70 years) and the old-old group (> 70 years).Risk factors for CAD and co-morbidities were documented at the time of catheterisation by completing a questionnaire.ACS was divided into STEMI,NSTEMI and unstable angina.
Laboratory Analysis
At baseline,venous blood samples were obtained within 30 min of admission to measure haematological indices (haemoglobin,total leucocyte count,differential count,platelets,NLR,mean corpuscular volume,mean corpuscular hemoglobin,and PLR).An automated Sysmex XN-1000™ hematology analyzer (Sysmex America)was used to measure haematological indices.
Statistical Analysis
For descriptive statistics,the continuous variable was presented as mean ± SD or medians (interquartile range) as appropriate.The categorical variables are described as counts (percentages).All data were assessed for normality.The Student’st-test,Fisher’s exact probability test,and Mann-WhitneyUtest was used wherever applicable.Variables withP-value < 0.05 on univariate analysis were included in the multivariate logistic regression analysis.Receiver operating characteristic curve analysis was conducted to determine the prognostic accuracy of haematological markers in predicting shortterm mortality.The backward stepwise likelihood ratio method was used to identify the independent predictors of 30-day mortality.All tests were two-tailed andP-value < 0.05 was considered statistically significant.Statistical analysis was done using SPSS 28.0 (SPSS Inc.,IBM,Armonk,NY,USA).The significance level was set atPvalue < 0.05.
RESULTS
The demographic,clinical risk factors and co-morbidities of the 601 study patients are described in Table 1.The mean age of presentation was 77 ± 17 years.The majority were males (n=486,80.9%) and the rest were females (n=115,19.1%).There were 272 patients (45.3%) belonged to rural areas and 329 patients (54.7%) lived in urban areas.

Table 1 Demography, risk factors and comorbidities.
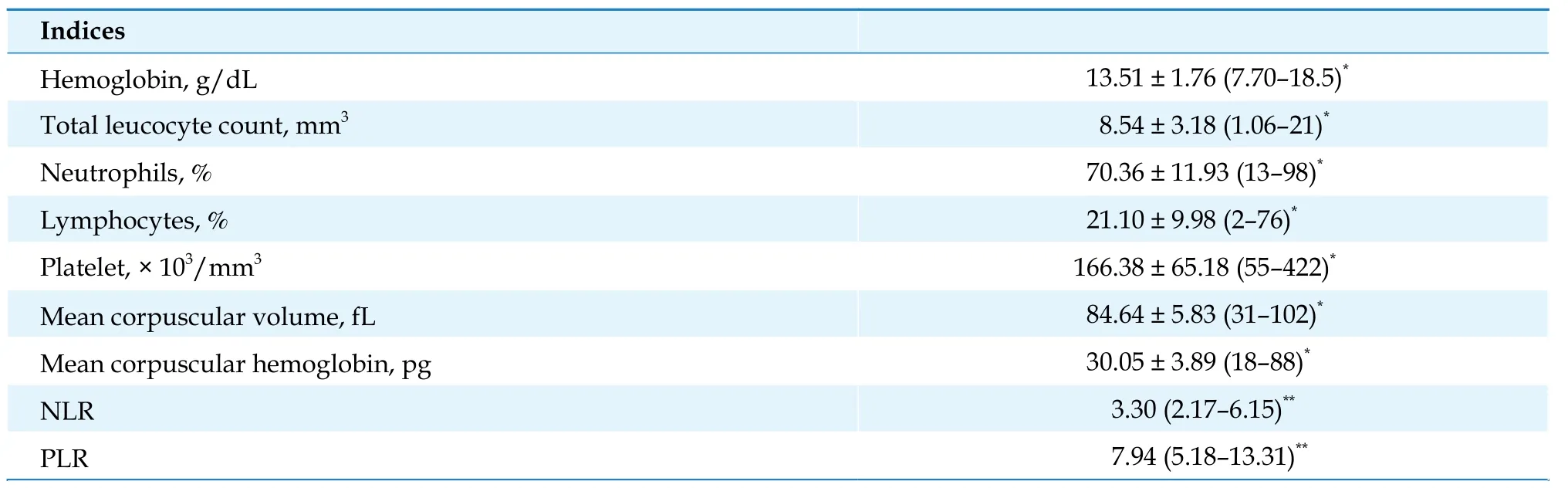
Table 2 Hematological indices of study participants.
PCI was performed in all 601 study patients.Primary PCI was performed in 77 patients (11.8%).Forty-seven patients out of these presented to secondary care hospitals in remote areas and had initial thrombolysis.Elective PCI was performed in 524 patients (87.2%).In total,565 patients had successful stent deployment and reperfusion and 36 patients were referred for coronary artery bypass grafting.
A total of 32 patients (5.3%) died post-PCI within 30 days.The thirty-day mortality was 2.7% in the young-old group and 14.1% in the old-old group (P< 0.0001),respectively.NLR,PLR,and hematocrit were associated with mortality and were statistically significant (Table 3).

Table 3 Haematological parameters related to 30-day mortality.
Higher mortality was seen in female patients (n=11,9.5%),as compared to male patients (n=21,4.32%) (P<0.028).On univariate analysis,total leucocyte count [odds ratio (OR)=0.85,P=0.021],hematocrit (OR=0.91,P=0.018),NLR (OR=1.10,P=0.001) and PLR (OR=1.05,P=0.001) were associated with mortality (Table 4).
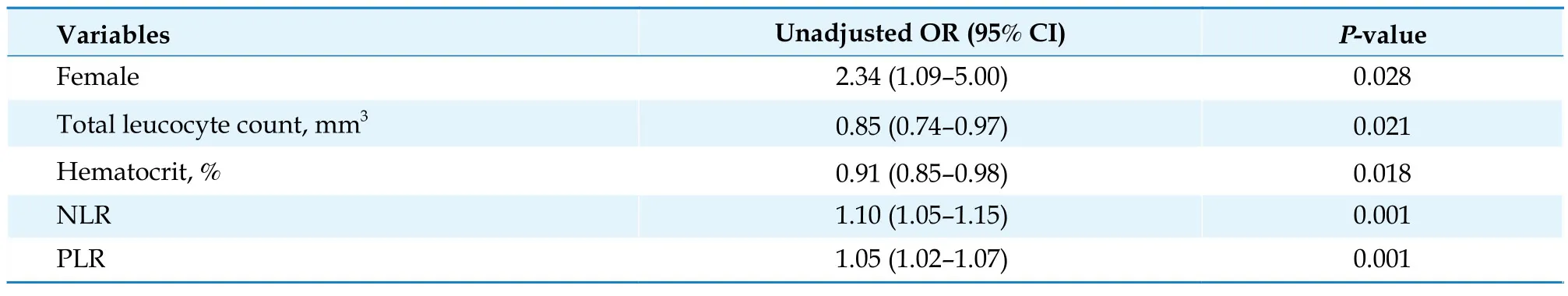
Table 4 Univariate analysis of parameters.
Figure 1 depicts the receiver operating characteristic curve analysis of NLR and PLR with the outcome as mortality.We found that NLR has a diagnostic accuracy of 68.1% for predicting mortality,whereas PLR has a slightly lower accuracy of 65.7%.A cut-off of 3.30 NLR (median NLR) was associated with a sensitivity of 75% and specificity of 52%.A cut-off of 7.94 PLR (median PLR)was associated with a sensitivity of 72% and specificity of 52%.

Figure 1 ROC curve analysis of NLR and PLR as predictors of mortality. The area under the ROC for NLR was 0.681 (P=0.001)and the area under the ROC for PLR was 0.657 (P=0.003).NLR: neutrophil-lymphocyte ratio;PLR: platelet-lymphocyte ratio;ROC:receiver operating characteristic.
Only NLR (OR=1.096,95% CI: 1.006-1.15,P=0.035)was an independent predictor of 30-day mortality in elderly patients with ACS on multivariate analysis as depicted in Table 5.
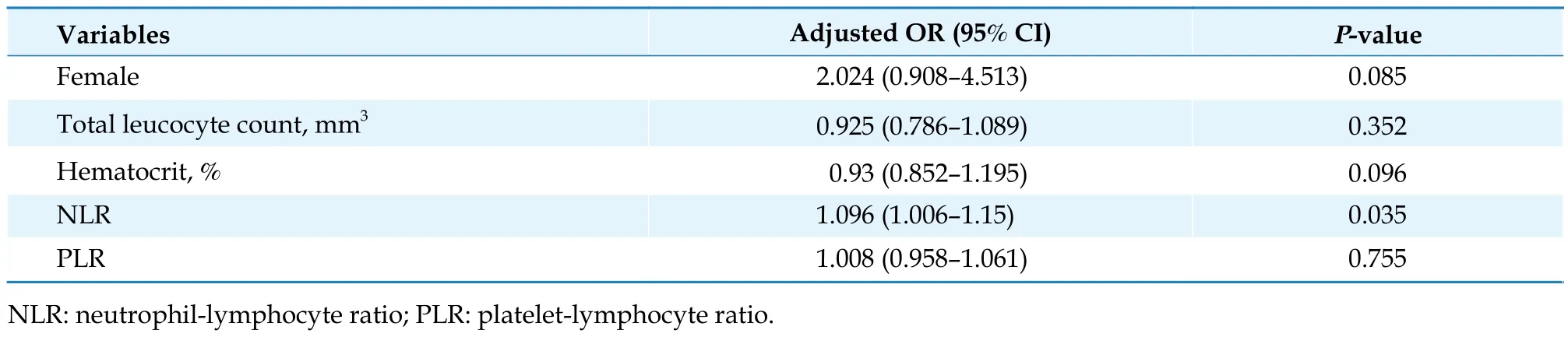
Table 5 Multivariate logistic regression analysis.
DISCUSSION
Based on the results of this study,a higher NLR ratio was associated with higher 30-day mortality in elderly patients with ACS.The NLR of elderly patients with ACS who died was higher than that of those who survived.On multivariable analysis,this was also established as an independent predictor of 30-day mortality in elderly patients with ACS.Furthermore,on univariate analysis,the female sex,a lower hematocrit,and a lower total leucocyte count at admission were associated with an increased risk of mortality.
A hemogram is available to all patients who visit the emergency department of any hospital.A routine hemogram contains many parameters that have been studied to assess factors in the prediction of mortality in ACS,such as NLR and white blood cell (WBC).[10,11]Most of these studies had a small number of elderly patients.The current study sought to investigate these haematological parameters only in this age group (age > 60 years).In addition,we determined the NLR cut-off value in a larger patient cohort.In our cohort,a higher NLR was associated with a higher likelihood of predicting mortality.NLR can be calculated simply by dividing the neutrophil count by the lymphocyte count in a differential WBC sample.It is one of the most well-studied haematological biomarkers in ACS,providing prognostic and diagnostic information.The combination of neutrophil and lymphocyte parameters outperforms each parameter separately in terms of prognosis.Tamhane,et al.[12]described the admission NLR as a predictor of in-hospital and 6-month mortality in patients undergoing PCI.NLR is useful in predicting short-and long-term mortality in NSTEMI patients with an NLR of more than 4.7.[13]
According to Sahin,et al.,[14]NLR is also related to the severity of CAD in STEMI patients.The NLR of the high SYNTAX score group was higher than that of the low SYNTAX score group (P< 0.001).NLR was found to be a predictor of all-cause mortality and cardiovascular events in patients undergoing angiography or cardiac revascularization in one of the meta-analyses.[15]In patients with acute inferior STEMI and stent thrombosis,NLR is also an independent predictor of right ventricular dysfunction.[16,17]
The link between atherosclerosis and inflammation is not new and has been extensively researched.[18,19]Atherosclerosis is primarily caused by inflammation,which also plays a significant role in plaque rupture,the development of an acute coronary event,and the size of the infarct and subsequent fibrosis.[20,21]
9月底至10月中旬,每亩茶园施腐熟饼肥100~150公斤或商品畜禽粪有机肥150~200公斤+38%茶树专用肥(氮-五氧化二磷-氧化钾=18-8-12或相近配方)30公斤,有机肥和专用肥拌匀后开沟15~20厘米或结合深耕施用。
Due to their effect on the instability of atherosclerotic plaques,leukocytes play an important role in the pathophysiology of ACS.Leukocytes permeate endothelial cells and become activated when they reach the tunica intima,causing the formation of microvascularity and,as a result,making plaques more prone to rupture.[22]Many studies have linked leukocytosis to an increased risk of cardiovascular disease.Chia,et al.[23]discovered that elevated leucocytes and neutrophils are predictors of adverse cardiac events in 363 STEMI patients in a prospective study.
Polymorphonuclear cell accumulation in the coronary culprit lesion site thrombus is an independent predictor of mortality in patients with ACS,according to Distelmaier,et al.[24]At the site of the culprit lesion,polymorphonuclear cell release neutrophil extracellular traps.Neutrophil extracellular traps are prothrombotic and proinflammatory fibres that can entrap leucocytes and spread thrombosis.[24]Lymphocytes,particularly B cells and T helpers,as components of the adaptive immune system,on the other hand,can mute and limit inflammation.Lower lymphocyte counts were linked to atherosclerosis progression and poor outcomes in ACS patients.[25,26]
Platelets are important in the pathophysiology of ACS.Platelets,when combined with fibrin,form a coronary thrombus.According to the CADILLAC study,platelet levels (which do not affect the effectiveness of percutaneous interventions) are significantly correlated with the incidence of restenosis and stent thrombosis.[27,28]There was no statistically significant difference in platelet levels between patients who died and/or survived in our study.The PLR is an important metric for describing the systemic inflammatory response.PLR has been identified as a risk factor for all-cause mortality following NSTEMI.In patients with ACS,PLR at admission is significantly related to the severity of coronary atherosclerosis.[29,7]In addition,a higher PLR is linked to recurrent MI,heart failure,ischemic stroke,and all-cause mortality in patients with STEMI.[30]In our study,PLR between survivors and those who died was not significant in multivariate analysis.
On multivariate analysis,NLR and PLR were found to be independent predictors of the Global Registry of Acute Coronary Events (GRACE) score in STEMI patients.[31]On multivariate analysis,our study found that only NLR was an independent predictor of short-term mortality (30 days) in elderly patients.
LIMITATIONS
Our study had a few disadvantages,including being a single center study,having a limited sample size for the disease’s prevalence in the region,having a preponderance of male patients,and focusing solely on interventional care.
CONCLUSIONS
Inflammatory processes are crucial in the onset of atherosclerosis,destabilisation of atherosclerotic plaques,and formation of clots on the plaque surface.In elderly individuals with ACS,NLR and PLR both predict 30-day mortality.For the risk classification of all elderly ACS patients,we highly advise using NLR rather than the total WBC count.It serves as a key instrument for intra-hospital clinical surveillance.However,more research is needed on these hematological indicators.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
猜你喜欢
杂志排行
Journal of Geriatric Cardiology的其它文章
- Prolonging dual antiplatelet therapy improves the long-term prognosis in patients with diabetes mellitus undergoing complex percutaneous coronary intervention
- Development and validation of a score predicting mortality for older patients with mitral regurgitation
- Age-related outcomes in patients with cardiogenic shock stratified by etiology
- Transcatheter aortic valve implantation in a patient with anomalous right coronary artery originating from the left aortic sinus with interarterial course
- The first experience of multi-gripper robot assisted percutaneous coronary intervention in complex coronary lesions
- Feasibility of emergent transcatheter aortic valve replacement sequentially followed by cardiac computed tomography angiography: experience from the procedure
