Value of 18F-FDG PET/CT in predicting EGFR mutation status and PD-L1 expression in non-small cell lung cancer
2022-11-02LIXueyanWANGDaweiYULijuanLINXiuyanGONGWeiPANDengCHENLu
LI Xue-yan, WANG Da-wei, YU Li-juan, LIN Xiu-yan, GONG Wei, PAN Deng, CHEN Lu
1. Medical Imaging Department, Hainan Cancer Hospital Medical Imaging Department, Haikou 570311, China
Keywords:PET/CT Non-small cell lung cancer EGFR PD-1/PD-L1
ABSTRACT Objective: To explore the relationship between multimodal imaging features and metabolic parameters derived from 18F-FDG PET/CT and the mutation status of epidermal growth factor receptor (EGFR) and the expression of programmed cell death ligand 1 (PD-L1) in non-small cell lung cancer (NSCLC), so as to provide objective evidence for clinical screening of targeted therapy and immunotherapy beneficiaries. Methods: Data of NSCLC patients who underwent 18F-FDG PET/CT scans, EGFR mutation and PD-L1 expression tests with confirmed pathological results were collected. The differences of PET/CT morphological characteristics and metabolic parameters between the EGFR mutation and the wild group, and between the PD-L1 expression positive and the negative group were analyzed. Univariate and multivariate logistic regression analyses were used to test the correlation between clinical and PET/CT parameters and EGFR mutation and PD-L1 expression status. Results: MTV(P=0.01)and TLG(P=0.00) values of EGFR mutant patients were statistically lower than those of wild type patients. Univariate and multivariate logistic analysis showed that age(P=0.03), smoking history(P=0.00) and MTV(P=0.00) were independent risk factors for EGFR mutation. The positive expression of PD-L1 in stage Ⅲ/Ⅳ group was significantly higher than that in stageⅠ/Ⅱ Group (P=0.01), but there was no significant difference in different age, gender, smoking history, SUVmax, MTV, TLG, LDH and CEA groups. Logistic univariate analysis showed that only stage was associated with the positive expression rate of PD-L1 (P=0.01). There was no significant correlation between PET/CT parameters and PD-L1 status. Conclusion: PET/CT metabolic parameters MTV, age and smoking history are independent predictors of EGFR mutation, which is expected to provide objective evidence for clinical screening of targeted treatment beneficiaries; however, PET/CT metabolic parameters are not good in predicting PD-L1 protein expression, which needs to be further verified by large sample.✉Corresponding author: WANG Da-wei, Associate Chief Physician, Bachelor of Medicine.
1. Introduction
Lung cancer is one of the most important public health problems in the world, and it is the malignant tumor with the highest risk of morbidity and mortality [1]. Non-small cell lung cancer (NSCLC)accounts for about 80% of all lung cancers [2]. The cell proliferation rate of NSCLC is usually slow, and the disease progression is not obvious. It is easy to miss the good opportunity for radical treatment after the onset of NSCLC. Statistics showed that about 75% of NSCLC patients were in the middle or advanced stage when they came to hospital, and the five-year survival rate was very poor [3].Despite the increasing diversification of lung cancer treatment methods, traditional cytotoxic chemotherapy is still the main means in the whole-course management of NSCLC patients, especially in adjuvant therapy. Therefore, it is important to find molecular markers that can predict the efficacy of chemotherapy and establish an effective prognostic model to noninvasively assess the survival of NSCLC patients. Screening the targeted population that may benefit from chemotherapy is an urgent problem to be solved.
PET metabolic radiomics not only integrates traditional medical imaging, genomics and clinical big data, but also integrates the basic concepts of radiomics and clinical diagnostic methods. The advantage of PET metabolic radiomics lies in the high dimensional information obtained by computer, which makes it possible to data the micro information in PET images on macro images. In this study,multi-modal18F-FDG PET/CT data were deeply mined by computer technology, which aimed to predict the chemotherapy sensitivity of advanced NSCLC, and to establish and screen a dominant prognostic model.
2. Materials and Methods
2.1 General Information
The study was conducted in our hospital from September 2017 to April 2021. A total of 146 patients with advanced NSCLC who underwent18F-FDG PET/CT examination were included in this study. The inclusion requirements were as follows: ① First diagnosis, bronchoscopic bite examination or fine-needle aspiration pathology confirmed NSCLC; ② Clinical stage Ⅲ or Ⅳ; ③ PET/CT examination and at least two cycles of chemotherapy were performed; ④PET/CT images were clear, and there were no other pulmonary diseases that might affect image analysis. ⑤No history of secondary primary tumor; ⑥ The case data are complete and traceable. The clinical data of the enrolled cases were reviewed,including age, gender, smoking status, pathological type, serum tumor markers, chemotherapy regimens and cycles, and whether or not they had received radiotherapy.The progression-free survival (PFS) of the patients were followed up. PFS was defined as the time between the start of initial treatment and the detection of progression, recurrence, or death from any cause on examination. All patients were followed up from the date of initial treatment until death or the cutoff date (April 20, 2022), with a median follow-up time of 8.6 months (range: 2.8 to 57.6) through our cloud platform medical record system or telephone follow-up.
2.2 PET/CT imaging and image parameters were collected
All subjects fasted for 4-6 hours before examination, and peripheral blood glucose (< 150md/dL was considered normal) was examined.GE Discovery 710 PET/CT instrument with imaging agent was used. 18F-FDG was prepared by GE Qilin cyclotron facility and chemical synthesis system with radiochemical purity exceeding 95%. The intravenous dose of 18F-FDG was 5.5-7.4 MBq/kg. After the injection, the subjects were instructed to rest for one hour before the whole body scan, image reconstruction, attenuation correction,and image fusion. The morphologic and metabolic parameters of lung cancer were collected using PET VCAR software. The morphological parameters mainly included size, location, density,adjacent bronchus, internal and marginal conditions of the mass.The metabolic parameters were as follows: Maximum standardized uptake value (SUVmax) of primary lesion, metabolic tumor volume of primary lesion and systemic tumor, MTV) and total lesion glycolysis (TLG; TLG= mean SUV(SUVmean)×MTV).The threshold values of 30% SUVmax, 40% SUVmax, and 50% SUVmax were used simultaneously to determine or calculate the MTV and TLG of primary lesion, while the threshold values of 40% SUVmax of primary lesion were used for whole body MTV (MTVwb) and whole body TLG (TLGwb),Figure 1.
2.3 VOI delineation and PET/CT omics feature extraction were performed
PET/CT images of all cases were exported to Lifex software(version 6.20), and the images were read and analyzed by two experienced nuclear medicine physicians. The Region of interest(ROI) of the lesions was delineated layer by layer in the PET images until the ROI covered all tumor sites. With 42 % SUVmax as the optimal threshold, the three-dimensional Volume of interest (VOI)was obtained semi-automatically, and the PET radiomics features of the primary lesions were extracted. ITK-SNAP 3.8 application software was used to delineate and extract the CT omics features.During the delineation of the ROI, the entire lesion should be completely included on the basis of avoiding the peripheral blood vessels and internal necrotic areas. The morphology, gray statistics,texture and wavelet features were extracted from the above VOI.
2.4 Omics feature screening and prognostic model construction
In order to avoid the overfitting of the omics model, the dimensionality of the omics features was reduced before the model was created. The method of Least absolute shrinkage and selection operator (LASSO) was used to screen the dominant features in the training group to create the omics model. The radiomics score(RS) of each case was obtained by weighting the above features with corresponding coefficients. In order to simulate the routine clinical decision-making process, the composite prediction model was formed by integrating the omics characteristics and the clinical parameters with predictive value after multivariate Cox regression.The performance of the model was evaluated by Receiver operating characteristic curve (ROC).
2.5 Statistical analysis

Figure 1 PET/CT images of typical lung adenocarcinoma patient
All cases were divided into high risk group and low risk group according to the median PFS. In the training group, rank-sum test was used to preliminarily analyze the radiomics characteristics with significant differences between the two groups. The machine learning technology of Support vector machine (SVM) was used to classify the best features selected by LASSO algorithm. Eighty percent of the data were randomly selected to training group, and the remaining 20% were used as validation group. The clinical prognostic models were analyzed by univariate and multivariate Cox proportional hazard regression models. ROC curve was used to calculate the AUC, sensitivity and specificity of the model. All test results were two-sided, and P < 0.05 was considered statistically significant. Python software and SPSS26.0 software were used to analyze the above data.
3. Results
3.1 General data of the enrolled patients
The median PFS of the enrolled patients was 7.1 months (range: 0.8 to 55.6 months). The patients were divided into two groups based on the boundary of 7.1 months. Those with PFS≥7.1 months were classified as low-risk group, and those with PFS < 7.1 months were classified as high-risk group. A total of 146 NSCLC patients were randomly divided into the training group (n=116) and the validation group (n=30) according to the ratio of 8:2.The age of 116 patients in the training group ranged from 31 to 79 years, with an average age of (58.6±9.7) years. The average age of the 30 patients in the test group was (58.2±10.7) years (range, 42-80 years).Chi-square test was used to verify that the distribution of baseline characteristics was basically balanced between the training group and the test group(χ2= 0.019-2.429, P= 0.144-1.000). The general information of all patients is shown in Table 1.

Table 1 Relationship between clinicopathological parameters and EGFR mutation status
3.2 Screening of radiomics features and creation of prognostic models
LIFEx 6.20 and ITK-SNAP 3.8 were used to delineate the tumor VOI, and then 1017 radiomics feature parameters were extracted from each primary lesion using Python. A total of 47 features were obtained by Wilcoxon rank sum test to select features with significant differences in the training group, including 6 PET features and 41 CT features. In order to prevent the overfitting of the omics model,LASSO algorithm was used to further reduce the dimensionality,and the best prediction parameters were selected by ten-fold cross test. Finally, a total of 4 omics features (2 PET features and 2 CT features) were selected, named Original_firstorder_90Percentile(OF90P), Wavelet-lhh_firstorder_90percentile (WLF90P), wavelETHHL_FIRSTORDER_10PERCENTIle (WHF10P) and NGLDM_Coarseness, The coefficients of the feature are -0.056, 0.048, -0.004,-0.074, respectively. The feature screening process of LASSO is shown in Figure 1. The RS of each patient was calculated using the following formula: RS=-0.056×OF90P+0.048×WLF90P-0.004×WHF10P-0.074×NGLDM_Coarseness. ROC results showed that the AUC of radiomics model in predicting NSCLC PFS was 0.746 in the training group and 0.622 in the validation group (Figure 3).

Figure 2 SUVmax, MTV, and TLG boxes in patients with EGFR mutant and wild-type NSCLC

Figure 3 ROC curves of SUVmax, MTV and TLG to predict NSCLC EGFR mutation status
3.3 Construction of clinical prognostic model and composite prognostic model
In this study, a total of 3 clinical imaging features related to PFS in NSCLC patients were included by COX multivariate analysis.They were pathological type [Hazard Ratio:0.596(95%CI:0.364-0.913), P=0.019], clinical stage [Hazard Ratio:0.626(95%CI:0.429-0.912), P=0.015] and MTV30[Hazard Ratio: 0.158 (95% CI: 0.044 0.573), P = 0.005) ].A composite predictive model for PFS was obtained by combining RS with clinical model. The ROC curve was used to compare the predictive ability of clinical model, radiomics model and composite model for PFS of NSCLC patients. The area under the ROC curve of the three models were 0.746, 0.753 and 0.716 respectively (Figure 3). The radiomics model had the highest diagnostic efficiency, whose sensitivity and specificity were 0.663 and 0.833, respectively (Table 2). Delong test showed that there was no significant difference in the predictive performance between the radiomics model and the composite model (Z=1.777, P=0.076) and the clinical model (Z=0.323,P=0.747).
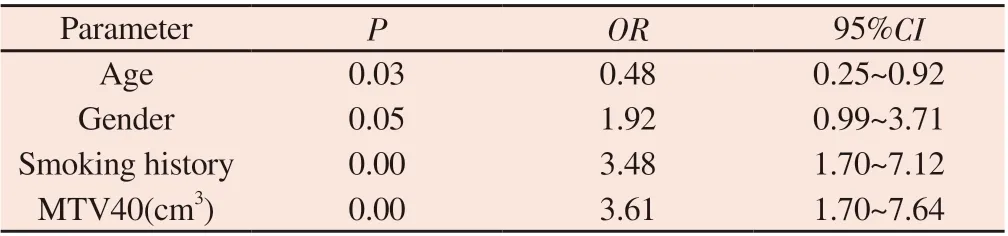
Table 2 Multifactorial analysis of EGFR mutation in 223 NSCLC patients
3.4 The relationship between clinicopathological characteristics, PET/CT metabolic parameters and the expression of PD ‑ L1 protein
The study group of correlation between PET/CT and PD - L1 protein expression finally enrolled 123 patients, including 79 males(64.23%) and 44 females (35.77%). The positive rate of PD - L1 was 65.85%, and the expression levels of 0, 1, 2 and 3 were 37.82%,27.91%, 26.25% and 8.02% respectively.The ROC curve analysis results showed that SUVmax, MTV and TLG predicted the cut - off values of PD - L1 protein expression status as 9.65 (AUC=0.47, 95%CI: 0.36~0.58, P=0.57), 24.15 cm3 (AUC=0.56, 95% CI: 0.45~0.66,P=0.03) and 71.25 g (AUC=0.52, 95% CI: 0.41~0.63, P=0.72),respectively (Figure 4). Mann - Whitney U test results showed that there was no statistically significant difference in SUVmax, MTV and TLG values between groups with different PD - L1 protein expression status (P>0.05) (Figure 5).Logistic single factor analysis was used to evaluate the relationship between clinical factors and PDL1 protein expression status, as shown in Table 3. The study found that the positive expression rate of PD - L1 in Phase III/IV group was higher than that in Phase I/II group (P=0.01), while age (P=0.33), sex (P=0.12), smoking history(P=0.65), SUVmax (P=0.47), MTV (P=0.37), TLG (P=0.12), LDH(P=0.27) and CEA (P=0.98) had no significant relationship with the protein status of PD - L1 (P>0.05) (Table 3).
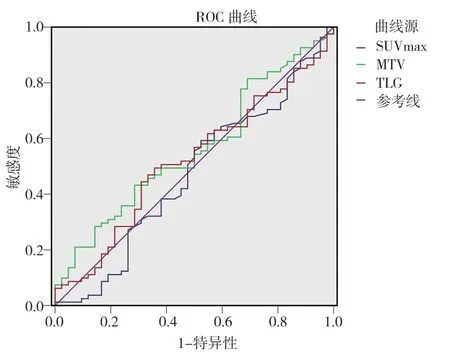
Figure 4 ROC curves of SUVmax, MTV and TLG to predict PD-L1 protein expression status

Table 3 Relationship between clinicopathological parameters and PD-L1 expression in 123 patients

Figure 5 SUVmax, MTV and TLG boxes of NSCLC patients in the positive and negative groups with PD-L1 expression
4. Discussion
Lung cancer is a malignant tumor that seriously endangers human life and health. There are many prognostic factors. How to construct an effective prognostic model to evaluate the survival of lung cancer patients and provide an objective basis for non-invasive precise treatment of lung cancer has important clinical significance.However, only a few biomarkers have shown clinical application potential among a large number of related biomarkers[4].Radiomics is a new and rapidly developing research method based on image feature analysis of computer technology. It has been gradually applied to the field of nuclear medicine since the beginning of this century, mainly to study the internal heterogeneity of tumors in PET images. A large number of studies have shown that PET/CT radiomics is more accurate than traditional CT and PET/CT visual evaluation in differentiating benign and malignant lung nodules, lung cancer pathological typing, gene mutation and molecular phenotype,showing more accurate diagnostic performance[5-8].
Studies on PET/CT radiomics technology in the prognosis of lung cancer have confirmed that both CT and PET imaging modes can obtain tumor prognostic omics characteristic parameters, and have certain predictive value for the prognosis assessment of lung cancer[9-13].Oikonomou [11] found that SUVmax alone could not effectively predict the overall survival of lung cancer patients after radiotherapy, but the predictive value was greatly improved after combining radiomics features. Director Zhao Xinming's team conducted radiomics analysis on 300 NSCLC patients in China,and constructed radiomics model, clinical prediction model and composite model combining the two. The results showed that the RS and composite model score of omics model were independent prognostic factors for overall survival of NSCLC patients[14].In our study, ROC curve was used to evaluate the efficacy of three prognostic models. The results showed that the radiomics model had the highest AUC (0.753) and the highest diagnostic efficacy. The model was verified in the validation process, and the area under the curve was 0.622, which was still satisfactory. In multivariate COX analysis of traditional clinical parameters, only pathological type,clinical stage and MTV30 were independent prognostic factors for PFS in NSCLC patients, while SUVmax and other thresholds corresponding to MTV and TLG were not significantly associated with prognosis. These results are similar to the results of most studies. These results further indicate that radiomics features are more effective than traditional imaging parameters in predicting the prognosis of NSCLC patients.However, there are still relatively few studies on PET/CT radiomics in predicting the efficacy and prognosis of NSCLC. Radiomics studies require a relatively large sample size, and most singlecenter studies are often unable to meet the sample size requirements of omics analysis. Therefore, most studies tend to design broad inclusion criteria without scientific grouping and stratification of enrolled patients. It is well known that tumor stage and treatment have a great impact on the prognosis of patients. If patients with different stages and receiving different treatment methods are analyzed in the same layer, the results will inevitably be biased.Our research set up a relatively strict entry criteria: all patients were inoperable with advanced NSCLC, and treatments are given priority to with chemotherapy. Then, the interference of clinicopathological factors was comprehensively considered, and on this basis, survival analysis was performed to obtain independent predictors of the prognosis of advanced NSCLC after chemotherapy and establish a prognostic model.
Radiomic feature extraction is a key step in radiomics research.In theory, the stereoscopic analysis of the whole tumor can better reflect the heterogeneity of the tumor than the maximum crosssectional analysis. Therefore, in this study, omics features were extracted in 3D VOI, and 42%SUVmax was used as the optimal threshold to avoid the interference of SUVmax inherent noise,variability, background uptake, and partial volume effect[15].Both PET/CT image features and RS are from the original image, but they represent two different methods of image analysis. Traditional image interpretation is a macroscopic observation of image features, which is subjective and easily influenced by the experience of physicians.Radiomics technology can reveal and quantify the microscopic features related to tumor heterogeneity in a non-invasive manner,but it is also limited by the complexity of its calculation and lack of standardization. Therefore, the integration of the two radiographic analysis methods and clinical factors into a composite model may lead to better decision making for patients with NSCLC. However,this study found that although the omics model had better predictive power than the other two models, there was no statistically significant difference in the Delong test results among the three models. There are two possible reasons for this result :(1) retrospective small sample study with a certain degree of data deviation;(2) the selection of SUV optimization threshold has a great impact on the shape and size of ROI, which may further influence the extraction of omics features [15-17].The above two aspects are also the limitations of this study. Therefore, the next goal of our study is to validate the model in a prospective multicenter clinical trial to improve data stability and reproducibility.In recent years, targeted therapy and immunotherapy for NSCLC have developed rapidly, which has greatly improved the survival outcomes of specific populations[18-20].Targeted therapies targeting EGFR, ROS1 fusion gene, MET gene amplification, and BRAF mutation gene targets are precisely providing more survival benefits for NSCLC patients. At the same time, immunotherapy is also constantly changing the diagnosis and treatment mode of advanced NSCLC, especially for patients who are resistant to conventional chemotherapy and targeted therapy. Based on this, the next step of this study will be to in-depth study and analyze the prognostic efficacy of radiomics between different genome and immune expression groups, in order to provide a basis for more accurate personalized treatment.In conclusion, the PET/CT radiomics model has a good predictive value for the prognosis of advanced NSCLC after chemotherapy. As a non-invasive and quantitative method, radiomic features may be a potential biomarker to provide a complement to traditional clinical and radiographic prediction models for personalized treatment of NSCLC patients. However, further validation is needed before widespread application in clinical practice.
Author's contribution:
Li Xueyan: design of experimental protocol, writing and revision of the paper;
Wang Dawei: responsible for paper review and image processing;
Yu Lijuan: responsible for writing instruction;
Chen Lu: Image analysis and radiomics analysis;
Pan Deng: clinical data collection of the enrolled patients.
All the authors declare that there are no conflicts of interest.
杂志排行
Journal of Hainan Medical College的其它文章
- Advances in BRAF gene mutations in papillary thyroid carcinoma
- Research progress on the correlation between lncRNA and the pathogenesis of COPFD
- Analysis of laboratory and imaging examination results of patients with COVID-19 2 years after discharge in Chengdu
- Efficacy and prognosis of vacuum-assisted excision for benign intraductal papilloma of breast: A meta-analysis
- Clinical efficacy and perioperative safety of simultaneous or staged bilateral total hip arthroplasty:A Meta analysis
- Kaempferol attenuates knee osteoarthritis via inhibiting cartilage apoptosis in mice