Clinical efficacy and perioperative safety of simultaneous or staged bilateral total hip arthroplasty:A Meta analysis
2022-11-02XIONGBinglangLINTianyeYANGPengXUJingliZOUQizhaoLAIQizhongLIZiqiHEWeiZHANGQingwen
XIONG Bing-lang, LIN Tian-ye, YANG Peng, XU Jing-li, ZOU Qi-zhao, LAI Qi-zhong,LI Zi-qi, HE Wei, ZHANG Qing-wen✉
1. The First Clinical Medical College, Guangzhou University of Chinese Medicine, Guangzhou 510405, China
2. The First Hospital of Traditional Chinese Medicine of Zhanjiang, Zhanjiang 524000, China
3. Department of Joint Orthopedic, the Third Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou 510405, China
Keywords:Bilateral Arthroplasty Replacement Hip Simultaneous Staged Meta-analysis
ABSTRACT Objective: To investigate the clinical efficacy and perioperative safety of simultaneous or staged bilateral total hip arthroplasty (THA) using meta-analysis. Methods: Relevant retrieval methods were developed to retrieve PubMed, Embase, Cochrane Library, CNKI, Wanfang and VIP databases, and the time was set to build the database until September 2020. All the literatures related to simultaneous or staged total hip arthroplasty were screened out. The final included literatures were determined according to the inclusion and exclusion criteria, and the quality of the literatures was evaluated. Meta analysis of all indexes was performed using Review Manager 5.3 software. Results: A total of 22 articles were included, including 3 415 patients. Meta analysis results showed that the total hospitalization time in the simultaneous group was significantly lower than that in the staged group [MD=-9.99,95%CI(-14.72, -5.26),P<0.000 1].Total hospitalization expenses in the simultaneous group were lower than those in the staged group [MD=-1.3, 95%CI (-1.73, -0.86), P<0.000 01]. The operative time in the simultaneous group was less than that in the staged group [MD=-27.08, 95%CI (-40.89,-13.26), P=0.000 1]. The total blood loss in the simultaneous group was less than that in the staged group [MD=-176.55, 95%CI (-282.5, -70.6), P=0.001]. The surgical transfusion volume in the simultaneous group was higher than that in the staged group [MD=69.85, 95%CI (40.48,99.22), P<0.000 01]. Postoperative Harris score of hip joint in the simultaneous group was higher than that in the staged group [MD=1.79, 95%CI(0.8, 2.79), P=0.000 4]. The incidence of operative complications in the simultaneous group was lower than that in the staged group[OR=0.73, 95%CI (0.56, 0.96), P<0.05]. Conclusion: Compared with staged bilateral total hip replacement, simultaneous bilateral total hip replacement has advantages in terms of reducing hospitalization time, saving hospitalization expense, shortening operation time and reducing surgical bleeding amount, and can promote postoperative hip function recovery, reduce postoperative complications, but increase total blood transfusion volume.
1. Introduction
Total hip arthroplasty is considered one of the most successful surgeries of the 21st century because it can significantly alter mobility and quality of life in patients with end-stage hip disease[1].Hip dysplasia, rheumatoid arthritis, necrosis of the femoral head and other diseases often involve bilateral hip joints, requiring bilateral total hip replacement.However, there is still controversy over whether it is a simultaneous or staged operation. Bilateral hip replacement at the same time was first proposed by Jaffe in 1971[2].Some studies believe that because only one anesthesia is required,bilateral total hip arthroplasty can reduce the length of hospital stay and the total cost of hospitalization, and can promote the recovery of hip joint mobility to improve the efficiency of surgery[3, 4]. A recent retrospective study by Guo[5] also proved that simultaneous bilateral total hip arthroplasty has a lower postoperative complication rate than staged bilateral total hip arthroplasty, but the postoperative blood transfusion rate is higher. However, Tan[6]'s study found that within 90 days after the operation, there was no significant difference in the total hospitalization costs and the incidence of postoperative complications between the two groups. Although some articles have evaluated and compared simultaneous total hip arthroplasty and staged total hip arthroplasty, most of these studies are clinical studies based on small sample data, and the results obtained have a high risk of bias and insufficient reliability. In this study, the Meta-analysis method was used to compare the hospitalization time, hospitalization cost, operation time, total blood loss, total blood transfusion volume, postoperative Harris score of hip joint, and incidence of postoperative complications between the same period and stage groups to comprehensively evaluate The clinical efficacy and safety of both. To the greatest extent, the problems of insufficient sample size and lack of evaluation indicators in previous single studies have been overcome. The obtained conclusions provide evidencebased medical evidence for the formulation of bilateral total hip arthroplasty surgical plans.
2. Materials and Methods
2.1 Search Methods and Strategies
Three researchers independently searched PubMed, Embase,Cochrane Library English databases and CNKI, Wanfang, VIP and other Chinese knowledge bases, the time was set from the establishment of the database to May 2021, and the English database search method was subject words plus free word,Search keywords included bilateral、Arthroplasty, Replacement, Hip、Arthroplasties,Replacement, Hip、Arthroplasty, Hip Replacement、Hip Prosthesis Implantation、Hip Prosthesis Implantations、Implantation, Hip Prosthesis、Implantations, Hip Prosthesis、Prosthesis Implantation, Hip、Prosthesis Implantations, Hip、Hip Replacement Arthroplasty、Replacement Arthroplasties, Hip、Replacement Arthroplasty, Hip、Arthroplasties, Hip Replacement、Hip Replacement Arthroplasties、Hip Replacement, Total、Replacement, Total Hip、Hip Replacements, Total、Replacements,Total Hip、Total Hip Replacements、Total Hip Replacement、simultaneous、staged. Chinese search terms include: bilateral hip replacement, simultaneous, stage.
2.2 Literature Inclusion and Exclusion Criteria
2.2.1 Inclusion criteria for the literature
1.The study type is a cohort study or a randomized controlled study.2.Subjects: Patients with severe hip disease requiring bilateral total hip arthroplasty.3.Intervention measures: the simultaneous total hip arthroplasty was performed in the contemporaneous group,and the staged total hip arthroplasty was performed in the staged group.4.Efficacy and safety evaluation indicators: at least one of the indicators such as hospitalization time, hospitalization cost, operation time, blood loss, blood transfusion, hip Harris score, postoperative complication rate.
2.2.2 Exclusion criteria
1.Animal experiment.2.Literature for which full text is not available.3.Repeated publications, conference abstracts, reviews.4.No control group was set, there were obvious errors in clinical data, and there was no literature on relevant outcome evaluation indicators.
2.3 Literature screening and literature quality evaluation
The retrieved literature was screened by 2 investigators according to the inclusion and exclusion criteria. First, deduplicate the retrieved literature. Read the titles and abstracts of the literatures, preliminarily exclude literatures that are obviously irrelevant to the research purpose, download and read the full texts of the literatures that initially meet the requirements, and finally screen out the included literatures. The NOS scoring scale [28] was used to evaluate the quality of the included cohort research literature, with a total score of 9 points. The evaluation content mainly included the selection of cases, comparability between groups, and the formulation of results evaluation methods.A score of more than 5 points can be considered to be of good quality and can be included in the meta-analysis.Randomized controlled trials were evaluated using a modified Jadad scale [29], with a total score of 7 points, and a score greater than 3 was defined as high-quality literature included in this study.
2.4 data analysis
This study used Review Manager 5.3 software to perform a metaanalysis of the included literature data. Since the data included in this study included both enumeration data and measurement data,the WMD and OR values were calculated according to the data type as the effect size, and the 95% confidence interval (Cl) of all effect sizes was calculated, represented by a P value less than 0.05. The difference is statistically significant. The I2 test was performed to assess the heterogeneity of the statistic, where the I2 value of 0%,25%, 50%, and 75% represented no heterogeneity, low heterogeneity,moderate heterogeneity, and high heterogeneity, respectively sex.When I2<50%, a fixed effect model was used. When I2>50%,a random effects model was used. When heterogeneity is large,perform sensitivity analysis, subgroup analysis, or assess sources of heterogeneity by varying effect sizes
3. Results
3.1 The results of a literature search
A total of 1092 articles were retrieved through the established search formula: PubMed (360 articles), Embase (44 articles), Cochrane Library (46 articles), HowNet (187 articles), Wanfang (256 articles),VIP (199 articles) ). Import all documents into EndNote software,after removing duplicate documents, there are 570 remaining documents. After two researchers carefully read the title and abstract of the literature, and screened according to the inclusion and ranking criteria, there were 64 remaining literatures. After reading the full text, 22 papers that met the requirements were finally included, with a total of 2,046 people in the experimental group and 1,369 people in the control group, as Figure 1.

Figure 1 Flow chart of literature retrieval and screening
3.2 Literature quality evaluation
A total of 20 retrospective cohort studies and 2 randomized controlled studies were included, as shown in Table 1. According to the NOS score, in retrospective cohort studies, 5 [5, 6, 23-25] were rated 8, 5 [11, 13, 15, 17, 20] were rated 7, and 10 [ 7-10, 12, 14, 16, 18-19,21] were rated as 6. According to the modified Jadad score, 2 articles[22,26] in RCTs were rated as 4 points.

Table 1 Basic features of the included studies
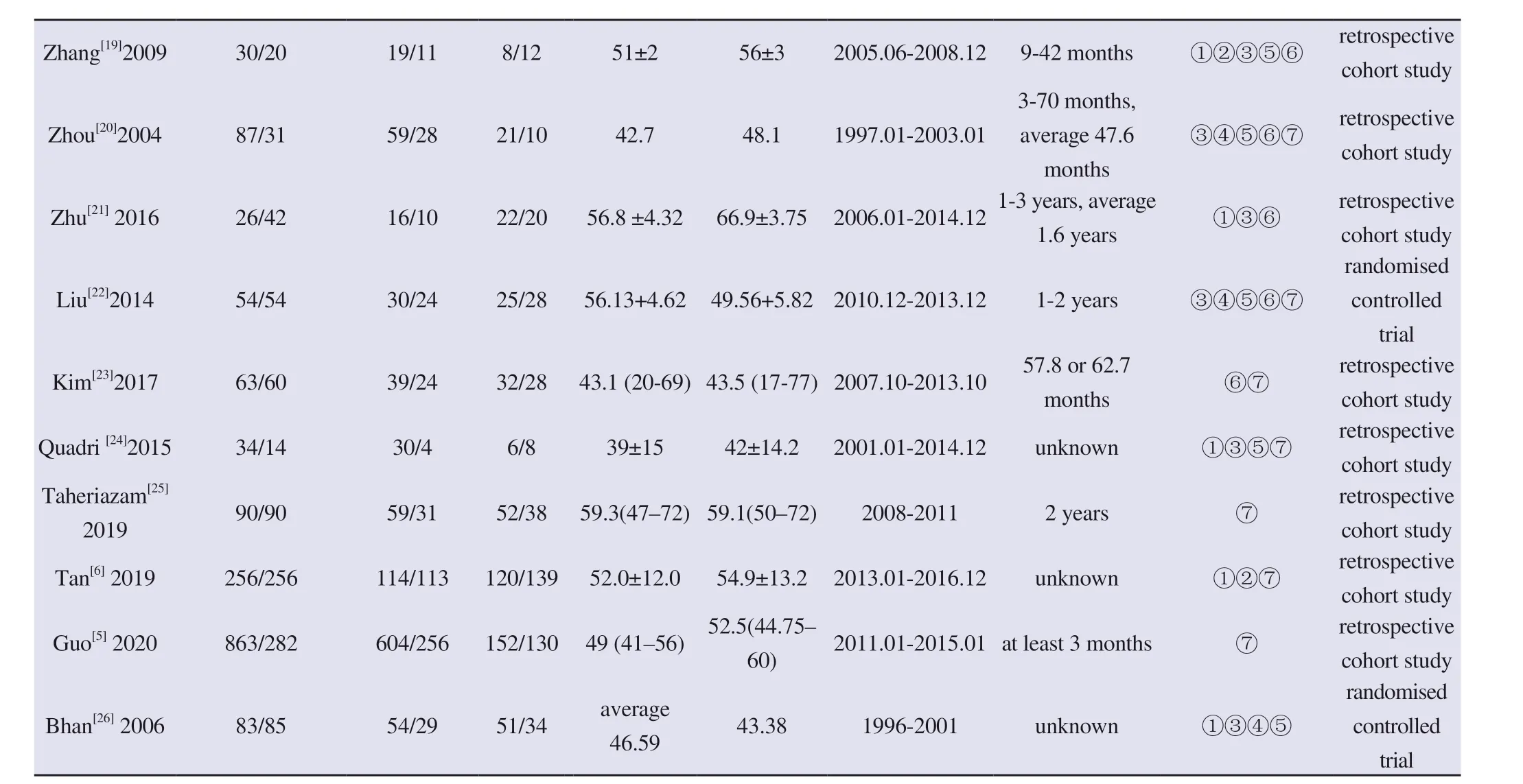
Outcome indicators: ①Length of hospital stay ②Total hospital expenses ③Operation time ④Total blood loss ⑤Total blood transfusion ⑥Postoperative Harris score of hip joint ⑦Postoperative complication rate
3.3 Meta analysis
3.3.1 hospital stay
A total of 14 articles [6-9, 11-16, 19, 21, 24, 26] were included to evaluate the length of hospital stay (753 cases in the same period group and 710 cases in the stage group). Due to the obvious heterogeneity between the two groups (I2=100%, P less than 0.000 01), a random effect model was used. After comparing the two sets of data, the final conclusion is drawn:The difference was statistically significant, and the hospital stay in the same period group was significantly shorter than that in the stage group (MD=-9.99, 95%CI(-14.72, -5.26), P<0.000 1), as shown in Figure 2.
3.3.2 Hospital costs
Among the included literatures, there are 7 [6,8,11,13,15,16,19]literatures comparing the hospitalization costs between the two groups (concurrent group: 530 cases, staging group: 458 cases). The meta-analysis showed that the heterogeneity between the two groups was large (I2=98%, P less than 0.000 01), so a random effect model was used. The comparison between the two groups showed that the difference was statistically significant, and the hospitalization expenses in the same period group were lower than those in the stage group (MD=-1.3, 95%Cl (-1.73, -0.86), P<0.000 01), as shown in Figure 3.
3.3.3 operation time
A total of 15 articles [8,9,11-13,15-22,24,26] compared the operation time between the two groups (669 cases in the same period group,597 cases in the stage group), because there is heterogeneity between the two groups (I2=99%, P less than 0.000 01), so a random effect model is used. Meta-analysis results showed that the comparison of operation time between the two groups was statistically significant,and the operation time in the same period group was shorter than that in the stage group (MD=-27.08, 95%Cl (-40.89, -13.26), P=0.000 1),as shown in Figure 4.
3.3.4 Total bleeding
A total of 11 [7,8,10,12,13,16-18,20,22,26] literatures compared the total blood loss during the perioperative period (558 cases in the same period group and 486 groups in the stage group). There was obvious heterogeneity between the two groups (I2=99%, P less than 0.000 01), so a random effect model was used. Meta-analysis results showed that the total bleeding volume between the two groups was statistically significant, and the total bleeding volume in the same period group was less than that in the staged group (MD=-176.55,95%Cl (-282.5, -70.6), P=0.001), as shown in Figure 5.

Figure 2 Comparison of total length of hospital stay between simultaneous and staged bilateral THA
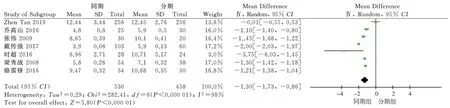
Figure 3 Comparison of total hospitalization costs of simultaneous and staged bilateral THA

Figure 4 Comparison of operative time between simultaneous and staged bilateral THA
3.3.5 Total blood transfusionA total of 12 articles [7, 8, 10, 11, 15-17, 19, 20, 22, 24, 26] were included to compare the total perioperative blood transfusion volume between the two groups (589 cases in the same period, staging 481 groups),due to the obvious heterogeneity between the two groups in the heterogeneity test (I2=67%, P=0.000 5), a random effect model was used. Meta-analysis results showed that the total blood transfusion volume between the two groups was statistically significant, and the total blood transfusion volume in the same period group was greater than that in the stage group (MD=69.85, 95%Cl (40.48, 99.22),P<0.000 01), as shown in Figure 6.
3.3.6 Postoperative Hip Harris Score
A total of 13 articles [7-9, 12, 13, 15, 16, 18-23] were included to compare the Harris scores of the hip joint between the two groups(583 cases in the same period group and 489 groups in the stage group). There was significant heterogeneity between the two groups in the heterogeneity test (I2=82%, P less than 0.000 01), so a random effect model was used. Meta-analysis results showed that the postoperative Harris score of hip joint was statistically significant between the two groups, and the postoperative Harris score of hip joint in the same period group was higher than that in the stage group(MD=1.79, 95%Cl (0.8, 2.79), P=0.0004), as shown in Figure 7.
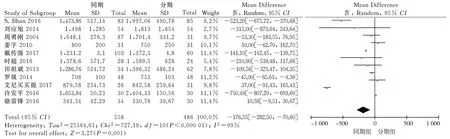
Figure 5 Comparison of total bleeding volume during simultaneous and staged bilateral THA

Figure 6 Comparison of total blood transfusion volume between simultaneous and staged bilateral THA
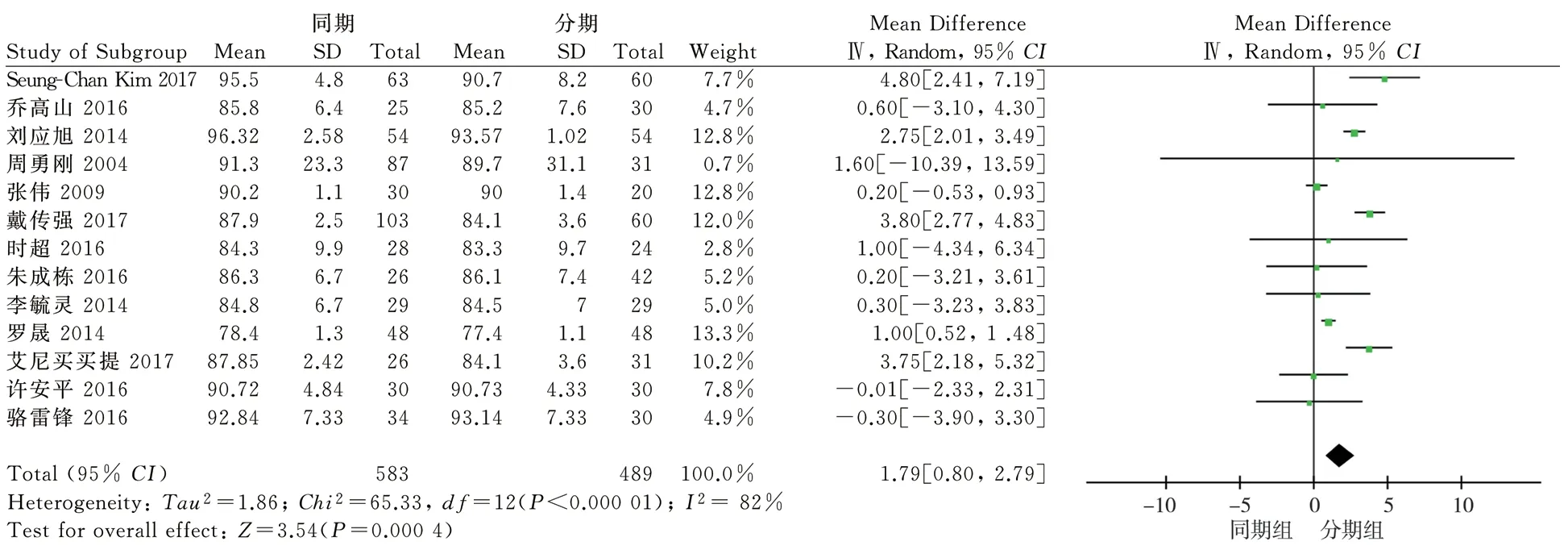
Figure 7 Comparison of Harris score of hip joint after simultaneous and staged bilateral THA
3.3.7 Postoperative complications
A total of 15 articles [5-9, 11, 13-15, 18, 20, 22-25] were included to compare the incidence of postoperative complications between the two groups (1763 cases in the same period group, 1057 cases in the stage group) , the heterogeneity test showed that the heterogeneity between the two groups was low (I2=42%, P=0.05), so a fixed effect model was used. The results of Meta analysis showed that the incidence of complications between the two groups was statistically significant, and the incidence of surgical complications in the same period group was lower than that in the stage group (OR=0.73,95%Cl (0.56, 0.96), P<0.05), as shown in the figure 8.

Figure 8 Comparison of postoperative complications between simultaneous and staged bilateral THA
3.4 Sensitivity analysis
In this study, a sensitivity analysis was performed for the comparison of hospitalization time, total hospitalization cost,operation time, total blood loss, postoperative hip Harris, etc. with greater heterogeneity. Eliminating some documents or changing the analysis effect model has not affected the results, so it is confirmed that the results obtained in this study are still credible.
3.5 publication bias
This study conducted a publication bias analysis on the incidence of postoperative complications. The results showed that the included literatures were basically symmetrically distributed on both sides of the funnel plot, indicating that the risk of publication bias was small,as shown in Figure 9.

Figure 9 Funnel plot of postoperative complications
4. Discussions
It has been reported that 20% of patients with primary total hip arthroplasty also require contralateral total hip arthroplasty within 5 years [27]. Many end-stage hip diseases require bilateral hip replacement. Considering economic factors and the need for rapid rehabilitation, simultaneous bilateral hip replacement has received widespread attention since it was proposed. However, its clinical efficacy and safety are still controversial. A study by Taheriazam[25]in 2019 found that bilateral hip replacement in the same period did not increase the incidence of postoperative complications compared with the staged group, and there was no significant difference in postoperative hip mobility. In this study, 22 relevant research papers were included and Meta-analysis was conducted to conclude that the incidence of postoperative complications in the same period group was lower than that in the staging group,and the postoperative recovery of hip joint function was better. The reason for the higher incidence of postoperative complications in the staging group may be related to the increased activity of the patients after the second operation compared with the same period group.Tan[26] retrospectively analyzed the clinical data of 512 patients with bilateral hip arthroplasty and believed that in terms of total hospitalization costs, there was no significant difference between the contemporaneous group and the staged group, but the hospitalization time of the contemporaneous group was shorter than that of the staged group. This is consistent with some of the conclusions of this study. This study believes that the hospitalization time of the contemporaneous group is shorter than that of the staged group, and the hospitalization cost is also lower, so the choice of simultaneous bilateral hip replacement can better alleviate the economic pressure.This difference may be due to the fact that simultaneous surgery can reduce the cost of secondary anesthesia and related routine examination costs, and reduce the hospitalization time occupied by preoperative preparations. In addition, this study also concluded that simultaneous bilateral hip replacement can shorten the operation time and reduce the amount of surgical blood loss, but the total blood transfusion volume in the perioperative period is more, which is consistent with the results of Bhan et al[26]. Therefore, it can be concluded that the safety of bilateral simultaneous hip replacement is better.
In this study, we searched multiple databases in both Chinese and English, strictly formulated standards for inclusion in the literature, and conducted a Meta-analysis of the literature data. The hospital costs, surgical safety and clinical efficacy were compared between the simultaneous bilateral hip replacement and the staged bilateral hip replacement. Finally, the following conclusions were drawn: Compared with staged bilateral hip arthroplasty,simultaneous bilateral hip arthroplasty has advantages in reducing hospital stay, saving hospital costs, shortening operative time, and reducing operative blood loss, etc., and can improve postoperative hip function recovery and reduce postoperative complications.Complications, but increased total transfusion volume. Therefore,we can speculate that the clinical efficacy of simultaneous bilateral hip replacement is equivalent to the safety and staged bilateral hip replacement, and it can shorten the length of hospital stay and reduce the total cost of hospitalization. Under the condition of grasping the surgical indications and contraindications, simultaneous bilateral hip replacement can be selected.
The shortcomings of this study: (1) The research time of the included literature is inconsistent. Due to differences in surgical techniques and price levels, the analysis of indicators such as hospitalization time, total hospitalization expenses, and operation time will have an impact. (2) The heterogeneity of the included literature is large, and the heterogeneity may be due to the different proficiency of the surgeons in the operation, the different methods of measuring and evaluating indicators, and the subjective differences of the researchers. (3) Among the 22 literatures included in this study, 20 were retrospective cohort studies, lacking high-quality randomized controlled studies. (4) There are differences in the follow-up time of relevant outcome indicators in this study, which may have an impact on the results of the study.In summary, based on the current research results, we believe that the clinical efficacy of simultaneous bilateral hip replacement is equivalent to the safety and staged bilateral hip replacement, and it can shorten the length of hospital stay and reduce the total cost of hospitalization. However, there is still a lack of large randomised controlled trials to further improve the quality of the included literature.
Author Contribution: Binglang Xiong, first author, research designer, involved in literature retrieval, screening, data analysis,paper writing. Zhang Qingwen, corresponding author, proofreader of research proposal and article content. Second author, participated in literature search and screening. The third author, involved in data processing. The fourth author gives technical guidance to the software. The fifth and sixth authors participated in the literature quality assessment. Seventh and eighth authors, participating in the correction of the first draft of the article.
杂志排行
Journal of Hainan Medical College的其它文章
- Advances in BRAF gene mutations in papillary thyroid carcinoma
- Research progress on the correlation between lncRNA and the pathogenesis of COPFD
- Analysis of laboratory and imaging examination results of patients with COVID-19 2 years after discharge in Chengdu
- Efficacy and prognosis of vacuum-assisted excision for benign intraductal papilloma of breast: A meta-analysis
- Kaempferol attenuates knee osteoarthritis via inhibiting cartilage apoptosis in mice
- Effect of Acacetin on flagellin induced NLRC4 inflammasome activation in mouse bone marrow-derived macrophages