Current evidence on the use of near-infrared spectroscopy for postoperative free flap monitoring: A systematic review
2023-01-13HaoZheBianChongHanPekJolieHwee
Hao Zhe Bian ,Chong Han Pek ,Jolie Hwee
a Lee Kong Chian School of Medicine,Nanyang Technological University,Singapore 308232
b Department of Plastic,Reconstructive and Aesthetic Surgery,Khoo Teck Puat Hospital,Singapore 768828
Keywords:Free flap Flap monitoring Near-infrared spectroscopy Systematic review
ABSTRACT Background: Although the surgical outcomes of free flap reconstruction have improved over time,vascular compromise remains a devastating complication.Near-infrared spectroscopy (NIRS) is a promising new free flap monitoring technique with the potential for better outcomes than clinical monitoring (CM).This systematic review aims to provide a comprehensive review of the current evidence regarding the use of NIRS for free flap monitoring.Methods:A systematic literature review was performed,according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines,on existing NRIS studies,including the clinical outcomes of NIRS monitoring,speed of detection,diagnostic accuracy,variables affecting NIRS accuracy,and cost-effectiveness.Results: A total of 24 articles were included in this analysis.In most instances of flap compromise,NIRS enabled earlier detection of compromise than did CM,by an average of 8.1 (0.5-32.0) h.The flap salvage rate of flaps monitored with CM and NIRS (87.2%) was significantly higher than that of flaps monitored with CM alone(50.0%)(P<0.01).The overall survival rate for flaps monitored with CM and NIRS(98.1%)was also significantly higher than that for flaps monitored with CM alone (96.3%) (P=0.02).Blood oxygen saturation was the only variable with a significant effect on NIRS results.Conclusion: NIRS is an objective and reliable flap monitoring technique that provides superior flap salvage and survival rates compared with CM,which translates to cost savings and a reduction in workload for healthcare staff.Further large-scale studies are needed to standardize flap compromise criterion values and efficacy for different flap types.
1.Introduction
Since the first successful free tissue transfer surgery over 50 years ago,1the use of free flap reconstruction has evolved;it is now a routine intervention in the field of reconstructive surgery.2Flap survival rates have greatly improved over time with advancements in surgical techniques.3However,flap failure due to vascular compromise remains a devastating complication that can increase patient morbidity and prolong hospital stay.4Studies have shown that early detection of flap compromise and timely intervention result in higher salvage rates and better outcomes.5-7A robust and effective flap monitoring protocol is imperative in improving flap survival rates and clinical outcomes.
In 1975,Creech and Miller outlined the characteristics of the optimal free flap monitoring technique: harmless to the patient and free flap,accurate and reliable,rapidly responsive,inexpensive,and applicable to all flap types.8Conventionally,the standard flap monitoring technique has been bedside clinical assessment of flap color,capillary refill,skin turgor,temperature,pinprick,and hand-held Doppler readings.Over the years,various methods of flap monitoring have been developed and attempted,such as near-infrared spectroscopy (NIRS),implantable Doppler,multispectral imaging,and others.9Although these technologies are available,clinical monitoring(CM)remains the gold standard for flap monitoring.10However,there are limitations to CM,such as variability in the clinical judgment of different physicians or nurses.Smaller centers may also have insufficient trained staff to perform close monitoring.The ongoing COVID-19 pandemic is likely to further exacerbate this issue.Therefore,there is a need for an alternative to CM for flap monitoring.Studies have previously reported that NIRS is a promising flap monitoring tool;however,there is sufficient data on its usage.11
NIRS is a relatively new monitoring technology,first described for postoperative flap monitoring in 1995,12that is gaining in popularity.It is a noninvasive method that monitors regional tissue oxygenation and perfusion based on the principle of reflectance spectrophotometry.NIRS provides real-time measurements of oxygenated,deoxygenated,and total hemoglobin concentrations.These measurements indirectly reflect the status of tissue perfusion.13Fig.1 shows a typical NIRS monitoring device.14The NIRS probe is attached to the free flap skin paddle and connected to a display monitor that shows regional tissue oxygenation levels(Fig.2).Conventionally used as an indirect measure of oxygen perfusion in the brain,NIRS has evolved over the years to have various uses,15including free flap monitoring.NIRS provides some advantages over CM,such as faster detection of vascular compromise16and continuous flap monitoring.

Fig. 1.Vioptix T.Ox Tissue Oximeter (Vioptix Inc.,Fremont,CA,USA) with sensor probe.

Fig. 2.Diagram illustrating NIRS monitoring of free flap.NIRS,near-infrared spectroscopy.
Currently,literature on NIRS for free flap monitoring is limited.Several pilot and cohort studies have been conducted;however,no randomized controlled trials have been completed to date.The existing sparse reviews have focused mainly on the impact of NIRS on flap salvage rates.17-19The number of cases has been limited,with only one study including breast flaps.18There are no data on factors that could impact NIRS reliability.This systematic review aimed to provide a more updated comprehensive overview of the current evidence surrounding the use of NIRS for free flap monitoring,including the clinical outcomes of NIRS compared to CM,and threshold values.We have also expanded our review to analyze variables affecting NIRS reliability and cost-effectiveness from the perspectives of both the patient and healthcare system,which are areas not extensively covered in previous reviews.
2.Methods
The reporting of the systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)2020 statement,a guideline for reporting systematic reviews.20
2.1.Literature search strategy
We conducted a comprehensive electronic literature search using PubMed (Medline),The Cochrane Central Register of Controlled Trials(CENTRAL),Embase,and Web of Science databases with the following search terms: “flap monitoring” AND (“tissue oxygen saturation” OR“tissue oximetry” OR “near-infrared spectroscopy” OR “NIRS”).Articles published from database inception to September 2021 were included.
2.2.Inclusion and exclusion criteria
Only articles published in English before September 2021 and containing original data relating to postoperative free flap monitoring using NIRS were included.Reviews,letters,comments,oral and poster presentations,conference abstracts,animal studies,and duplicate publications of previous studies were excluded.
2.3.Study selection and data extraction
The titles and abstracts of papers obtained from the primary search were screened by two independent reviewers.The two reviewers independently reviewed the full texts of potentially relevant papers and extracted data.Any differences in opinions were resolved by a third reviewer.The data obtained included the type of study,type of NIRS device used,total number of patients and flaps,flap types,flap monitoring methods,frequency of monitoring,threshold values to determine flap compromise on NIRS,complication rate(defined as events resulting in vascular compromise),causes of vascular compromise,speed of detection of flap compromise,flap salvage rate,number of false positives and negatives,overall flap survival rate,variables affecting NIRS reliability,and cost-effectiveness analysis of NIRS.
2.4.Methodological quality and risk of bias assessment
All selected studies,except one,21were assessed for methodological quality and risk of bias using the Newcastle-Ottawa Scale (NOS),a checklist developed to determine the quality of non-randomized studies in systematic reviews.22The NOS is scored based on three components:selection of study groups,comparability of study groups,and ascertainment of the outcome of interest.The studies were assessed and classified as high,moderate,or poor quality by two independent reviewers,and a third reviewer resolved any areas of disagreement.
2.5.Statistical analysis
Chi-squared tests were utilized to compare the clinical outcomes between flap monitoring using only CM and flap monitoring using CM and NIRS.Statistical significance was set atP<0.05.A pooled analysis was performed.Statistical analyses were performed using SPSS 28.0 (SPSS Inc.,Chicago,Illinois,USA).
3.Results
The initial literature review identified 378 non-duplicate citations,of which 206 were excluded after title and abstract screening.The reasons for exclusion are illustrated in Fig.3.Subsequently,the remaining 46 citations underwent full-text screening,and 24 papers were selected for data extraction and analysis (Fig.3).Sixteen papers were prospective cohort studies,seven were retrospective cohort studies,and one was a cost-effectiveness model study.

Fig. 3.PRISMA diagram of study selection process.
3.1.Newcastle-Ottawa Scale methodological quality and risk of bias
The methodological quality and risk of bias of the studies were assessed using the NOS for cohort studies.All studies assessed were deemed to be of at least moderate quality and suitable for data analysis.One study21was not included in this assessment as it was a cost-analysis study and not a cohort study.A summary of the scores of each study is presented in Table 1.
3.2.Near-infrared spectroscopy instruments and threshold values
A large variety of NIRS instruments and threshold values for the detection of flap compromise were utilized in the included studies(Table 2).Fourteen different NIRS devices were used in the selected studies,with the most commonly used device being the ViOptix T.Ox™Tissue Oximeter (ViOptix,Fremont,CA,USA).The instruments used wavelength measurements ranging from 568 nm to 880 nm.One study developed a novel wireless wearable device that measured tissue perfusion using NIRS.23
The threshold values for detection of vascular flap compromise varied across the included studies (Table 2).Most authors used a criterion similar to the one described by Keller et al.24:a drop rate in tissue oxygen saturation(StO2)of 20%or more per hour,lasting for more than 30 min.Only one study did not adopt a threshold criterion based on absolute StO2 value or rate of change of StO2 value: Akita et al.25developed a regional oxygen saturation index,defined as the ratio of regional StO2 of the flap to regional StO2 of the non-dissected control portion.The criterion for flap compromise was defined as a regional oxygen saturation index of 0.75 or lower.Five studies did not specify a threshold criterion for determining flap compromise.
3.3.Data synthesis
In total,3 529 free flap reconstructions were performed in 2 529 patients.Overall,433 free flaps underwent flap surveillance via CM only(CM-only group),whereas 3 096 free flaps underwent CM with adjunctive NIRS monitoring (CM and NIRS group).However,no study examined NIRS as the sole modality for postoperative flap monitoring.
The most common flap type was the deep inferior epigastric perforator (DIEP) flap (n=3 031,85.9%),followed by the free fibular flap(FFF) (n=136,3.9%),superior gluteal artery perforator (SGAP) flap(n=92,2.6%),and anterolateral thigh(ALT)flap(n=85,2.4%).The free jejunal flap (n=23,0.67%) in the study by Yano et al.26was the only visceral flap-type monitored.A summary of individual study characteristics,including the number of free flaps,vascular complication rate,and mean time advantage in the detection of vascular compromise,is shown in Table 3.
3.4.Clinical outcomes
The clinical outcomes of each study are presented in Table 4.
3.4.1.Speed of detection of vascular compromise
From 23 papers that compared outcomes between CM-only and CM and NIRS,nine studies found that all instances of vascular compromise were detected using NIRS before the onset of any clinical signs and features.In three studies,more than half the total vascular events were detected earlier using NIRS.27-29Six studies did not comment on the difference in timing of detection of flap compromise between CM and NIRS,and the remaining studies did not encounter any flap vascular complications.Four papers reported the time difference in the detection of flap compromise with NIRS compared to CM.30-33Across the four studies,clinical signs of flap compromise lagged from 0.5 h to 32 h after NIRS indicated that a problem had occurred(Table 3).
3.4.2.Diagnostic accuracy
The diagnostic accuracy of NIRS was also analyzed.In the CM and NIRS group,four cases of false positives were reported out of 3 096 free flaps: two (3.5%) by Takasu et al.,33one (0.2%) by Koolen et al.,34and one (0.1%) by Ricci et al.28There were six cases of false negatives reported:one(10%)by Whitaker et al.,27one(0.2%)by Koolen et al.,34one(0.1%) by Ricci et al.,28and three (4.8%) by Ouyang et al.35The specificity values of NIRS for postoperative flap monitoring for all studies were above 95%,and sensitivity values were above 96%,except for the studies by Whitaker et al.27and Ouyang et al.35that reported sensitivity values ranging from 50%to 66.7%(Table 4).
3.4.3.Flap salvage and overallflap survival rate
Flaps were removed either when the NIRS threshold for vascular compromise was reached or when clinical signs of flap compromise were observed.In the CM-only group,from 433 free flaps,vascular complications occurred in 31 flaps (7.2%),of which 30 were returned to the operating theatre (OT) for re-exploration.Of the flaps that were reexplored,15 (50%) were successfully salvaged.In the CM and NIRS groups,of 3 096 flaps,vascular complications occurred in 155 flaps(5%),with 133 being returned to the OT.Of the flaps taken back,116 were successfully salvaged,resulting in a flap salvage rate of 87.2%(Table 5).There were no significant differences in the rates of vascular compromise(χ2,P=0.060) or re-exploration (χ2,P=0.090) between the two groups.However,the flap salvage rates in the CM and NIRS group were significantly higher than those in the CM-only group(χ2,P<0.001).Overall flap survival rates were also significantly higher in the CM and NIRS group than those in the CM-only group(χ2,P=0.015).

Table 1 Newcastle-Ottawa Scale (NOS) risk of bias assessment for included studies.

Table 2 Overview of near-infrared spectroscopy (NIRS) devices and measurement parameters for each study.

Table 3 Summary of study details.

Table 3 (continued)
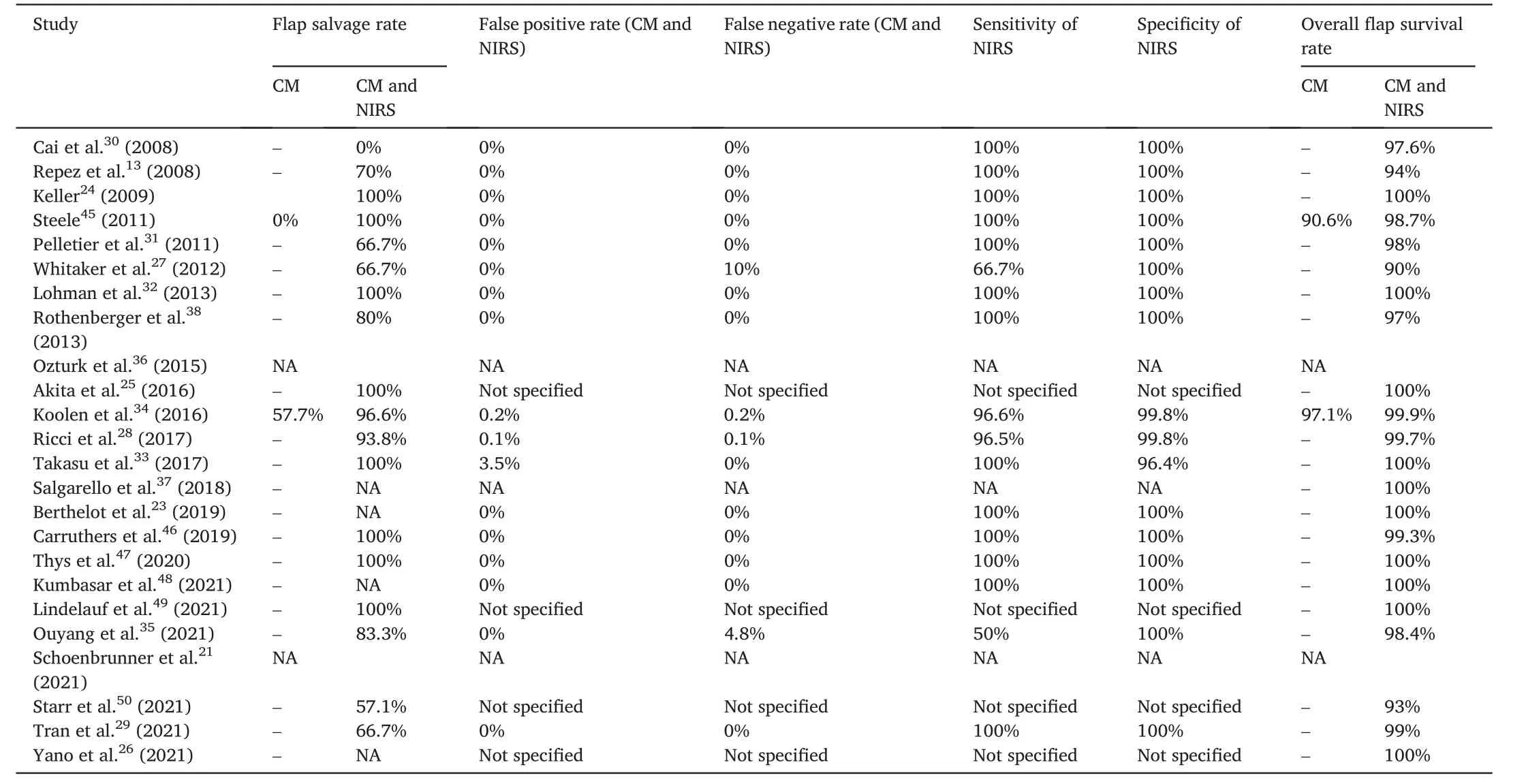
Table 4 Clinical outcomes of clinical monitoring (CM) and near-infrared spectroscopy (NIRS) monitoring.
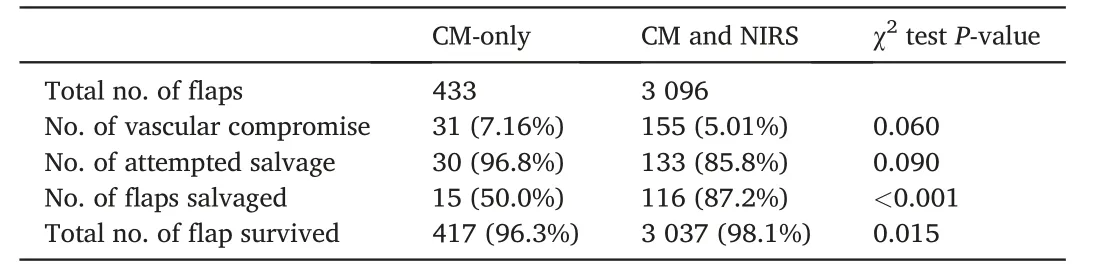
Table 5 Comparison of clinical outcomes between clinical monitoring(CM)-only and CM and near-infrared spectroscopy(NIRS).
3.5.Variables affecting near-infrared spectroscopy accuracy
Two studies investigated the variables affecting postoperative monitoring of flap regional StO2 using NIRS.36,37Ozturk et al.36carried out a prospective study to identify systemic and surgical factors impacting NIRS StO2 measurements in free flap breast reconstruction and showed that only blood oxygen saturation (SpO2) was significantly correlated with StO2,where an increase in SpO2 by 1% resulted in an increase inStO2 by 0.36%.Hence,factors that can cause hypoxemia,such as underlying chronic obstructive pulmonary disease,can result in variations in NIRS readings.In this study,supplemental oxygen,blood pressure,and surgical factors,including recipient vessel size,flap vessel size,perforator number,and perforator row,did not significantly affect StO2 readings.Salgarello et al.37conducted a retrospective study on postoperative monitoring of free DIEP flaps in breast reconstruction.Contrary to the findings of Ozturk et al.,a significant positive linear correlation was found between StO2 values and skin flap area,perforator number,and perforator size.A significant negative linear correlation was found between StO2 values and patient body mass index and flap size.
3.6.Cost-effectiveness of near-infrared spectroscopy monitoring
Three studies performed cost analysis of using NIRS for free flap monitoring.Repez et al.13reported that the cost of the InSpectra™Model 325 system (Hutchinson Technology,Hutchinson,MN,USA) was approximately €35 000 and disposable probe shields were €18 each.Rothenberger et al.38reported that the cost of the O2C system (LEA Medizintechnik,GieBen,Germany) was approximately €40 000,and Lohman et al.32reported that each ViOptix T.Ox sensor costs US$1 275.In some institutions,intensive care unit (ICU) monitoring for 24 h post-free flap is a standard practice.Two studies demonstrated a reduced need for postoperative ICU monitoring when NIRS was used for flap monitoring.When NIRS was used,Pelletier et al.31showed that postoperative surgical floor and ICU monitoring resulted in similar outcomes,translating to an average cost saving of US $1 937 per patient when monitored on the surgical floor.Ricci et al.28demonstrated that postoperative ICU monitoring with NIRS was cost-effective only for the first 15 h.Reducing the duration of ICU monitoring from the standard protocol of 24 h to 15 h would result in cost savings of US$1 666.70 per flap.Lastly,Schoenbrunner et al.21developed a model to analyze the cost-effectiveness of ViOptix T.Ox™for free flap monitoring in breast reconstruction;one way sensitivity analysis revealed that CM with adjunctive NIRS monitoring was cost-effective when the cost of each ViOptix probe to patients was less than US $1 487.
4.Discussion
Although clinical monitoring is the gold standard for postoperative flap monitoring,trained clinicians or nurses are required to provide round-the-clock monitoring.Even among trained healthcare professionals,the ability to reliably detect the clinical signs of vascular compromise is subject to individual experience.Emerging adjunctive modalities,such as NIRS,which provide continuous monitoring,are primed to change the paradigm of flap monitoring,especially during crisis periods,such as the COVID-19 pandemic,where there is a significant strain on manpower.
This review showed that adjunctive NIRS monitoring is reliable and superior to CM alone in detecting vascular complications.Both flap salvage rates(87.2%vs.50.0%)and overall flap survival rates in the CM and NIRS group(98.1%vs.96.3%)were significantly higher than those in the CM-only group,with minimal instances of false positives and negatives.This result is attributed to the ability of NIRS to provide continuous surveillance and detect vascular compromise earlier than clinical signs occur;one study quantified the earlier detection by NIRS to be 0.5-2.3 h before that of CM.32NIRS also serves as an objective quantitative measure that standardizes bedside assessment of flaps.As such,any patient care team member,regardless of clinical experience,can readily identify potential flap compromises and escalate to the attending surgeon.In addition,remote monitoring of flaps is possible using NIRS.From a questionnaire sent to members of the American Society for Reconstructive Microsurgery,results show that surgeons were significantly more likely to opt for an immediate return to the operating theatre for a concerning tissue oximetry reading than an abnormal Doppler signal from CM,suggesting that tissue oximetry may have a greater impact on clinical decision making in the postoperative period.39Some NIRS models,such as the TOS-OR(Fujita Medical Instruments,Co,Ltd,Tokyo,Japan),can also be used to monitor buried flaps such as jejunal flaps,as seen in the study by Yano et al.26
NIRS is a promising tool;however,it has limitations.First,some studies have found that NIRS is susceptible to multiple external factors.The values of regional tissue oxygen saturation have been reported to not only be affected by systemic oxygen saturation but also vary among individuals and even on different parts of the same flap.36,37Other issues raised by NIRS include the effect of ambient light on the NIRS device and the ease of dislodging the NIRS sensor.Berthelot et al.23developed a novel wireless NIRS device that addresses these two problems.This device is attached to a patient with adherent skin tape and covered with an opaque case to reduce the effect of ambient light.The use of NIRS in flaps with no skin paddle,such as muscle flaps,intra-oral or buried flaps,is also limited.
Second,there are concerns about false positives causing frequent alarms,which may induce unnecessary stress in patients and increase the workload for staff to verify the validity of alerts.However,in our review,there were minimal false positives and negatives,except for two studies.27,35In the study by Whitaker et al.,27the lower sensitivity value(66.7%) could be attributed to the small sample size,as only ten flaps were included.In the paper by Ouyang et al.,35the authors acknowledge that there is a limitation in the detection depth of their NIRS device(TSAH-100),which may result in a normal blood flow reading on the device despite the onset of flap compromise in obese patients or those with significant postoperative swelling.
Third,there are also concerns about the possibility of the NIRS device affecting the postoperative mobilization of patients;however,some devices allow the probes to be temporarily disconnected.Moreover,NIRS is only used immediately after free flap reconstruction,when mobilization is usually limited.
A fourth constraint of NIRS monitoring is the lack of consensus regarding the NIRS threshold values for flap compromise.Most studies used a criterion threshold based on absolute StO2 value or rate of change of StO2 value,adopted from Keller et al.24The criterion threshold developed by Akita et al.25is the only one based on the ratio of the StO2 value of the flap to the value of a control portion of the body.These are the only two studies that have developed their own criterion threshold and investigated the efficacy of their criteria.Further studies are required to establish a standard criterion threshold that can be validated for use across different NIRS devices and flap types.
And the fifth commonly cited limitation of NIRS monitoring is its high cost.The cost of NIRS devices varies across brands.Some NIRS systems can cost between €35 000 and €40 000,13,38and each ViOptix T.Ox™sensor costs between US$650 and US$1 275.32All current cost analyses of NIRS monitoring were performed from the patient’s perspective.Two studies reported cost savings from a reduction in the duration of postoperative ICU monitoring required with adjunctive NIRS monitoring.28,31However,these cost savings only apply to institutions with a current protocol for postoperative ICU monitoring,which is not the case for all institutions in the included studies.A cost-effectiveness model by Schoenbrunner et al.21showed that using CM with adjunctive NIRS monitoring will be cost-effective if the cost of a probe is lower than US $1 487.However,these cost analyses did not consider the value of time spent by the surgeon or experienced staff performing round-the-clock clinical monitoring or lower overall healthcare costs conferred from the higher flap salvage rates using NIRS,as shown in these studies.Fischer et al.40reported additional costs of US $9 000 for each free flap loss incurred to healthcare institutions and an extended hospital stay of two days for patients with flap loss.A higher flap salvage rate will thus help alleviate these costs to the healthcare system and provide indirect cost savings by reducing additional healthcare resources such as hospital beds for patients with flap loss.
Other existing adjunctive free flap monitoring techniques include implantable Doppler probes,color duplex sonography,and microdialysis techniques.11NIRS has some advantages over these techniques.NIRS is a noninvasive technique,and when compared to implantable Doppler,it has a much lower risk of disturbing the vascular anastomoses.NIRS also requires a lower level of technical expertise to operate and interpret results compared to color duplex sonography,which requires detailed knowledge of the flap and recipient sites.41Indocyanine green (ICG) angiography is another monitoring technique that makes use of near-infrared imaging.It is more commonly used intraoperatively to determine flap perfusion but has a lower sensitivity for detecting flap compromise postoperatively compared to CM.42Compared with NIRS,ICG angiography is a more invasive technique as it involves injecting the ICG dye intravenously,and it may cause adverse reactions in patients with dye allergies.43Another advantage of NIRS over ICG angiography is the ability to provide continuous flap monitoring.Recent developments have introduced a remote alert system where a text message is sent to staff when the NIRS threshold for flap compromise has been breached.44This system will positively augment any current monitoring system and may lessen or even entirely remove the need for routine physical checks.Repez et al.13also showed that NIRS can differentiate between arterial and venous causes of flap compromise.
This review has several limitations.At present,there is a lack of highlevel evidence,such as randomized controlled trials,and studies comparing NIRS as a sole monitoring method.Most studies only studied breast flaps,and the large variety of NIRS devices used resulted in high heterogeneity across studies,making comparison and statistical analysis of data difficult.There was also a large difference in the number of free flaps between the CM-only(433)and CM and NIRS groups(3 096),which may have affected the accuracy of the results.Publication bias may also exist when studies with positive results are more likely to be published.Lastly,there may be confounders,such as flap size and weight,patient chronic medications,and underlying diseases,that may affect the results of this review.However,these factors could not be analyzed in this review as most studies did not include sufficient data relating to these factors.
NIRS has changed the practice of flap monitoring at our institution.For close to a year,we have adopted the use of NIRS for postoperative monitoring of free flaps for up to five postoperative days.The use of NIRS for flap monitoring functions as an effective warning system for vascular complications that can be readily learned by nurses,who can subsequently keep surgeons informed.It also significantly reduces the workload burden on the on-call team and confers a degree of confidence in trainees who monitor the flaps.
5.Conclusion
This study provides a comprehensive review of many aspects of using NIRS for postoperative flap monitoring and shows that NIRS is a reliable and effective monitoring technique that can objectively supplement clinical assessment.It is a straightforward tool to detect impending or current flap failure before the onset of any clinical features and results in a significantly higher flap salvage and survival rate than CM alone.However,future large-scale studies are required to establish a more robust threshold criterion for flap compromise and efficacy in other flap types.There is significant potential for newer developments and further research into NIRS technology to definitively establish its reliability as a tool for free flap monitoring that can improve patient care,reduce healthcare costs,and possibly eliminate the need for intensive round-theclock clinical surveillance in the future.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented for the publication.
Authors’ contributions
Bian HZ: Data collection,Data analysis and interpretation,Writing-Original draft.Pek CH: Project supervision,Writing-Review and editing.Hwee J: Conceptualization,Data analysis and interpretation,Writing-Review and editing.
Competing interests
The authors declare that they have no competing interests.
杂志排行
Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Rhinoplasty in China: A review of the most important events in its history of development
- A combined therapy for the repair of alar defects that consists of a modified spiral flap and postoperative nasal stent
- DeepPurpose-based drug discovery in chondrosarcoma
- Micropunch grafting for healing of refractory chronic venous leg ulcers
- Oral health-related quality of life between Chinese and American orthodontic patients: A two-center cross-sectional study
- A rare post-coronavirus disease 2019 complication of maxillary mucormycotic osteomyelitis in a Southeast Asian patient
