Micropunch grafting for healing of refractory chronic venous leg ulcers
2023-01-13AyMohmedSmyMostfAdElHlimAhmedHssnElSgh
Ay Mohmed Smy ,Mostf Ad El-Hlim ,Ahmed Hssn El-Sgh,*
a Department of Plastic and Reconstructive Surgery,Mansoura University Hospital,Mansoura 35516,Egypt
b Plastic Surgery Center,Faculty of Medicine,Mansoura University,Mansoura 35516,Egypt
Keywords:Venous ulcer Micropunch grafting
ABSTRACT Background:Chronic venous ulcers are a serious problem for both patients and physicians.The CEAP classification(clinical manifestations (C),etiologic factors (E),anatomic distribution of disease (A),and underlying pathophysiologic findings (P)) for chronic venous disorders (CVD) was developed in 1994.Published papers on CVD use all or part of the CEAP.Micropunch grafts,which are a variation of skin grafts,have been used with great success in plastic surgery for both esthetic and reconstructive purposes.This study aimed to assess the outcomes of micropunch grafting in the treatment of chronic refractory venous ulcers.Methods: Patients with chronic venous ulcers who did not respond to conservative treatment for more than 6 months were included in the study.All patients underwent ulcer coverage by micropunch skin grafts using a micrometer.The patients were discharged on the same day as the surgery.Micropunch skin grafts were manually counted per square centimeter intraoperatively and during follow-up using Dermlite Dermatoschope™II Pro HR.Patient satisfaction was assessed by using a questionnaire.Results: Twenty patients underwent the surgery.Most of the patients were middle-aged males.The ulcers were predominantly small-and medium-sized.The mean operation time was 167.00±86.01 min.After 6 months,the survival rate of the planted micrografts was 84%.Three ulcers had graft loss and two patients had an infection at the ulcer site,which was managed conservatively.The patients were followed-up for 14 months.Conclusion:Micropunch grafting is a useful and convenient method for the treatment of difficult venous ulcers and can be performed on an outpatient basis.
1.Introduction
Chronic ulcers are an enormous burden to both patients and health services.By definition,chronic ulcers are wounds that fail to heal in a timely manner(i.e.,more than 12 weeks period).Chronic ulcers are most frequently caused by venous insufficiency.1The worldwide incidence of venous ulcers is 0.5%-2%,which may increase to 4%in old age.2,3
In 1994,the American Venous Forum,an international ad hoc committee,introduced the CEAP classification.It is composed of two parts:a classification of chronic venous disease (CVD) and a scoring system for CVD severity.The classification was based on clinical manifestations(C),etiologic factors (E),anatomic distribution of the disease (A),and underlying pathophysiologic findings (P),or CEAP.4,5The common complications of venous ulcers are infection and contact dermatitis,cellulites,affection of bone,malignant transformation,and a higher rate of recurrence after treatment,with an annual incidence ranging between 26%and 69%.6-13
The standard therapy for chronic ulcers includes compression with debridement of the ulcer,when necessary.Cellular human skin equivalents or low-level laser therapy may promote rapid healing,particularly in patients with longstanding ulcers.14,15Ulcers sometimes fail to heal;in such cases,surgery is required to fill the wound and to prevent further tissue damage.The first line of surgical treatment is autografting,which includes full thickness,split thickness,autologous skin cell suspension,and micropunch graft.16Micropunch grafting is the simplest and least expensive grafting procedure for the treatment of chronic ulcers.17These techniques can be performed alone or combined with adjuvant modalities such as platelet-rich plasma,stem cells,and negative wound therapy.18-20In this study,we assessed the clinical results of micropunch grafting for the treatment of chronic refractory venous ulcers.
2.Methods
This single-center prospective case series study was conducted between June 2019 and December 2021.This study was approved by the Ethics Committee of our university (approval no.MS.19.04.579-2019/07/14).Informed consent was obtained from all patients or their legal guardians.
All patients with chronic venous ulcers that had not improved with conservative treatment for at least 6 months or were covered before by sheet skin grafts were included in the study (C6CEAP classification).21The lesion sizes were classified(Table 1).
Exclusion criteria included extreme age,other types of chronic ulcers rather than venous ulcers or ulcers with mixed etiology,suspected carcinoma,and patients with uncontrolled chronic diseases such as hepatic and renal diseases or diabetes mellitus.
2.1.Surgical technique
The thigh was selected as the donor site.Local anesthesia was used under complete aseptic conditions.The graft was harvested with a Cut-To-Size (Robbins Instruments,NJ 07928,USA) blades of 0.9-1 mm width loaded into the handpiece of a micro motor that works at 1 500-3 000 rpm.The depth of the blade was down to the dermis.The harvested micropunch skin grafts were manually collected using jeweler forceps (Fig.1).The ulcer was locally anesthetized and surgically excised until it reached the bleeding bed.Chambers were created to plant the grafts at intervals of 4 mm.The grafts were placed using the implantation jeweler forceps.Dressing of the donor area was either exposed by frequent application of ointment or closed using gauze dressing.The grafts were covered with nonadhesive dressings,antibiotic ointment,gauze,and compression bandages.The patients were discharged on the same day as the surgery.The dressing was removed on the second day postoperative.Dressing was then performed twice per week.
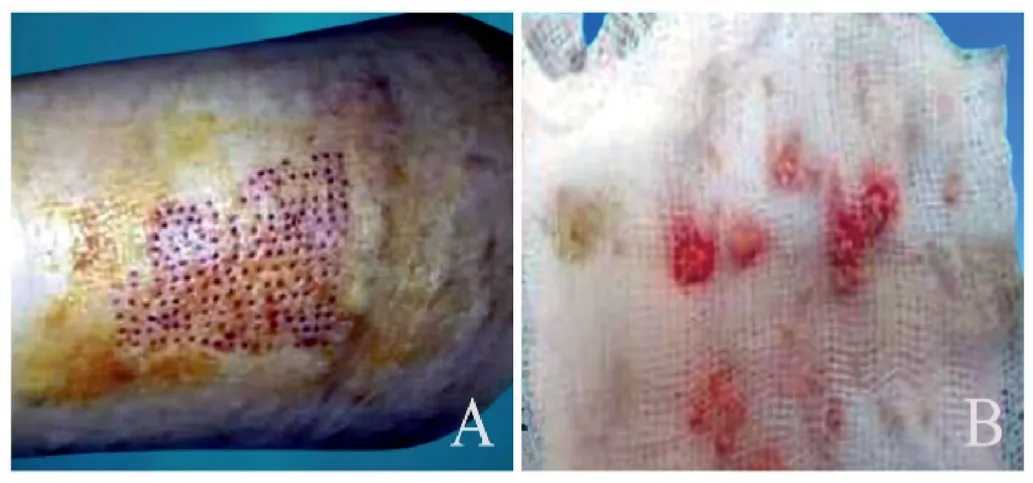
Fig. 1.Harvesting of micropunch graft.(A) Donor area.(B) Micropunch graft.

Fig. 2.(A)Preoperative two chronic venous ulcers at the anterior aspect of the lower end of the leg.(B) Postoperative after 1 week.(C) Postoperative after 14 months.

Fig. 3.(A) Preoperative chronic venous ulcer at the anterior aspect of the middle of the leg.(B) Postoperative after 10 days.(C) Postoperative after 7 months.
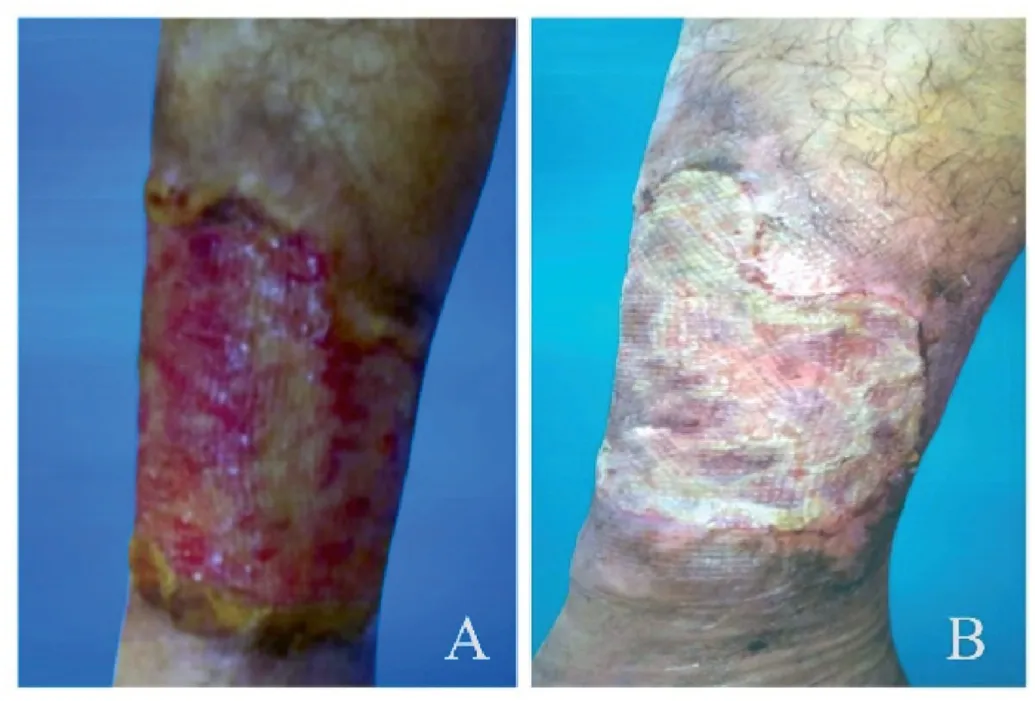
Fig. 4.(A) Preoperative big chronic venous ulcer at the anterior aspect of the lower end of the leg.(B) Postoperative after 5 months.

Fig. 5.(A) Preoperative recurrent venous ulcer after coverage with sheet skin graft on right leg.(B) Postoperative coverage with micropunch grafts after 6 months.
2.2.Postoperative measures
The transplanted micropunch skin grafts were manually counted per square centimeter using a Dermlite Dermatoschope™II Pro HR.This was done intraoperatively for comparison with counting during the follow-up period.Postoperative antibiotics,analgesics,and drugs were prescribed to all the patients.
2.3.Assessment of patient satisfaction
Measurement of patient’s degree of satisfaction was assessed according to a questionnaire ranging from 1 to 5,where 1 means totally agree up to 5,which means totally disagree.22The lowest score indicated a highly satisfied patient,whereas the highest score indicated a totally unsatisfied patient(Table 2).

Table 1 Classification of venous ulcers in leg.
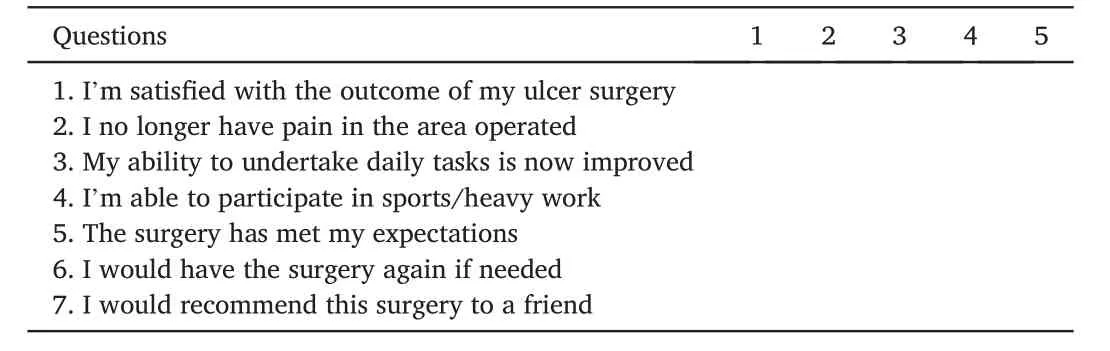
Table 2 Questionnaire of patient satisfaction.
2.4.Statistical analysis
The collected data were summarized as quantitative data in terms of range and mean±standard deviation.Qualitative data were expressed as percentages.ThePvalue(<0.05)was considered statistically significant,Pvalue (<0.001) was highly significant,andPvalue (>0.05) was insignificant.All statistical analyses were performed using STATA/SE version 11.2 for Windows (STATA Corporation,College Station,Texas,USA).
3.Results
A total of 20 patients(male,80%;median age,39.70±11.80 years;range,22-54 years)were included in the study.The mean time elapsed between disease onset and surgery was 2.40±1.52 years.A small lesion was present in 50%of the patients(10 cases).A medium-sized lesion was present in 30%of the patients(6 cases)and a large lesion was present in 20%of the cases(4 cases).
3.1.Clinical results
The mean operative time was 167.00 ± 86.01 min (range,70-360 min).On transplantation,the mean count of micropunch grafts was 29.05 ± 2.22 (extending from 24 to 32 micrografts per square centimeter).After 6 months follow up,the mean count of micropunch graft was 24.55 ± 2.49 (ranging from 20 to 28 micropunch grafts per square cm),showing an average survival rate 84.42%.Five patients were treated with micropunch skin grafts after failure of sheet skin graft use with complete survival.The mean follow-up period was 9.3 ± 3.21 months (extending from 4 to 14 months) (Figs.2-6).
3.2.Patient satisfaction
Of the patients,15% (3 patients) were highly satisfied,15% (3 patients)were satisfied,35%(7 patients)were moderately satisfied,20%(4 patients) showed mild satisfaction,and 15% (3 patients) were unsatisfied.
3.3.Complications
Fifteen percentage (3 cases) experienced one or more postoperative complications.Partial graft loss was the most common,which resulted in failure of ulcer healing (Fig.7).Other minor complications including infections,occurred in ten percentage (2 cases).The two infected cases were managed with systemic antibiotics according to culture and sensitivity tests and with daily dressing with antimicrobial cream.
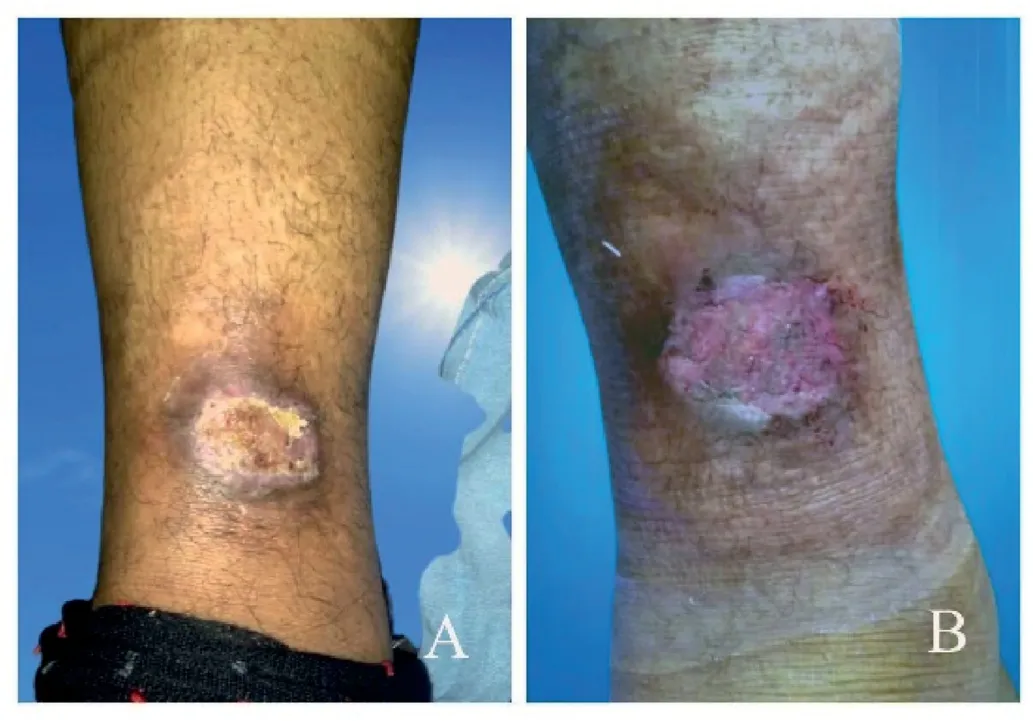
Fig. 6.(A) Preoperative recurrent venous ulcer after coverage with sheet skin graft on left leg.(B) Postoperative coverage with micropunch grafts after 4 months.

Fig. 7.(A) Preoperative big chronic venous ulcer at the anterior aspect of the leg.(B) Postoperative after 3 weeks.(C) Postoperative partial graft loss after two months.
4.Discussion
Refractory and large venous ulcers are two indications for skin grafting.23The use of skin grafts dates back to ancient Egypt and was described in the Ebert papyrus.24Skin grafts can be classified according to the geometry,source,and thickness of the graft.Micropunch skin grafting is a very common surgical technique used in plastic surgery for esthetic and reconstructive purposes.It was first reported by Reverdin in 1869 for the treatment of foot and leg ulcers and was reintroduced by Orentreich in 1972.24,25
The outcomes of punch grafts were superior in young individuals than in older ones.In old age,the skin loses its elasticity owing to decreased collagen content and becomes thinner and drier,making it is more vulnerable to infection and impaired wound healing.26In our study,age was not a factor affecting wound healing as most of our patients were middle aged.
Babu et al.reported that both male and female patients showed no difference in graft results.27However,others reported that females showed better results than males.This may be because androgens are negative regulators of the repair.In addition,estrogens and dehydroepiandrosterone accelerate wound healing by attenuating inflammation and promoting extracellular matrix deposition.28,29In this series,males were more dominant than females.Unlike Western societies,the number of men in our society exceeds the number of women.30
It was previously reported that micropunch grafting results were better in small-sized lesions than in large-sized ones.31This was not the case in our study.There were no significant differences in the outcome results between the ulcers of different sizes.This might be because the majority of lesions(80%)were small-and medium-sized ulcers.
In this study,we performed micropunch skin grafting in 20 patients,and good improvements were observed in 85%of the patients.Only 15%of the participants were unsatisfied.
The mean time elapsed between the onset of the disease and micropunch skin grafting intervention was 2.40±1.52 years.In a study of 284 ulcers managed with punch grafts,there were no significant differences in the graft results according to the latent period between the onset of the disease and the intervention.32
No complications occurred at the donor sites.Three patients had partial graft loss at the recipient site.
Two (10%) patients showed signs of postoperative infection at the ulcer site.The patients were managed conservatively.They showed moderate improvement with systemic antibiotic treatment and frequent dressings.Underlying diseases were the main cause of the disease.Lebanon et al.reported that post-grafting infection in chronic ulcer patients was due to the presence of bacterial load in the lesion bed before undergoing the operation.33
Punches less than 1.5 mm are a time-consuming procedure with the use of a manual punch,as the number of grafts required will be greater.In this study,the procedure became easier after using motorized power punches,as it offered the ability to harvest a larger number of grafts in less operative time (mean operative time,167.00 ± 86.01 min).In addition,it decreased the incidence of cobble stoning.
Interestingly,most of the micropunch grafting research has been published by dermatologic journals.Undoubtedly,micropunch grafting falls within the scope of plastic surgery.Therefore,plastic surgeons should be more interested in and expand the use of micropunch grafts.In this study,we used a micropunch graft for the coverage of recurrent venous ulcers after failure of sheet skin grafts in five patients with complete survival.We believe that using micropunch grafts has a better chance of survival than other types of skin grafts.For survival,micropunch grafts require a small blood supply to the ulcer bed compared with sheet skin grafts.
The limitations of our study were the small number of patients and the lack of histological examination to evaluate wound healing.Additionally,we used different types of skin grafts and compared their clinical outcomes.Sharing experiences with other centers would strengthen the study and increase its level of evidence.
5.Conclusion
Micropunch grafting using a motorized power punch successfully treated chronic venous ulcers.This is a convenient and low-cost surgical option.It can be performed on an outpatient basis,particularly in patients who are unlikely to tolerate hospitalization.
Ethics approval and consent to participate
This study received ethical approval from the Ethics Committee of the Mansoura University (approval no.MS.19.04.579-2019/07/14).The study conformed with the ethical standards set forth in the 1964Declaration of Helsinkiand its later amendments.All participants provided written informed consent prior to study enrollment.
Consent for publication
Informed consent was obtained from all patients for publication of the data contained within this study.
Authors’ contributions
Samy AM: Conceptualization,Methodology,Writing-Original draft.El-Halim MA: Methodology.El-Sabbagh AH: Methodology,Writing-Review and editing.
Competing interests
The authors declare that they have no competing interests.
杂志排行
Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Rhinoplasty in China: A review of the most important events in its history of development
- A combined therapy for the repair of alar defects that consists of a modified spiral flap and postoperative nasal stent
- DeepPurpose-based drug discovery in chondrosarcoma
- Oral health-related quality of life between Chinese and American orthodontic patients: A two-center cross-sectional study
- A rare post-coronavirus disease 2019 complication of maxillary mucormycotic osteomyelitis in a Southeast Asian patient
- Innovative combined therapy for multiple keloidal dermatofibromas of the chest wall: A novel case report
