Minimally invasive endoscopic repair of rectovaginal fistula
2022-10-11YiXianZengYingHuaHeYunJiangFeiJiaZiTingZhaoXiaoFengWang
Yi-Xian Zeng, Ying-Hua He, Yun Jiang, Fei Jia, Zi-Ting Zhao, Xiao-Feng Wang
Yi-Xian Zeng, Ying-Hua He, Yun Jiang, Fei Jia, Zi-Ting Zhao, Xiao-Feng Wang, Department of Proctology, Guang’anmen Ηospital, China Academy of Chinese Medical Sciences, Beijing 100053, China
Abstract BACKGROUND Surgical techniques for repair of rectovaginal fistula (RVF) have been continually developed, but the ideal procedure remains unclear. Endoscopic repair is a novel and minimally invasive technique for RVF repair with increasing reporting.AIM To review the current applications and preliminary outcomes of this technique for RVF repair, aiming to give surgeons an alternative in clinical practice.METHODS Available articles were searched according to the search strategy. And the sample size, fistula etiology, fistula type, endoscopic repair approaches, operative time and hospital stay, follow-up period, complication and life quality assessment were selected for recording and further analysis.RESULTS A total of 11 articles were eventually identified, involving 71 patients with RVFs who had undergone endoscopic repair. The principal causes of RVFs were surgery (n = 51, 71.8%), followed by obstetrics (n = 7, 9.8%), inflammatory bowel disease (n = 5, 7.0%), congenital (n = 3, 4.2%), trauma (n = 2, 2.8%), radiation (n = 1, 1.4%), and in two patients, the cause was unclear. Most fistulas were in a mid or low position. Several endoscopic repair methods were included, namely transanal endoscopic microsurgery, endoscopic clipping, and endoscopic stenting. Most patients underwent > 1-year follow-up, and the success rate was 40%-93%, and all cases reported successful closure. Few complications were mentioned, while postoperative quality of life assessment was only mentioned in one study.CONCLUSION In conclusion, endoscopic repair of RVF is novel, minimally invasive and promising with acceptable preliminary effectiveness. Given its unique advantages, endoscopic repair can be an alternative technique for surgeons.
Key Words: Endoscopic repair; Minimal-invasive technique; Rectovaginal fistula
lNTRODUCTlON
Rectovaginal fistula (RVF), a type of chronic gastrointestinal fistula, refers to an abnormal epithelializedlined connection between the rectum and the vagina, presenting with symptoms including uncontrollable passage of gas and/or fecal discharge from the vagina[1]. Even though it is benign, the distressing and persistent symptoms interfere with daily activities and sexual life, and have a long-term potential detrimental impact on psychological health[2,3]. Obstetric trauma is the primary etiological factor for RVF, but it can also be acquired from local abscess, pelvic floor or rectal surgery, trauma, or radiotherapy[3-5]. Chronic inflammatory bowel disease (most commonly Crohn’s disease) is the second most common etiology with rates varying between 6% and 23%[6]. It is reported that RVF occurs in up to 10% of women diagnosed with Crohn’s disease[7,8]. Congenital RVF is rare, usually coexists with anal malformation, and can be treated by anal reconstruction at a young age[9].
Standard classification of RVF will benefit to the choice of treatment approach and the comparison of treatment outcomes between studies, and help develop an algorithm for repair. However, there is no generally accepted classification of RVF. Currently, the classification of “simple/complex” or “low/ middle/high” according to location, size, and etiology of RVF is most used[10,11]. With the development of diagnostic and therapeutic techniques, the imaging results, endoscopic exploration and gradually defined local anatomical structure will promote a classification consensus[12,13]. The anatomical features are always the principle of classification, which makes it necessary to achieve a more detailed and precise anatomical recognition[14].
Various medical and surgical treatments have been applied for RVF, but treatment is still a challenge for doctors due to the high recurrence rate. Nonoperative methods are recommended for the treatment of fresh and slight symptomatic fistula. Surgical repair is essential, once it occurs and persists[15]. There is still no standard surgical repair technique worldwide for RVF and no evidence can suggest one surgical technique over another since the release of the procedural guidelines in Europe.
Multiple surgical repair techniques, including fistulectomy, advancement flap, muscle transposition, closure with biomaterials, endoscopic repair and transabdominal approaches[16], have been gradually reported in the literature. Fistulectomy is not technically demanding, whose main step is to remove the fistula tract, together with the surrounding scarred and sclerotic tissue. It may fail due to incomplete removal and excessive tissue tension of tissue suture for large excision, and is therefore, mostly used to repair small and simple RVFs[17,18]. Advancement flaps are performed by raising either the rectal mucosa (transrectal) or vaginal mucosa (transvaginal) to cover the fistula tract. Transrectal advancement flap is more commonly adopted compared to the transvaginal approach, and the repair is performed from the high pressure of the rectum side, and has an actual success rate of 50%-70%[1,4]. Even though some studies have recommended transrectal advancement flap as the first-line treatment for low RVFs, it is not as effective as expected if the periorificial tissue is chronically inflamed, or when the fistula is large in diameter and causes anal stenosis[19]. Reconstruction by Martius flap, gracilis muscle flap or bulbocavernosus muscle transposition can be used to introduce healthy vascularized tissues, which has achieved a certain effect for recurrent, Crohn’s-disease-related and radiation-related RVFs, with reported overall success rates ranging from 25% to 100%[20,21]. However, given the aggressive incision, tissue damage, prolonged hospital stay and protective stoma diversion routinely required, this technique is demanding and not easily accepted by patients[22,23]. Biomaterials and endoscopic repair are novel and less invasive techniques and constant attempts have been made to apply them for RVF repair. However, given the limited number of publications available, there are currently no relevant recommendations. Transabdominal approaches are recommended for high RVFs resulting from complications of colorectal anastomosis, and laparoscopic repair has been frequently adopted[15,24]. In clinical practice, protective stoma diversion is generally applied for the treatment of RVF, whereas absence of any reliable efficacy assessment for RVF makes it remain controversial. Theoretically, diversion stoma may help control the symptoms by fecal diversion and support healing of the fistula and surgical success[25]. Corteet al[26] claimed that a temporary diversion stoma could significantly improve the success rate of repair. However, Lambertzet al[27] found no connection between diversion stoma creation and rate of recurrence, which was supported by other authors[28,29]. Some studies have shown that radiation- and Chron’s-disease-related RVFs are indications for diversion stoma[30,31], and stating that once the diversion stoma is made, large invasion, distressing conditions and potential complications can occur[32]. Although the techniques for RVF repair have been developing, the etiology, classification, surrounding tissue condition, prior treatment procedures and the surgeon’s preference are always the basis for determining the approach. In addition, individualized, precise, and less-invasive surgical techniques for RVFs repair are gradually being recommended[13,33].
All the surgical interventions performedviaan endoscope or in the endoscopy unit can be classified as endoscopic repair, which is a novel and minimally invasive surgical technique for RVF. Several endoscopic repair approaches have been applied and reported for RVF surgical treatment. Transanal endoscopic microsurgery (TEMS) is an endoscopic technique performed entirely through the anus and rectum, which was originally developed in the 1980s to treat lower rectal adenomas[34] (Figure 1). Vávraet al[35] reported the first case of RVF treatment using TEMS in 2006, which is one of the most reported endoscopic approaches for RVF. Several minimally invasive endoscopic approaches such as the through-the-scope clip (TTSC), over-the-scope clip proctology system (OTSC) and endoscopic stenting have successively proven their role in RVF repair. After more than a decade of development, endoscopic repair for RVF has been continuously advanced and more advantages have been unveiled. Endoscopic repair for RVF is novel but limited by the information available. Therefore, a review of studies on minimally invasive endoscopic repair for RVF was carried out to assess the preliminary outcomes and introduce several endoscopic approaches for RVF surgical repair to surgeons, thereby contributing to developing a more individualized, precise, and less-invasive treatment plan appropriate for each patient.
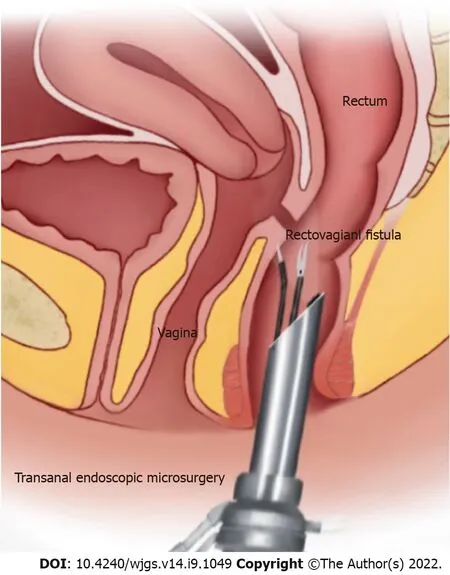
Figure 1 Transanal endoscopic microsurgery for rectovaginal fistula repair.
MATERlALS AND METHODS
A search was performed to identify the existing literature available in PubMed and EMBASE databases in December 2021, without timeframe limitations (Figure 2). The following keywords, including “rectovaginal fistula,” “rectovaginal,” “fistula,” “endoscope”, “endoscopic,” and “endoscopy”, were used for searching. Given that there were only around 184 articles available, every single article was reviewed at the beginning. Exclusion criteria included irrelevancy, not English language, guidelines, or reviews. Articles published by the same author were found a duplication in the inclusion of patients, and the study with the longest follow-up was included. Three independent reviewers extracted and summarized data from the included articles and conducted qualitative assessment in accordance with the Oxford Centre for Evidence-Based Medicine 2011 Level of evidence[36]. All disagreements were settled by consensus. In addition, we conducted a research using Reference Citation Analysis (https://www.referencecitationanalysis.com/) and cited the relevant references.
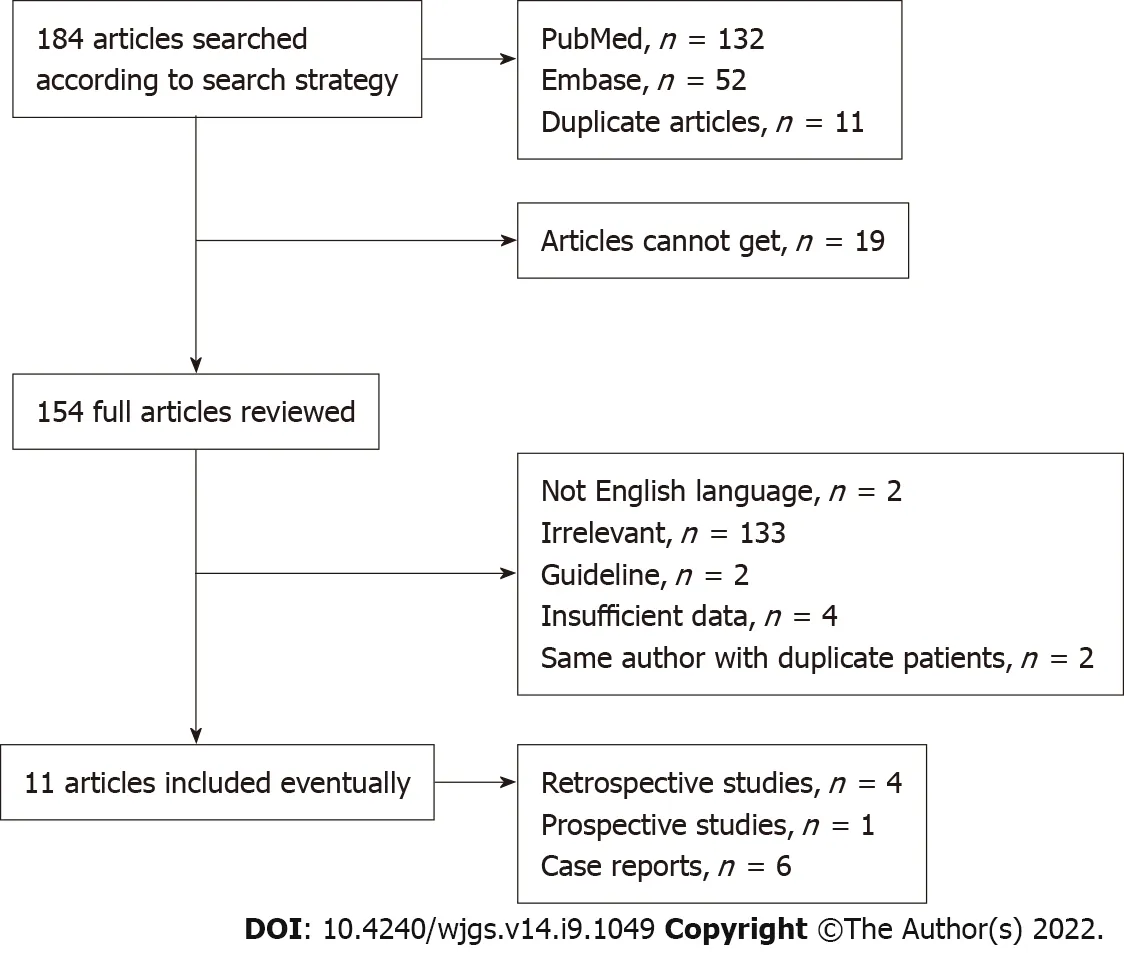
Figure 2 The search strategy.
RESULTS
A total of 11 articles were eventually identified according to the search strategy. Data were extracted by the reviewers and eventually reported using summary statistics, as shown in Table 1. The limited number of available articles and the low evidence of all studies made the primary outcome not sufficiently satisfactory. Besides, there were not enough eligible articles to perform a meta-analysis. In terms of the type of study, case reports seemed to be preferred for this novel technique, and the number of patients in each retrospective study was limited. The etiology was classified as: related to surgery (n= 51) such as rectal surgery, pelvic surgery and the colorectal anastomosis,etc., with 22 patients undergoing rectal surgery with a history of radiotherapy; and directly caused by radiotherapy (n= 1), inflammatory bowel diseases (n= 5) including Crohn’s disease and ulcerative colitis; congenital (n= 3), obstetric injury (n= 7), trauma (n= 2), with the etiology unclear in two patients. Most fistulas were situated in the middle or low. Most of the patients had undergone previous repairs, even on multiple occasions. Fecal diversion was chosen as part of surgical treatment in some patients. Psychological components regarded as important as the success rate were rarely reported[19,37], with improved sexual function after repair mentioned in only one paper.
Table 2 summarized the details and preliminary outcomes of endoscopic repair of RVFs. A total of 38 patients underwent the conventional surgical procedure with a transrectal endoscopic device, when the layered suture was closed for 24, and mucosal advancement flap was for 14 patients. Endoscopic clip was another commonly used approach for RVF repair, and 18 patients who were treated using this technique benefited from TTSC (n= 2) and OTSC (n= 16). One retrospective study reported endoscopic repair with placement of a self-expandable metal stent (n= 15). Several other endoscopic repair approaches for RVF such as endoscopic plugs, endoscopic injection and endoscopic-laparoscopic combined approach were noted, which were removed due to no complete references. Operating time and hospital stay were the desired outcomes, but not frequently reported. Most patients underwent > 1 year of follow-up. All case reports reported successful outcomes, but the success rates were different (40%-93%) in retrospective case series. More than half the studies reported no severe complications, and a few reported some minor postoperative complications, such as hematoma or abscess of rectovaginal septum (n= 2), moderate sphincter hypotonia (n= 1), pain (n= 5), minimal vaginal flatus (n= 1).
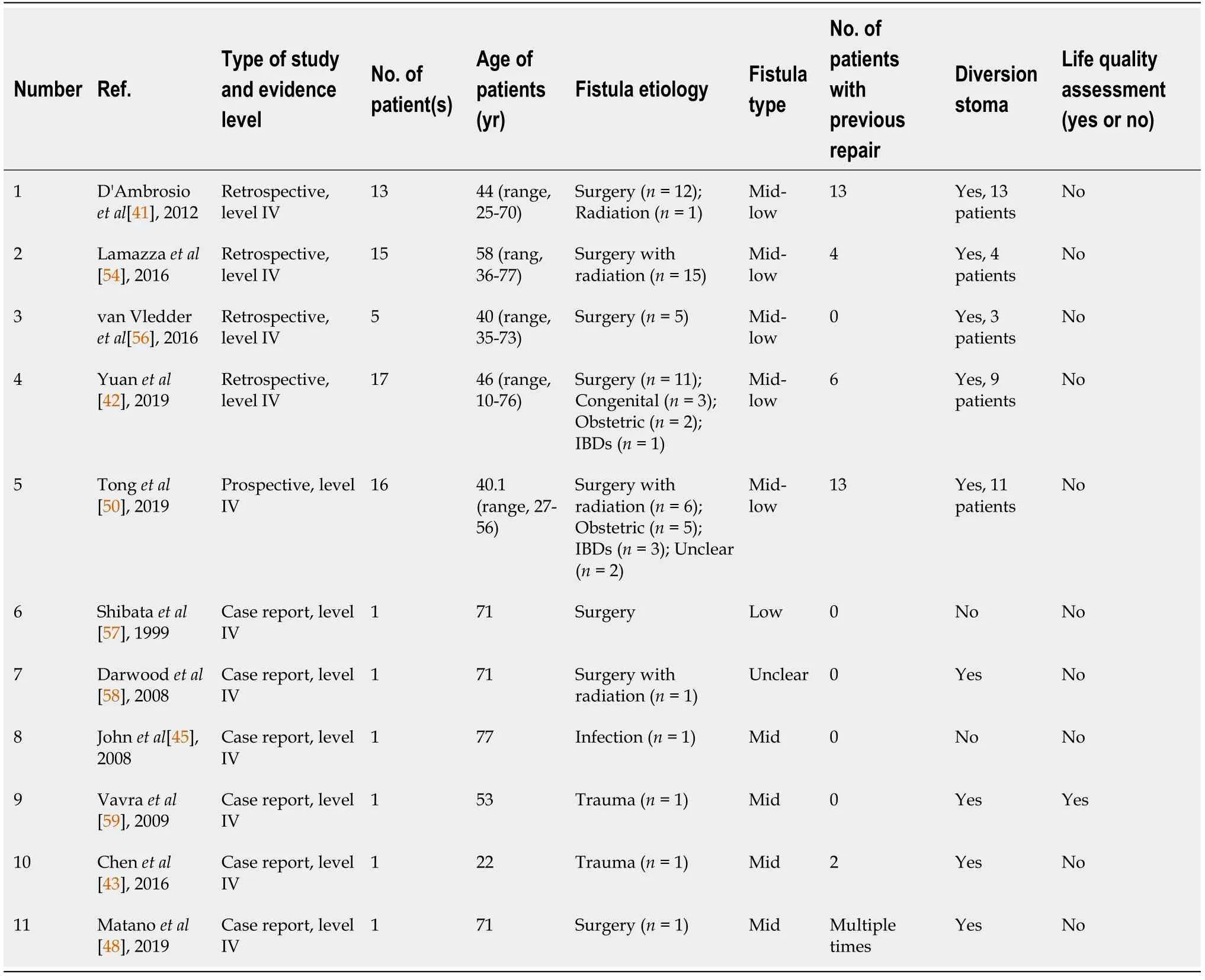
Table 1 Extract data of studies included
Minimally invasive endoscopic repair
TEMS:Minimally invasive techniques have been one of the major advancements in surgery in the last few decades, and are also one of the future trends. Such a technique has been almost routinely performed in colorectal resection irrespective of underlying diseases[38]. With the development of surgical instruments, endoscopic surgery is considered a feasible and minimally invasive approach that can facilitate better exposure, direct visualization and precise operation, with an increasing number of surgeons choosing it[39]. TEMS, as a platform for natural orifice transluminal endoscopic surgery, has developed into a well-established method of accurate resection of specimens from the rectum under binocular vision after the initial application for rectal cancer, and has also been adopted as an operative intervention in an extended setting for RVF[40]. After the first case of TEMS for RVF repair reported in 2006[35], the first retrospective review with 13 patients who had undergone layered suturesviathis repair technique was published in 2012, with a closure rate of 93%[41]. In the present review, more than half of patients (n= 38) underwent conventional surgical repair procedures with transanal endoscopic devices, with a success rate of 40%-93%. The latest study reported a closure rate of 82% of mid-low RVF TEMS with layered sutures and mucosal advancement flaps[42]. Another three cases all reported successful closure. The superior 3D exposure and direct vision were the greatest advantages of TEMS. Under good visualization, comprehensive procedures exploring the anatomical structural relationship could be provided preoperatively and intraoperatively. The conventional invasive procedure could be performed more accurately with TEMS equipment, and ensure complete removal of the surrounding scarred or granulomatous tissues, but without significant loss of normal tissue. Therefore, there was a greater certainty of adequate blood supply to the tissue overlaps and/or flaps owing to the fresh tissue with the healthy margins[42]. In addition, the smaller tissue defect and good control of suture tightness enable free-tension repair[43], and make up for the shortcomings of conventional local repair that cannot completely remove surrounding tissue and is subject to insufficient blood supply and prompt healing. Using a natural endoluminal approach with endoscopy, precise operation and visualization can greatly reduce the invasiveness of conventional surgery with less intraoperative bleeding, shorter operating time and hospital stay, and fewer postoperative complications.
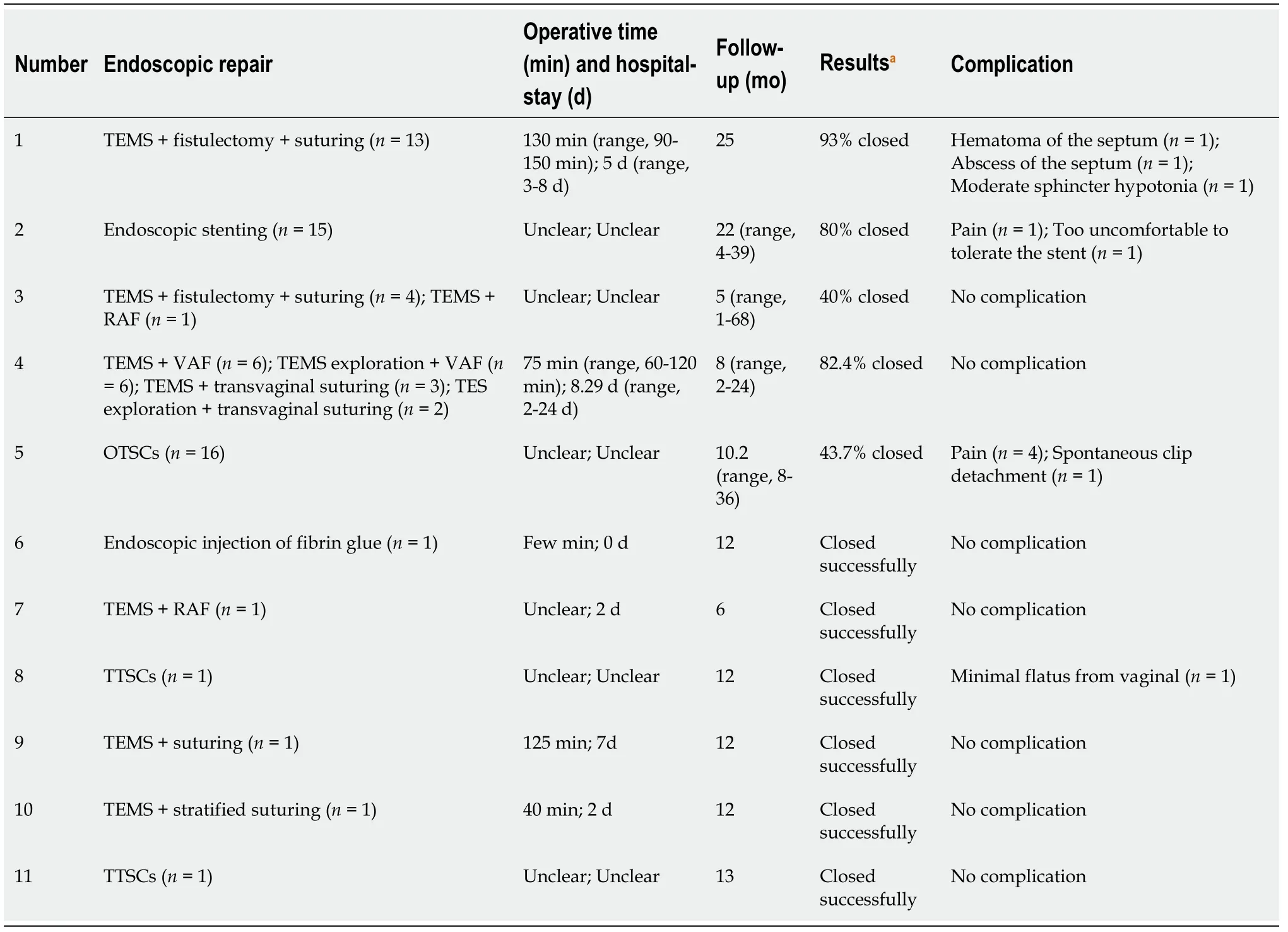
Table 2 Details and results of the endoscopic repair approaches for rectovaginal fistulas
Endoscopic clipping:Endoscopic clipping is another technology using endoclips to completely close gastrointestinal leaks and fistulas, initially applied for iatrogenic gastric perforation in 1993[44]. Johnet al[45] reported the first successful closure of an RVF with TTSCs, which was also applied for repair of refractory RVF[33]; Ortiz-Moyanoet al[46] described a combined approach using TTSCs and tissue adhesive that improved the rate of technical success in the endoscopic clips treatment of RVFs, since clips not only worked in opposing the margins, but acted as a scaffold for the glue. OTSCs for the gastrointestinal tract had greater force and a consistently high mean rate of procedural success of 80%-100%, and a durable clinical success rate of 57%-100%, and was preferred over TTSCs for closure of gastrointestinal fistulas[47]. Regarding colon perforation, small perforations (< 10 mm) could be successfully closed with TTSCs, whereas larger perforations could be successfully closed with OTSCs[48]. The first RVF closure using the OTSC proctology system was performed by Prosstet al[49] in 2015. One prospective study in 2019[50] presented the first evaluation of the therapeutic effects and safety of the application of OTSCs in complex RVFs, with a success rate of 43.7%, which was as high as that for gastrointestinal fistulas and convincing for complicated ones. Endoscopic clipping is a minimally invasive technique that involves transrectal placement of endoclips for RVF closure to avoid tissue incision, sphincter damage and intraoperative bleeding[49]. It is considered suitable for small fistulas, and is even recommended to repair high-level fistulas[45,48]. Given limited data and obtained evidence, the role of endoscopic clips in RVF repair remains to be further investigated.
Endoscopic stenting:Endoscopic stenting involves placement of a self-expandable metal stent into the gastrointestinal tract to treat the defects, especially anastomotic leaks or perforation of the upper gastrointestinal tract[51]. Endoscopic placement of the self-expandable metal stent to treat RVFs after colorectal resection for cancer was a useful alternative to divert colostomy for the palliation of malignant rectal obstruction[52]. The team presented the two series outcomes with a success rate of 83% (5 of 6 patients)[53] and 80% (12 of 15 patients)[54], and the fistula size decreased significantly in all remaining patients, indicating that endoscopic placement of self-expandable metal stents may be a valid adjunctive treatment of RVF after colorectal resection for cancer. However, the favorable results may have been due to the low number of patients and selection bias. In the selected cases, the endoscopic placement of the self-expandable metal stent for RVF repair showed that the endoscopic stenting allowed a fast and proper closure of the fistula in a minimally invasive endoscopic way, with minor discomfort for patients and early discharge. A clear indication and results are still required for further in-depth study.
DlSCUSSlON
Surgical outcomes of RVF repair are mostly measured by the rates of closure and reoperation[37]. The successful closure rates for RVF surgical repair vary in the literature[55]. A similar variation in success rate (20%-93%) was found in this study using different etiologies and endoscopic approaches. We acknowledge that the varying rate of successful closure, limited number of publications available on this novel technique, and the low quality of included studies were limitations of the present review. In addition, the indications for endoscopic repair for RVF are not clear due to the lack of high-quality clinical studies. From a review of the included literature, endoscopic repair for RVF seems to be more commonly used in the treatment of low- and mid-level fistulas. However, it is also used for high-level fistulas with small openings, because transabdominal surgery is an invasive approach for small fistulas; therefore, endoscopic repair is considered a viable minimally invasive approach[48]. Moreover, endoscopic repair is a promising option for primary repair of RVF, and can be recommended for treatment of recurrent fistulas as well[50]. Regarding endoscopic repair is performed locally, it is not suitable for refractory RVFs with large openings and excessive tissue defects. Nevertheless, the minimally invasive endoscopic approach for RVF repair is a promising choice, and more surgical methods could be developed based on the endoscopic technique. As the research progresses, more indications should be unveiled as well.
A 2014 systematic review claimed that the reason for difficulties in formulating a conclusion about the best surgical technique for RVF repair was the disappointing quality of existing literature surrounding different surgical techniques and outcomes for RVF repair[16]. Such a result not only persisted in the present review, but also in some related to single surgical approaches[8,20]. On the one hand, the limited number of samples and the heterogeneity of etiologies and local conditions made it hard to design large studies. RVF is a benign and chronic disease without a high incidence, but subject to variable and complex causes. There is no doubt that compared to the sample iatrogenic etiologies, IBDs-or radiation-related RVF would make difference in the local condition and the selection of surgical techniques. Therefore, retrospective studies were reviewed carefully to ensure the study sample size and homogeneity. With the continuous advancement of endoscopic techniques, different surgical procedures can be applied and standardized, which may improve the homogeneity of the surgical devices and contribute to designing large studies. On the other hand, in terms of the precise anatomical relationship of the fistula defect and the surrounding tissue, the lack of consensus on classification of RVFs makes it difficult to compare different surgical techniques. It is therefore proposed that further revisions are needed to guide the choice of newly developed treatment approaches[19]. Additionally, some authors claimed that a precise preoperative anatomical relationship assessment allowed better classification of fistulas and comparisons among different techniques[14]. It is believed that diagnostic imaging and endoscopic exploration could play a role in clarifying and developing anatomical relationship standards.
CONCLUSlON
Endoscopic repair for RVFs is novel, effective and promising. A precise operation under good visualization through a natural lumen can reduce the invasiveness of conventional procedures. Some endoscopic surgical modes such as clipping and stenting mentioned in this review could even close the fistula without incision, less intraoperative bleeding, fewer complications, and shorter operating time and hospital stay. Surgeons could clarify the anatomical relationship of the fistula and surrounding tissue by endoscopic preoperative exploration and provide patients with a more appropriate treatment approach. However, endoscopic surgical repair for RVFs is technically demanding with a long learning curve and requires sufficient professional experience. Therefore, it is advocated to be performed by professional colorectal surgeons in highly specialized centers. Besides, larger high-quality studies and longer follow-up studies are necessary to unveil the clear indication and advantages of this novel minimally invasive endoscopic technique for RVF repair.
ARTlCLE HlGHLlGHTS
Research background
Rectovaginal fistula (RVF) is abnormal connection between the rectum and vagina. Surgical repair is essential, once it occurs and persists. Surgical techniques for repair of rectovaginal fistula have been continually developed, but the ideal procedure remains unclear. Endoscopic repair is a novel and minimally invasive technique for RVF repair with increasing reporting.
Research motivation
To review the current literature of endoscopic repair of RVF and highlight the novel and minimally invasive technique for RVF repair to surgeons.
Research objectives
To evaluate the preliminary outcomes of this technique for RVF repair and analyze the indication and technical superiority.
Research methods
We searched PubMed and EMBASE databases for available studies. Data were extracted and qualitative assessment was conducted.
Research results
The endoscopic repair of RVF is in constant development, including several available approaches. The preliminary effectiveness of endoscopic technique for RVF repair is acceptable.
Research conclusions
Endoscopic repair for RVF is novel, effective and promising with acceptable preliminary effectiveness.In this manuscript, we have provided a detailed review of literatures, summarized its indications and unique technical advantages and made suggestions for its application and future development.
Research perspectives
Endoscopic repair for RVF is effective and safe according to preliminary outcomes. It is a promising technique for the treatment of rectovaginal fistulas and provides a minimally invasive technique selection for surgeons to treat rectovaginal fistulas.
FOOTNOTES
Author contributions:All authors contributed to this manuscript; Zeng YX, Wang XF and He YH designed the outline of this review; Zeng YX performed most of the writing, and prepared the figures and tables; Wang XF and He YH made critical revision of the manuscript for important intellectual content; Jiang Y, Jia F and Zhao ZT performed data acquisition, and writing; All authors read and approved the final version.
Conflict-of-interest statement:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
PRlSMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yi-Xian Zeng 0000-0002-9219-9103; Ying-Ηua Ηe 0000-0002-8970-4519; Yun Jiang 0000-0002-4449-2137; Fei Jia 0000-0002-4114-492X; Zi-Ting Zhao 0000-0003-4023-0006; Xiao-Feng Wang 0000-0001-6053-8177.
S-Editor:Zhang H
L-Editor:A
P-Editor:Zhang H
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Prediction factors for ischemia of closed-loop small intestinal obstruction
- Successful treatment of acute symptomatic extensive portal venous system thrombosis by 7-day systemic thrombolysis
- Retrorectal mucinous adenocarcinoma arising from a tailgut cyst: A case report and review of literature
- Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis
- Effect of cardiac output - guided hemodynamic management on acute lung injury in pediatric living donor liver transplantation
- Blood index panel for gastric cancer detection