A combined therapy for the repair of alar defects that consists of a modified spiral flap and postoperative nasal stent
2023-01-13YinminWngChengHungYouongNingRuiJinJunYngLinLuXusongLuo
Yinmin Wng ,Cheng Hung ,Youong Ning ,Rui Jin ,Jun Yng ,Lin Lu,* ,Xusong Luo,*
a Department of Plastic and Reconstructive Surgery,Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai 200011,China
b Department of Plastic Surgery,Shanghai General Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai 200080,China
c The First People’s Hospital of the Lancang Lahu Autonomous County,Puer 665699,Yunnan,China
Keywords:Nasal alar defects Flap transposition Spiral flap Nasal stent Nasal subunits
ABSTRACT Background: The repair of alar defects is challenging in clinics.Although skin grafts and nasolabial flaps are reliable,they can cause secondary post-surgical deformities.Methods: In this report,we describe an alar spiral advancement flap with a subcutaneous pedicle combined with postoperative nasal stent therapy for the repair of alar defects.Results:All cases showed slight asymmetry immediately after surgery,but at a median follow-up of 24 months,no cases of dissatisfaction with the nose shape or abnormal respiratory function were found.Almost all incision scars subsided within 12 months.In addition,all flaps that were dissected and rotated during the surgeries healed,and no signs of necrosis or development of vascular compromise were observed.Conclusion: Our preliminary experience suggests that the alar spiral flap followed by nasal stent therapy provides stable recovery of appearance and function for alar defects during follow-ups and shows promise for future therapies.
1.Introduction
The repair of alar defects,which include acquired alar defects and congenital alar rim clefts,is a challenge for plastic surgeons and dermatologists because of the aesthetic and functional considerations resulting from their location in the midface.1,2Various reconstructive approaches can be applied to repair alar defects.For instance,skin grafts can be used to cover defects that have intact cartilage and lining;however,the grafts may appear as patches with dissimilar colors and textures.3Local flaps,such as the bilobed flap from the lateral wall or the nasolabial flap,have been used for alar reconstruction.4However,the former may cause extra excisions of the dog-ear triangle between the defect and flap pivot point as well as high rates of obvious scarring and pincushion deformities.5In contrast,the latter may distort the nasolabial groove via the development of a trapdoor deformity.Therefore,improved methods to repair alar defects,including concealed incisions and similar skin colors and textures,are required for clinical application.
Here,we describe a novel method for repairing alar defects using a spiral flap and postoperative nasal stent.The goals of this study were to present a modified alar flap to repair alar defects within the same cosmetic subunit and identify its indications.
Descriptions of complex repairs via the use of composite tissue grafts from the ear or multi-surgery forehead flaps with cartilage transplants have been previously described and are beyond the scope of this article.6,7The techniques described here include the use of a local flap for alar repair within a single surgical session,and the post-surgical use of a nasal stent to prevent alar collapse or stenosis of the anterior naris.
2.Methods
2.1.Patient information
Five Asian patients aged between 21 and 56 years received a combined spiral flap and nasal stent therapy.The patient selection criteria were as follows: at least 18 years of age,single lesions within an alar subunit,and adequate tolerance to surgery and follow-up.The exclusioncriteria were lesions present beyond 50% of the alar area,lesions with cartilage or lining defects,and patients with vascular diseases or coagulation disorders.The lesion areas were between 16.2%and 43%of the alar area.Patient clinical information is summarized in Table 1.
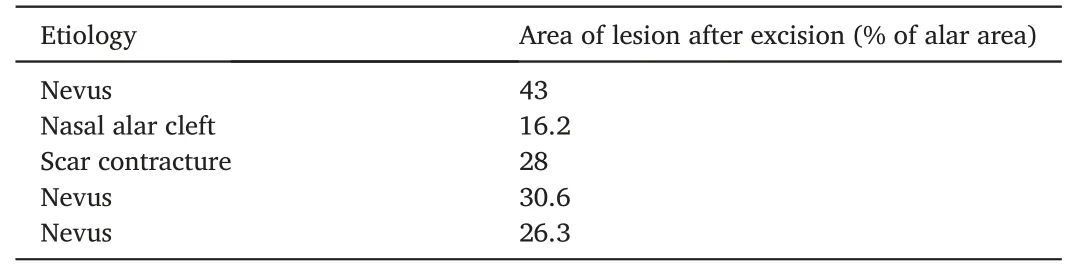
Table 1 Characteristics of lesions.
2.2.Surgical procedure and postoperative treatment
The design of the flap is described as follows: first,an incision was made along the alar groove,which can extend to the nostril rim if necessary,extending medially to the lesion.Ideally,the flap appeared as an arc around the defect.Extra skin was excised superior to the lesion along the nasofacial sulcus if needed.The distal end of the flap was dissected from the underlying subcutaneous tissue,while a myocutaneous pedicle was maintained over the proximal two-thirds of the flap to maintain sufficient blood supply.Superficial undermining was performed around the perimeter of the flap.The distal part of the flap was rotated to close the defect.Finally,the flap was anchored with minimal distortion of the alar-free margin(Fig.1).
To prevent nostril stenosis or collapse post-surgery,a custom-made silicone stent based on the contralateral nostril was printed using three-dimensional printing technology.The stents were worn for at least 3 months to maintain the size of the nasal passage(Fig.2).Furthermore,topical silicone gel was used in these patients to avoid hypertrophic scar formation.
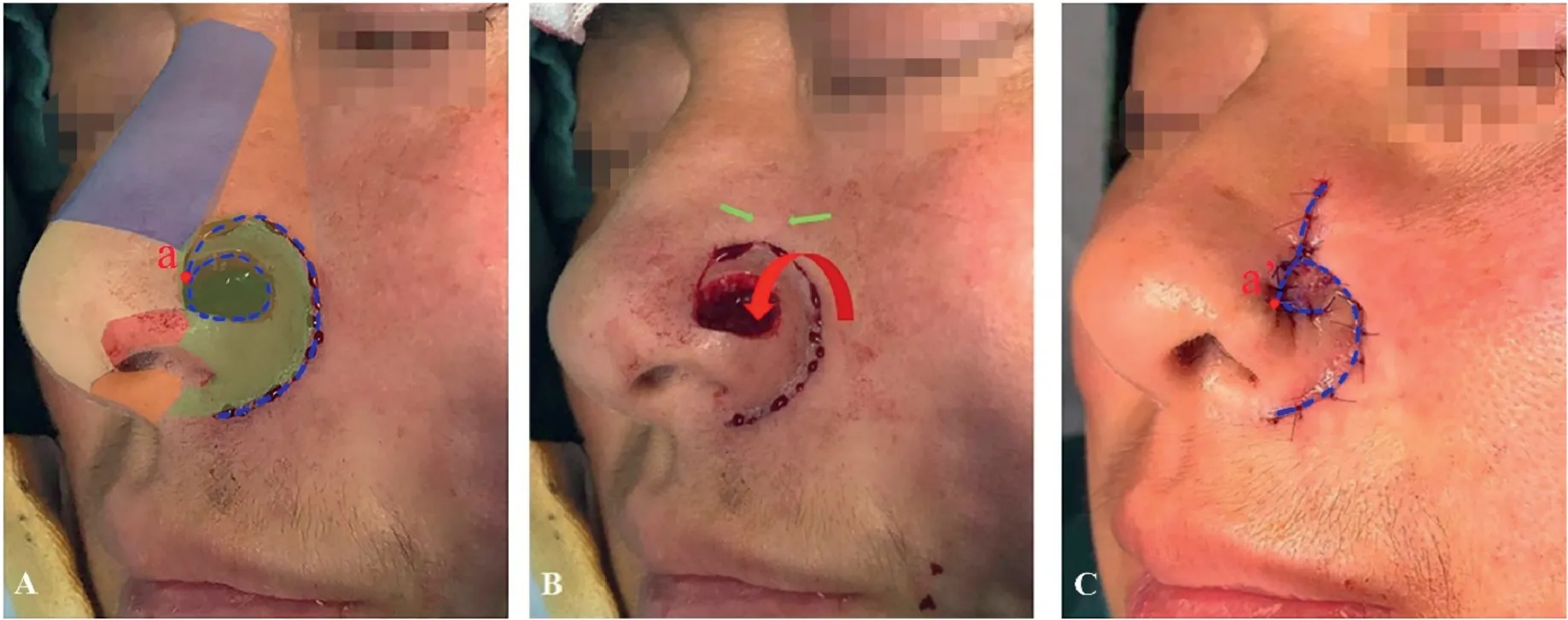
Fig. 1.(A)The alar defect following lesion excision and spiral incision.The schematic color blocks showing the subunits of the nose,and the green area represents the alar subunit.The blue dotted line represents the incision line.(B) The intraoperative photo of the spiral flap,and the red arrow shows the rotation of the flap.The green arrows show the close of secondary defect.(C)The immediate post-surgical appearance of the alar repair.The blue line shows the rotation of the flap.The tip of the flap is indicated by a red dot and a in Fig.1A,which is transferred to a’ in Fig.1B.

Fig. 2.(A) The model of wearable nasal stent used in this study.(B) The clinical application of the nasal stent in nasal alar repair.
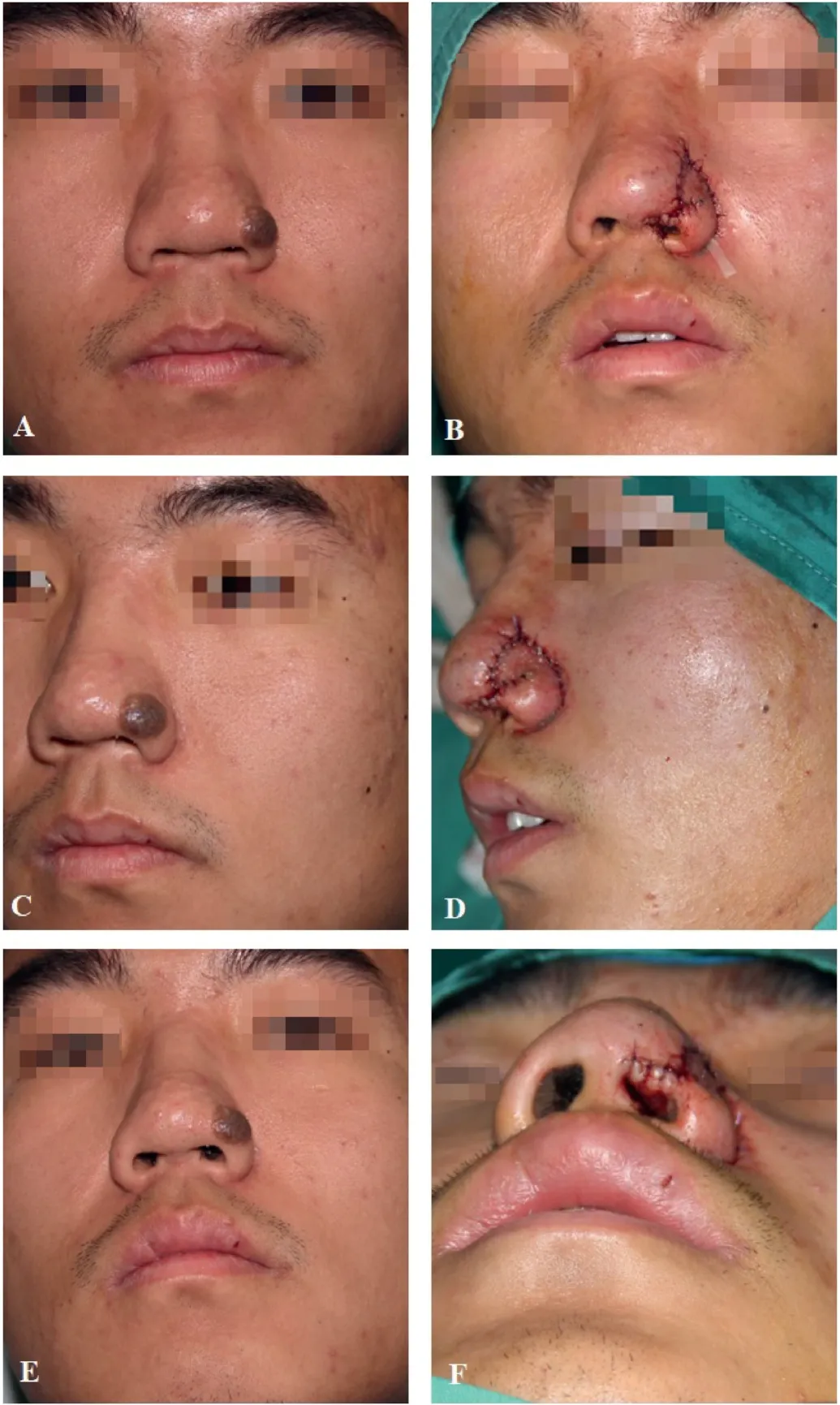
Fig. 3.A 26-year-old man with a congenital nevus on the nasal ala.(A) Preoperative front view of the patient.(B) Postoperative front view of the patient.(C) Preoperative side view of the patient.(D) Postoperative side view of the nevus postoperatively.(E) Preoperative base view of the patient.(F) Postoperative base view of the patient.
2.3.Pre-surgical and post-surgical evaluation
Images of the patients were analyzed using ImageJ (National Institutes of Health)to evaluate lesion areas following excision.Moreover,at a minimum,6-month follow-ups of the patients by professional plastic surgeons were carried out to evaluate the surgical effects and complications.Respiratory function,external nose shape,and scar formation were evaluated according to post-surgical patient self-reports.8The report adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
3.Results
At a median follow-up of 24 months,all the incisions healed without signs of necrosis.All cases showed slight asymmetry immediately after surgery but were relieved during follow-ups.Redness and swelling from scar formation were noticed in two of the cases,but subsided within 6-12 months post-operation.No cases of dissatisfaction regarding nose shape or abnormal respiratory function were reported during follow-up.Representative cases are described in detail below.
3.1.Typical case 1
A 26-year-old man presented with a lump in the nasal ala,near the nasal tip.According to the patient,the lump was congenital and had expanded with age.The lump measured approximately 1.4 cm×1.1 cm,was grey-black in color,and was without pain or pruritis.The decision to perform surgical excision was made after a consultation that considered the desire to avoid malignant changes and aesthetic concerns.Surgical treatment was conducted as described above.A nasal stent was applied within the first 6 months post-surgery.Post-surgical pathology indicated that the lump was a compound nevus(Fig.3).At the 6-month follow-up,the incision scar was slightly red,which subsided with mild hyperpigmentation at the 12-month follow-up.
3.2.Typical case 2
A 42-year-old woman presented with a lump in the nasal ala.The lump expanded with age,but was stable in recent years.The lesion was dome-shaped with short hair and was light brown in color.Surgical treatment was conducted as described above.A nasal stent was also applied.Postoperative pathology indicated a dermal-type melanocytic nevus.At the 6-month postoperative follow-up,the scar was not obvious and the symmetry of the alar structures was maintained (Fig.4).

Fig. 4.A 42-year-old woman had a lump on the nasal ala.(A) Preoperative side view of the patient.(B)Side view of the patient 6-month postoperatively.(C) Front view of the patient 6-month postoperatively.(D) Base view of the patient 6-month postoperatively.
4.Discussion
In this study,all patients recovered well after surgery.No acute complications,such as dehiscence,infection,or flap necrosis,were observed after surgery.Two patients exhibited redness from scar formation,which subsided within 12 months.All patients exhibited slight asymmetry immediately after surgery;however,this was mitigated following postoperative stent application.Furthermore,no signs of respiratory obstruction were observed in any of the patients.
The skin of the nasal area has different textures,depending on the subunit.For instance,the alar skin is thin but adherent,whereas the skin of the dorsum and sidewall is thin and mobile,and the tip is thick and stiff.To achieve aesthetic results,traditional nasolabial flaps need to be thinned before inset to the alar defect,which may increase the risk of vascular compromise,and obvious differences can still be noticed postsurgery.9Indeed,only the tissue in the alar or dorsal and sidewall subunits can achieve results with the same colors and textures as described in this study.Further,the nose has an aesthetic boundary,10which means that incisions along the subunit borders minimize scar formation.Incisions along the alar groove and nasofacial sulcus of the spiral flap can hide post-surgical scars at the border of the alar and sidewall subunits,which is particularly important for Asians,who have a tendency for hypertrophic scar formation.Moreover,the structure of the alar subunit is maintained to maximize aesthetic reconstruction of the nose shape.This surgical procedure improves the spiral flap as reported by Stoner et al.11by excluding nasolabial tissue transposition.Altogether,in this study,we applied an alar spiral flap to improve the outcomes of nasal alar defect repairs,a procedure especially suitable for Asians.
As the alar rim has no cartilage support,cartilage grafts are used to prevent nasal alar collapse or nostril stenosis in the traditional repair of alar defects.12In our study,a wearable nasal stent was used in patients that underwent flap reconstruction of alar defects.Wearable or implantable nasal stents have been previously reported to prevent nostril stenosis and even dilate congenital nostril stenosis.13,14Thus,nasal stents,to some extent,may bypass the need for cartilage transplantation and help maintain unobstructed nasal airways in patients with spiral flaps.Moreover,they help avoid scar contracture,which may cause acquired nostril stenosis in postoperative patients,especially within the first 6 months post-surgery.15
A limitation of our method is that it is ideal for small to medium-sized defects with intact cartilage and lining tissue within the alar subunit and sufficient tissue remaining around the alar groove.Defects that involve over 50% of the alar area may cause severe deformity of the nasal alar and cannot be prevented by wearing postoperative stents.Furthermore,due to the limited number of patients included in this study,complications of this method may be hidden,and additional work is required to fully validate our techniques.Regardless,we hope that the outcome of our treatment will inspire future efficient reconstructive methods for alar defects.
5.Conclusion
An alar spiral flap followed by nasal stent therapy for alar defects provides satisfactory functional and aesthetic outcomes in patients in this study.This combined therapy is promising for future clinical application of alar defect repair.
Ethics approval and consent to participate
The study received ethical approval from the Ethics Committee at the Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine(approval no.SH9H-2021-T242).All procedures performed in this study were in accordance with the 1964Helsinki Declarationand its later amendments.All participants provided written informed consent before study enrolment.
Consent for publication
Informed consent was obtained from all patients for publication of the data contained within this study.
Authors’ contributions
Luo X: Conceptualization,Methodology.Lu L: Conceptualization,Methodology.Yang J: Supervision.Jin R: Investigation,Data curation.Wang Y.Writing-Original draft.Huang C: Writing-Review and editing.Ning Y:Writing-Review and editing.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant nos.81701901 and 81801946),Natural Science Foundation of Shanghai Committee of Science and Technology (grant no.19ZR1430100),and Shanghai Municipal Key Clinical Specialty (grant no.shslczdzk00901).
杂志排行
Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Rhinoplasty in China: A review of the most important events in its history of development
- DeepPurpose-based drug discovery in chondrosarcoma
- Micropunch grafting for healing of refractory chronic venous leg ulcers
- Oral health-related quality of life between Chinese and American orthodontic patients: A two-center cross-sectional study
- A rare post-coronavirus disease 2019 complication of maxillary mucormycotic osteomyelitis in a Southeast Asian patient
- Innovative combined therapy for multiple keloidal dermatofibromas of the chest wall: A novel case report
