Oesophageal cancer metastases: An observational study of a more aggressive approach
2022-10-11LiannePickettMaryDunneOrlaMonaghanLiamGroganOscarBreathnachThomasWalsh
Lianne Pickett, Mary Dunne, Orla Monaghan, Liam Grogan, Oscar Breathnach, Thomas N Walsh
Lianne Pickett, Department of Surgery, Connolly Ηospital, Blanchardstown, Dublin D15 X40D, Ireland
Mary Dunne, Clinical Trials Resource Unit, St Luke's Radiation Oncology Network, Dublin D06 ΗΗ36, Ireland
Orla Monaghan, Department of Radiation Oncology, St Luke's Radiation Oncology Network, Dublin D06 ΗΗ36, Ireland
Liam Grogan, Oscar Breathnach, Department of Medical Oncology, Beaumont Ηospital, Dublin D09 V2N0, Ireland
Thomas N Walsh, Department of Surgery, RCSI Bahrain, Adliya 15503, Bahrain
Abstract BACKGROUND The prognosis for oesophageal carcinoma is poor, but once distant metastases emerge the prognosis is considered hopeless. There is no consistent protocol for the early identification and aggressive management of metastases.AIM To examine the outcome of a policy of active postoperative surveillance with aggressive treatment of confirmed metastases.METHODS A prospectively maintained database of 205 patients diagnosed with oesophageal carcinoma between 1998 and 2019 and treated with curative intent was interrogated for patients with metastases, either at diagnosis or on follow-up surveillance and treated for cure. This cohort was compared with incomplete clinical responders to neoadjuvant chemoradiotherapy (nCRT) who subsequently underwent surgery on their primary tumour. Overall survival was estimated using the Kaplan-Meier method, and the log-rank test was used to compare survival differences between groups.RESULTS Of 205 patients, 11 (5.4%) had metastases treated for cure (82% male; median age 60 years; 9 adenocarcinoma and 2 squamous cell carcinomas). All had undergone neoadjuvant chemotherapy or chemoradiotherapy, followed by surgery in all but 1 case. Of the 11 patients, 4 had metastatic disease at diagnosis, of whom 3 were successfully downstaged with nCRT before definitive surgery; 2 of these 4 also developed oligometastatic recurrence and were treated with curative intent. Following definitive treatment, 7 had treatment for metachronous oligometastatic disease; 5 of whom underwent metastasectomy (adrenal × 2; lung × 2; liver × 1). The median overall survival was 10.9 years [95% confidence interval (CI): 0.7-21.0 years], which was statistically significantly longer than incomplete clinical responders undergoing surgery on the primary tumour without metastatic intervention [n = 62; median overall survival = 1.9 (95%CI: 1.1-2.7; P = 0.012]. The cumulative proportion surviving 1, 3, and 5 years was 100%, 91%, and 61%, respectively compared to 71%, 36%, and 25% for incomplete clinical responders undergoing surgery on the primary tumour who did not undergo treatment for metastatic disease.CONCLUSION Metastatic oesophageal cancer represents a unique challenge, but aggressive treatment can be rewarded with impressive survival data. In view of recent advances in targeted therapies, intensive follow-up may yield a greater number of patients with curative potential and thus improved long-term survival.
Key Words: Oesophageal metastases; Oligometastases; Active surveillance; Treatment for cure; Metastasectomy; Survival
lNTRODUCTlON
Oesophageal cancer is an aggressive disease that presents insidiously, disseminates early, and spreads rapidly in most patients. It remains a leading cause of death from cancer worldwide and fewer than 5%-12% will survive 5 years[1,2]. At least 40% of patients present with distant metastasis at initial diagnosis[3], and only 5% of these patients will be alive at 5 years[4]. Even when presenting with early disease, 29%-54% of patients undergoing surgical resection with curative intent will develop locoregional or distant recurrence[5-7]. Of patients with a ypT0N0M0 tumour at resection following neoadjuvant chemoradiotherapy (nCRT), up to 17% will succumb to distant metastases[8-10]. Because of these poor survival outcomes, the role of intensive surveillance post-oesophagectomy and treatment of metastatic disease remains controversial.
The management of oesophageal cancer has undergone major advances over the past 30 years. Specifically, both neoadjuvant chemotherapy and nCRT have been shown to increase survival over surgery alone[11-13]. While neoadjuvant chemotherapy has achieved this increase by targeting occult micrometastases[14], combined CRT has increased survival by both targeting micrometastases and sterilizing locoregional disease, thus up to 50% of patients with squamous cell carcinoma (SCC) and up to 25% of patients with adenocarcinoma (AC) undergoing CRT have a complete pathological response in the resected specimen, depending on the regimen and the disease stage[11,12].
Nevertheless, metastatic oesophageal cancer remains a challenge. Oligometastases are defined as a state of limited metastatic disease characterized by fewer than five metastases[5,15]. Synchronous oligometastases may be detected at the time of diagnosis of the primary cancer, while metachronous oligometastases are those detected during follow-up[5,16]. Metastasectomy is well-established in the treatment of certain oligometastatic cancers, such as colorectal cancer, where partial hepatectomy and pulmonary resection are well established[5]. Both the United Kingdom’s National Institute for Health and Clinical Excellence and the United States’ National Comprehensive Cancer Network recommend surveillance strategies to identify recurrence as well as liver and pulmonary metastasectomy where possible[17,18]. In contrast, the National Institute for Health and Clinical Excellence recommends neither routine clinical follow-up nor radiological follow-up be offered to patients who have no symptoms or evidence of residual disease after treatment for oesophagogastric cancer with curative intent for the detection of recurrent disease[19]. The National Comprehensive Cancer Network reco-mmends clinical follow-up alone for asymptomatic patients and palliation alone for patients who develop metastatic recurrence[20].
Over the past decades, efforts have focused on the molecular and biological alterations that lead to oesophageal cancer, specifically the influence of angiogenesis on micrometastatic tumour growth[21,22]. This has resulted in the development of novel molecularly targeted agents that target a variety of relevant pathways, such as vascular endothelial growth factor, cyclooxygenase-2, epidermal growth factor receptor, and mammalian target of rapamycin[23] as well as targeted radiotherapy in the form of stereotactic radiotherapy[24]. Leading the way are HER-2 inhibitors for the treatment of HER-2 expressing metastatic ACs[23]. It is intuitive that aggressive treatment of oligometastatic disease would improve disease control and provide a survival benefit for patients with recurrent cancer detected at its earliest stage. The purpose of this study was to examine survival outcomes in patients who underwent active surveillance and targeted therapy at our institution for their oligometastatic disease.
MATERlALS AND METHODS
Study design and patients
We conducted a retrospective review of a prospectively maintained database of all patients diagnosed with oesophageal carcinoma and treated with curative intent between 1998 and 2019 at Connolly Hospital Blanchardstown, Dublin, Ireland. Patients were treated with either CRT alone, or CRT followed by surgery, or surgery alone.
Patient management and follow-up
Over a 21-year period, 205 patients with oesophageal carcinoma underwent curative management. Following discharge, patients were followed up in the clinic every 3 mo for the first 3 years with esophagogastroduodenoscopy performed every 3 mo and computed tomography (CT) performed every 6 mo. Between 3 years and 5 years they were followed up in the clinic every 6 mo with esophagogastroduodenoscopy every 6 mo and CT scanning performed annually. After 5 years patients were followed up annually with endoscopy and a clinic visit (which was on the same day for patients who had to travel from a distance). In addition, patients had access to their oncology coordinator and were encouraged to call at any time with any concern. On receipt of a call, the coordinator would offer them a clinic visit or an esophagogastroduodenoscopy (or other imaging) depending on their symptoms or concerns.
Patient database
A patient database was maintained over the study period, both by nursing and clinical staff. This was scrutinized for patients with synchronous and metachronous oligometastases. Only patients who underwent curative treatment of oligometastatic disease were included in this study. A second group of patients (with non-metastatic disease) who had an incomplete clinical response to nCRT and subsequently underwent surgery on the primary tumour were identified for comparison of survival outcomes.
Of 205 patients treated with curative intent, 62 had an incomplete response to nCRT for nonmetastatic oesophageal cancer and subsequently underwent surgery, and 11 had oligometastases treated for cure. The medical and electronic records of the oligometastatic cohort treated for cure were reviewed for demographic, clinical, and histopathologic variables. Notably, staging of the primary oesophageal cancer was prospectively assigned according to the TNM classification of the American Joint Committee for Cancer Staging, initially the 6thedition and then the 7thfollowing its publication. Each case was assessed with respect to the use of neoadjuvant therapy, history of oesophagectomy, and timing of metastasis. Further details regarding the site and treatment of metastasis were included. Survival data was included for analysis and comparison.
Ethical approval
As this was a retrospective audit ethical approval was not required, but audit approval was sought and granted by the Connolly Hospital Ethics Committee.
Statistical analysis
The statistical analysis of this study was performed by biostatistician Mary Dunne from St Luke’s Radiation Oncology Network, Dublin D06 HH36, Ireland. Overall survival was estimated using the Kaplan-Meier method and was defined as the duration from the date of diagnosis until death from any cause or last follow-up at study endpoint on February 26, 2020. The log-rank test was used to compare survival differences between groups (assessed for significance at the 0.05 level). Statistical analysis was performed using IBM SPSS Statistics 25 (Chicago, IL, United States).
RESULTS
Clinical characteristics of patients
Of the 205 patients, 11 (5.4%) patients diagnosed with oesophageal carcinoma [146 (71.0%) male; 135 (65.9%) AC; 68 (33.2%) SCC; 2 adenosquamous)] between 1998 and 2019 and treated with curative intent had metastases treated for cure. Of these, 4 had synchronous oligometastatic oesophageal cancer, 2 of which also had treatment for cure for oligometastatic recurrence. A further 7 had metachronous oligometastatic oesophageal cancer only. The median age of patients with synchronous metastasis was 65 years (range: 53-71 years; AC 75%) and in patients with metachronous carcinoma was 57 years (range: 36-72 years; AC 86%) (Table 1). The majority of both cohorts were male (75% and 86%, respectively).
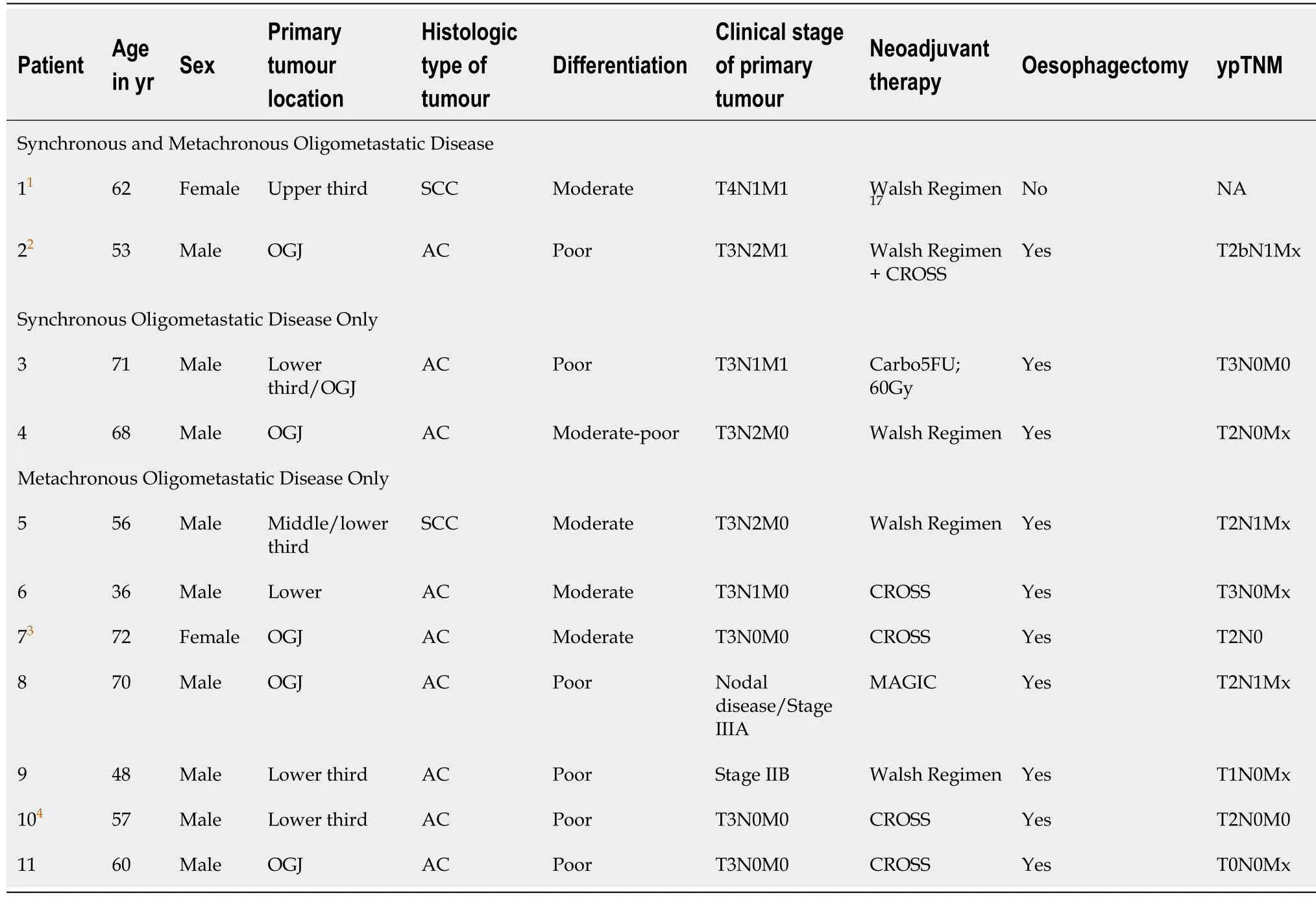
Table 1 Clinical characteristics of patients
Treatment of synchronous oligometastatic oesophageal cancer
The 4 patients that had metastatic disease at presentation were treated with nCRT, 3 of whom underwent subsequent oesophagectomy and achieved a margin free R0 resection and 1 of whom declined surgery following a clinical complete response to nCRT (Table 1). Two of these patients subsequently presented with metachronous metastases, which were also treated for cure (Table 2).

Table 2 Treatment of synchronous and metachronous oligometastatic oesophageal carcinoma
Patient 1 had locally advanced SCC at diagnosis (T4N1M1). Despite a complete clinical response to definitive CRT, routine surveillance positron emission tomography-CT (PET-CT) almost 12 mo later (11.5 mo) revealed fluorodeoxyglucose (FDG) avid lung lesions bilaterally. These were subsequently treated with stereotactic radiotherapy. The patient survived for 3 years post metastatic recurrence (36.4 mo). Patient 2 had a 12 mm short-axis FDG-positive lymph node lying immediately to the right of the coeliac axis on staging PET-CT (AC, T3N2M1). The patient was treated with nCRT and radical oesophagogastrectomy for a poorly differentiated junctional/cardia AC (ypT2bN1Mx). Almost 18 mo later (17.9 mo) a radiological work-up for a pulmonary embolus revealed a 1.9 cm left para-aortic node with FDG uptake on PET-CT, which was subsequently treated with chemotherapy (Table 2). Follow-up CT showed a reduction in tumour size and subsequent surveillance with endoscopy and CT revealed stable disease with no evidence of recurrence. The patient was alive and well at the conclusion of this study, 83.3 mo after his initial diagnosis (65.4 mo post-recurrence).
Two further patients (Patient 3 and Patient 4) had treatment for cure of synchronous oligometastatic disease only (Tables 1 and 2). Patient 3 had liver metastasis on staging PET-CT (AC, T3N1M1). Restaging CT post nCRT was negative for liver metastasis, and the patient subsequently underwent oesophagectomy (ypT3N0M0). Patient 4 had a 1 cm FDG avid right supraclavicular node on staging PET-CT (AC, T3N2M0) and underwent nCRT and subsequent oesophagectomy for a moderate to poorly differentiated AC at the oesophagogastric junction (ypT2N0Mx). The patient was alive and well at the conclusion of this study, 8.5 years after his initial diagnosis (102.8 mo).
Treatment of metachronous oligometastatic oesophageal cancer
The remaining 7 patients did not have clinical evidence of metastatic oesophageal cancer at diagnosis. These patients had mostly T3 disease with or without nodal involvement (Table 1; Patient 5-11). All underwent nCRT or neoadjuvant chemotherapy followed by surgery for their primary cancer. Of this cohort (n= 7), 3 developed pulmonary recurrence, 2 adrenal, 1 liver, and 1 patient had biopsy proven retroperitoneal nodal recurrence. All 7 patients underwent targeted treatment for metastatic recurrence with intent to cure, the details of which are summarized in Table 2. The median time from diagnosis to recurrence was 19.2 mo (range: 15.7-33.0 mo), and the median survival post recurrence was 97.4 mo [95% confidence interval (CI): 0-204 mo). The median overall survival (MOS) was 130 mo (95%CI: 3-258 mo), or the MOS was 10.9 years (95%CI: 0.2-21.5 years).
Survival outcomes
The MOS of the 11 patients who underwent curative treatment for synchronous or metachronous metastatic disease or both was 10.9 years (95%CI: 0.7-21) which was statistically significantly longer than patients with an incomplete clinical response following nCRT undergoing surgery [n= 62; MOS = 1.9 years (95%CI: 1.1-2.7);P= 0.012] (Figure 1). Of note, the latter did not undergo curative treatment for any future proven or probable metastatic recurrence. The cumulative proportion of patients with metastatic disease treated for cure surviving 1, 3, and 5 years was 100%, 91%, and 61%, respectively, with 6 patients still alive at the end of the study period, compared to 71%, 36%, and 25% for incomplete clinical responders without metastatic disease undergoing surgery on the primary tumour.
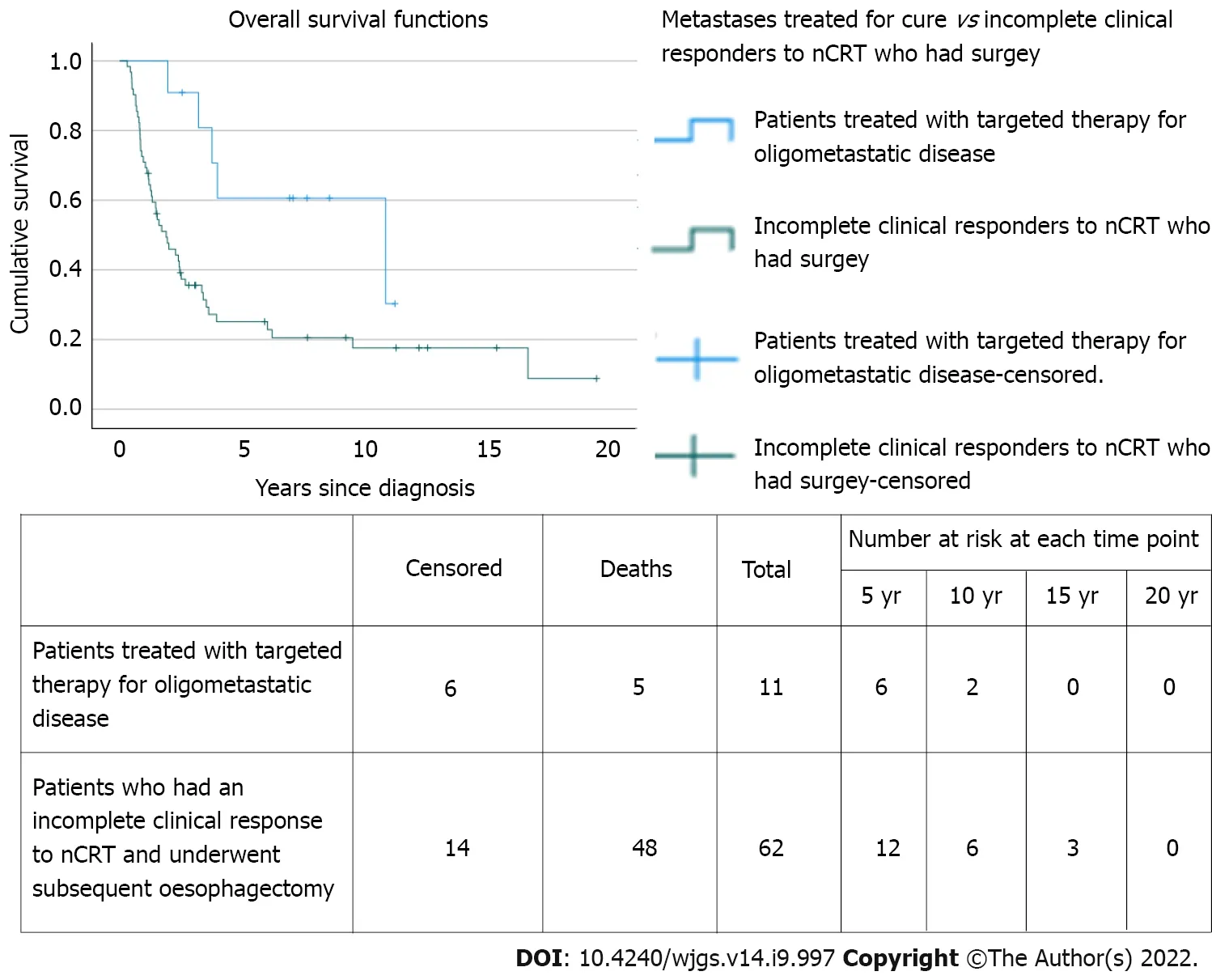
Figure 1 Survival plots for patients undergoing treatment of oligometastatic disease for cure vs patients with an incomplete clinical response to neoadjuvant chemoradiotherapy who underwent subsequent oesophagectomy. nCRT: Neoadjuvant chemoradiotherapy.
Patients that underwent surgical resection for their recurrence (n= 5) had a MOS of 10.9 years (95%CI: 0.6-21.2) from date of diagnosis, 8.1 years (95%CI: 0-16.8 years) post recurrence, and a 5-year survival of 80% from the date of diagnosis.
DlSCUSSlON
Patients with metastatic oesophageal cancer present a unique challenge. Although solitary metastases of oesophageal cancer are uncommon[25], the evolution of imaging will ensure ever-earlier detection, which challenges oncologists and surgeons to detect and deal with them. Treatment of oligometastatic oesophageal cancer is controversial, and to date formal guidelines are lacking. There are no large randomized multicenter trials, and thus case series, such as ours, remain an important source of information for clinicians managing these challenging patients.
Those patients treated surgically for recurrence in our study had a MOS of 10.9 years, or 130.3 mo and a 5-year survival of 80%. Depypereet al[26] conducted a large retrospective study comparing different treatment options for different subtypes of recurrence following curative resection, including single solid organ metastasis and single metastasis at another location. Of 1754 patients that had curative resection, 43.7% had recurrence, 14.4% of whom had clinical solitary solid organ recurrence (liver, lung, brain, or adrenal)[26]. Only 20 patients (1.14%) had their recurrence resected with or without systemic therapy and had a significantly better median and 5-year survival than 63 non-surgically treated patients [54.8 mo (5-year survival 43.9%)vs11.6 mo (5-year survival 4.6%)][25,26]. Arguably, those suitable for resection self-select, but the survival statistics for metastatic resection in a disease as aggressive as oesophageal cancer are impressive.
The patients in our study who underwent adrenalectomy were alive at 62.1 and 118.9 mo post recurrence. The oesophagus is the third most frequent site of origin of adrenal metastasis[27], and there are only a few reports of adrenalectomy for recurrence with survival ranging from 28 mo to over 5 years[27-30]. These findings confirm that adrenalectomy for isolated adrenal metastases from oesophageal carcinoma is worthwhile. A disease-free interval of over 6 mo and an AC subtype are reported as predictors of improved survival and should be considered in patient selection[31,32]. As adrenal metastases are clinically silent, intensive surveillance imaging is indicated if they are to be identified early enough for curative resection.
The remaining patients who underwent metastasectomy in our case series had either lung or liver metastases. All had metachronous oligometastases, had received nCRT, and had undergone resection of their primary tumour. Those who underwent pulmonary metastasectomy lived for 26.1 and 97.4 mo post recurrence, while the patient who underwent liver metastasectomy was alive and disease-free at 51.9 mo post recurrence. While hepatectomy and pulmonary resection are universally recommended for colorectal cancer metastases[17,18], they are not recommended for oesophageal cancer[19,20]. A nationwide study by Seesinget al[33] of the Dutch national registry for histopathology and cytopathology identified 32057 patients who underwent resection for gastro-oesophageal cancer between 1991 and 2016 and reported that 34 (0.11%) underwent resection for pulmonary (n= 15) or hepatic (n= 19) metastases across 21 hospitals and had an overall 5-year survival of 53% and 31%, respectively[33]. Liuet al[34] reported that 26 SCC patients with solitary hepatic metastasis, who underwent liver resection, had 1- and 2-year survival rates of 50.8% and 21.2%, respectively, which was significantly higher than the 31.0% and 7.1% survival rates for the 43 non-surgically treated patients[34].
Oesophageal cancer patients very frequently present with metastases, which almost inevitably consigns them to palliative management. Until recently primary cancer resection in these circumstances was rarely considered. Of the 4 patients who presented with metastatic oesophageal cancer in our case series, 3 underwent surgery to the primary cancer. All 3 had nCRT and all achieved an R0 resection, with a cumulative proportion surviving 2 years of 67%. Zhanget al[35] analysed a large populationbased cohort of 4367 metastatic oesophageal cancer patients (M1b-stage) from the SEER database[35] and found a significant survival benefit for surgery for the primary tumour with a median survival for the surgery group of 14 mo compared with 9 mo for the no surgery AC group, and a similar significant survival advantage for surgery (11 mo) compared with the no surgery SCC group (7 mo)[35]. Of note, patients who had not received neoadjuvant chemotherapy failed to benefit from resection for either tumour subtype[35]. Thus, when combined with neoadjuvant chemotherapy, surgery for the primary tumour is associated with improved survival in a select group of patients with metastatic oesophageal cancer[35].
Three of the patients in our series received chemotherapy alone for recurrent oligometastatic oesophageal cancer (patients 2, 6, and 11). Although chemotherapy is commonly considered as merely palliative in recurrent metastatic cancer, it also has the potential to cure[36]. Taxanes as single agents have a slightly higher response rate in patients with AC (34%) than in patients with SCC (28%), resulting in an overall survival rate of 13.2 mo[37]. Parryet al[38] reported complete tumour regression in 2 patients after chemotherapy alone, with both patients alive at last follow-up (35 and 112 mo)[38]. Developments in proton beam therapy and stereotactic ablative radiation increases its conformality and reduces radiation toxicity[39]. Sachdevaet al[40] recently reported on the use of external beam radiotherapy for the treatment of oligometastatic sacral metastases in a 46-year-old male with a rare case of primary oesophageal lymphoma[40]. Moreover, 1-year and 2-year progression-free survival and overall survival rates have been reported at 62% and 48% and 90% and 72%, respectively, following stereotactic ablative therapy for pulmonary metastases[41].
With few predictive factors for survival of metastatic oesophageal cancer in the literature[42], it is unclear which patients or which tumour characteristics predict the best survival outcomes. The current approach to metastatic disease all too often consigns the patient to palliative care and a dismal outcome. We have previously reported that bone marrow positivity for micrometastases at the time of oesophagectomy is a predictor of increased risk of cancer-related death and can identify patients requiring intensive surveillance for early detection of metastases with intent to treat[43]. Our current findings suggest that a more optimistic approach can be rewarded with impressive survival data. It is intuitive that aggressive treatment can improve survival, but it implies a need for more intensive surveillance strategies, especially in the first 3 years post-resection, to identify salvageable patients and consider curative intent. In an era of molecularly targeted agents, the identification of such patients is more important than ever as identified by the CheckMate 557 trial where the addition of nivolumab for patients with residual disease following CRT provided a median disease-free survival of 22.4 movs11.0 mo in the placebo arm, which was significant[44].
The obvious limitation of our study is the small sample size of patients with metastatic oesophageal cancer treated for cure. Moreover, the survival data reported in our study reflects a policy of aggressive treatment of confirmed limited metastases only. Such patients self-select, and our survival data cannot be applied to all patients with metastatic oesophageal cancer.
CONCLUSlON
In conclusion, as advances in imaging facilitate earlier metastatic disease detection and advances in multimodal and targeted treatments improve survival outcomes, surveillance strategies must be intensified to diagnose metastatic disease earlier in the recurrence process to institute medical or surgical measures with a greater possibility of success. Future studies are needed to prospectively identify the rate of oligometastatic recurrence in oesophageal carcinoma in the context of today’s imaging technologies to update surveillance and treatment guidelines in line with those for cancers of the lower gastrointestinal tract.
ARTlCLE HlGHLlGHTS
Research background
The prognosis of metastatic oesophageal cancer is poor. The rate of oligometastatic oesophageal cancer is not well established nor is the survival benefit of intervention. As a result, current guidelines advocate against a proactive approach, which is incongruent with other oligometastatic cancers such as colorectal cancer. Based on a policy of active postoperative surveillance and survival outcomes of patients with oligometastatic disease treated with curative intent at our institution, we advocate for more intensive surveillance strategies to identify patients with curative potential early and thus improve long-term survival.
Research motivation
To evaluate the impact of a policy of active surveillance and aggressive management of confirmed metastases on long-term survival.
Research objectives
To examine survival outcomes in patients who underwent active surveillance and targeted therapy of their oligometastatic disease, either at diagnosis or on follow-up surveillance, at our institution. When compared to incomplete clinical responders to neoadjuvant chemoradiotherapy (nCRT) for nonmetastatic oesophageal cancer who underwent surgery on their primary tumour, the median overall survival of the oligometastatic cohort was statistically significantly longer. These findings suggest that aggressive treatment of confirmed metastases can be rewarded with impressive survival data and that a more proactive approach to oesophageal oligometastases should be considered.
Research methods
A prospectively maintained database of patients diagnosed with oesophageal carcinoma and treated with curative intent in a single institution was interrogated for patients with metastases, either at diagnosis or on follow-up surveillance, and treated for cure. This cohort was compared with incomplete clinical responders to nCRT who subsequently underwent surgery on their primary tumour. Overall survival was estimated using the Kaplan-Meier method, and the log-rank test was used to compare survival differences between groups.
Research results
The overall survival of patients with oligometastatic disease who were treated for cure at our institution is impressive and statistically significantly longer than incomplete clinical responders without metastatic disease who subsequently underwent surgery on their primary tumour. These results suggest that intensive follow-up and aggressive management of confirmed metastases may improve long-term survival. Further studies are needed to prospectively identify the rate of oligometastatic recurrence in oesophageal carcinoma and evaluate the cost-benefit ratio of a policy of active surveillance and aggressive management of confirmed oligometastatic disease.
Research conclusions
In view of recent diagnostic and therapeutic advances, intensive follow-up and aggressive treatment of confirmed metastases may improve long-term survival in patients with oligometastatic oesophageal carcinoma.
Research perspectives
Further research should prospectively establish the rate of oligometastatic recurrence in oesophageal carcinoma to evaluate the cost-benefit ratio of active surveillance and aggressive management and inform future clinical guidelines.
FOOTNOTES
Author contributions:Walsh TN was the guarantor, designed the study, participated in the acquisition of data, and revised and edited the article critically; Pickett L acquired, analysed, and interpreted the data and drafted the initial manuscript; Dunne M statistically analysed the data and edited the manuscript; Monaghan O, Grogan L, and Breathnach O reviewed the article and made critical revisions related to important intellectual content.
lnstitutional review board statement:The study was reviewed and approved by the Connolly Hospital Institutional Review Board.
lnformed consent statement:As this was a retrospective audit and many patients were not alive at the commencement of this study, written informed consent was not feasible/obtained. This was an observational study, and no patient received treatment as part of the study. Furthermore, we have not included any identifiable patient information in our manuscript. Verbal consent, although not required, was obtained where appropriate/feasible.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:The statistical analysis and dataset are available from the corresponding author at lianne.pickett@ucdconnect.ie. As this was a retrospective audit consent was not routinely obtained but the presented data are anonymized, and risk of identification is low.
STROBE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Ireland
ORClD number:Lianne Pickett 0000-0001-5156-0612; Mary Dunne 0000-0002-3723-6311; Orla Monaghan 0000-0003-2902-528X; Oscar Breathnach 0000-0003-4852-0358; Thomas N Walsh 0000-0002-1600-8029.
S-Editor:Fan JR
L-Editor:Filipodia
P-Editor:Fan JR
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Prediction factors for ischemia of closed-loop small intestinal obstruction
- Successful treatment of acute symptomatic extensive portal venous system thrombosis by 7-day systemic thrombolysis
- Retrorectal mucinous adenocarcinoma arising from a tailgut cyst: A case report and review of literature
- Minimally invasive endoscopic repair of rectovaginal fistula
- Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis
- Effect of cardiac output - guided hemodynamic management on acute lung injury in pediatric living donor liver transplantation