Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis
2022-10-11NoemiZorzettiAugustoLauroMariaIreneBelliniSamueleVaccariBarbaraDallaViaMaurizioCervelleraRobertoCirocchiSalvatoreSorrentiVitoAndreaValeriaTonini
Noemi Zorzetti, Augusto Lauro, Maria Irene Bellini, Samuele Vaccari, Barbara Dalla Via, Maurizio Cervellera,Roberto Cirocchi, Salvatore Sorrenti, Vito D’Andrea, Valeria Tonini
Noemi Zorzetti, Department of General Surgery, Ospedale Civile A Costa, Porretta Terme 40046, Italy
Noemi Zorzetti, Augusto Lauro, Maria lrene Bellini, Samuele Vaccari, Salvatore Sorrenti, Vito D’Andrea, Department of Surgical Sciences, Sapienza University, Rome 00161, Italy
Samuele Vaccari, Department of General Surgery, Ospedale di Bentivoglio, Bologna 40010, Italy
Barbara Dalla Via, Valeria Tonini, Department of Emergency Surgery, St Orsola University Ηospital, Bologna 40138, Italy
Maurizio Cervellera, Department of General Surgery, Ospedale Santissima Annunziata, Taranto 74121, Italy
Roberto Cirocchi, Department of General Surgery, Ospedale di Terni, Università di Perugia, Terni 05100, Italy
Abstract BACKGROUND Acute appendicitis (AA) is one of the main indications for urgent surgery. Laparoscopic appendectomy (LA) has shown advantages in terms of clinical results and cost-effectiveness, even if there is still controversy about different devices to utilize, especially with regards to the endoloop (EL) vs endostapler (ES) when it comes to stump closure.AIM To compare safety and cost-effectiveness of EL vs ES.METHODS From a prospectively maintained database, data of 996 consecutive patients treated by LA with a 3 years-follow up in the department of Emergency General Surgery - St Orsola University Hospital, Bologna (Italy) were retrieved. A metaanalysis was performed in terms of surgical complications, in comparison to the international literature published from 1995 to 2021.RESULTS The meta-analysis showed no evidence regarding wound infections, abdominal abscesses, and total post-operative complications, in terms of superiority of a surgical technique for the stump closure in LA.CONCLUSION Even when AA is complicated, the routine use of EL is safe in most patients.
Key Words: Acute appendicitis; Laparoscopic appendectomy; Endoloops; Stapler; Post-operative complications
lNTRODUCTlON
Acute appendicitis (AA) is one of the most frequent causes of acute abdominal pain and access to emergency care department. The lifetime chance of developing AA is lower in women, and the risk of being subject to surgery is higher in males[1], representing in fact one of the main indications for an urgent operation. Surgery is generally performedviaa laparoscopic approach, and given the high volume of AA procedures worldwide, it represents a training operation as well[2].
Laparoscopic appendectomy (LA)[3,4] is demonstrated to be superior in terms of clinical results[5-9] and cost-effectiveness[10-14], even if there is still controversy[15-19] about the use of different devices during the operation[20-24]. Currently, it is still debated the use of endostapler (ES)vsendoloop (EL) in appendiceal stump closure[25-28]. The routine use of EL is safe in most patients affected by AA, also when it is complicated[29-32], representing a cost-effective device when taking into consideration the additional costs of potential post-operative complications, too[33-37]. We have previously shown money saving as well as the safety of the routine use of ELs[38]. The aim of this study is to meta-analyze the international literature, to compare the outcome of the patients laparoscopically treated in BolognaviaEL to the data from the international literature.
MATERlALS AND METHODS
Between November 2011 and January 2018, a total of 1045 LAs were performed in the department of Emergency General Surgery - St Orsola University Hospital, Bologna (Italy). Patients who undergone LA until January 2018 were identified retrospectively from a prospectively maintained database, so that a 3-year follow-up was achieved[39,40]. All grades of post-operative complications were collected and examined. Institutional review board for this study was not required, as this is a meta-analysis of already previous published data. At Bologna centre, patients were initially evaluated by a general surgeon, then underwent laboratory tests, and Alvarado or appendicitis inflammatory response (AIR) score (Table 1) were calculated in females and in males respectively[41,42].
Surgery
Surgical procedures were performed by attendants or supervised trainees. Written informed consent was signed by all the patients before the procedures. Antibiotic prophylaxis was always administered. A supraumbilical 12 mm-Hasson trocar with an open approach was adopted to induce pneumoperitoneum and initiate laparoscopy. Then, 2 other operative trocars were placed in the left flank (10 mm) and suprapubic position (5 mm), with identification of the appendix, cut and coagulation of the mesoappendix.

Table 1 Alvarado and appendicitis inflammatory response score
EL or ES use
The choice of ELvsES to close the base of the appendiceal stump was made by the operating surgeon, after evaluating the inflammatory infiltration of the appendicular base[43]. If an EL was used, the appendicular stump was cut 3-5 mm away from cecum. The surgical specimen was then removed in an endobag through the 12 mm trocar.
Bologna cohort
Patients were divided in two groups (EL and ES) and in three categories (edematous, phlegmonous and gangrenous appendicitis) based on the severity of the histological examination. Cases requiring conversion to open appendectomy were excluded, while 996 LA (95.3%) were included in the metaanalysis.
Meta-analysis
A meta-analysis was performed in terms of surgical complications, comparing the clinical data of the EL group (821 patients) to the international literature retrieved by Pubmed (Figure 1), according to the PRISMA principles[44].

Figure 1 PRlSMA diagram.
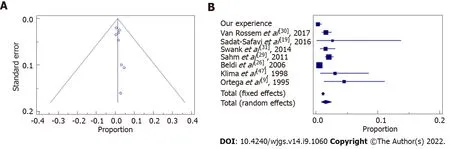
Figure 2 Wound infection Funnel plot. A: Asymmetrical distribution among both sides indicates that bias can be present; B: The confidence interval (diamond) confirms there is no statistically significant result.
Inclusion and exclusion criteria
Manuscripts were excluded from the analysis if they dealt with pediatric patients (< 15 years of age) or were published before 1995.
Statistical analysis
Data were collected and analyzed with MedCalc software. Statistical expertise was available to the authors. MedCalc 13.0.6.0 (MedCalc Software bvba, Østend, Belgium) was used for the meta-analysis. MedCalc uses a Freeman-Tukey transformation (arcsine square root transformation) to calculate the weighted summary proportion under the fixed and random effects model. The program lists the proportions (expressed as a percentage), with their 95% confidence interval (CI), found in the individual studies included in the meta-analysis. The heterogeneity was evaluated by means of statistics Cohran’s Q and I2. The results of the different studies, with 95%CI, and the pooled proportions with 95%CI are shown in a forest plot. Bias was detected using a funnel plot. Publication bias results in asymmetry of the funnel plot.P< 0.05 was considered statistically significant.
RESULTS
Meta-analysis of clinical outcome in EL patients and comparative results
The sample of our study consisted of all our patients treated with EL for a total of eight hundred twenty-one patients (Table 2), corresponding to the 78.5% of all LAs. Post-operative complications in this group of interest were collected (Table 3) and reported according to the Clavien-Dindo classification[45,46] (Table 4). These data were then compared to those retrieved from the manuscripts finally considered in the analysis[9,19,26,29-31,47] (Table 5), in fact other four papers that were initially assessed and that were from the last 3 years[48-51], were not included, because of the lack of information and partial numbers and percentages of patients with wound infections, abdominal abscesses and total post-operative complications.

Table 2 Groups and categories of severity of Bologna patients

Table 3 Post-operative complications in Bologna endoloop group

Table 4 Post-operative complications in Bologna 996 laparoscopic appendectomy patients
Examination of the seven papers involved in the meta-analysis[9,19,26,29-31,47] showed that only Beldiet al[26] were in favor of application of an ES for transection and closure of the appendiceal stump in patients with AA. In their report it lowered the risk of postoperative intra-abdominal surgical-site infection and the need for readmission to hospital. All the other 6 papers didn’t find a statistically significant difference for intra or postsurgical complications, length of stay (LOS), wound infections, and abdominal abscesses among different groups of patients. Sahmet al[29] and Van Rossemet al[30] clearly stated that infectious complication rate is not influenced by the type of appendicular stump closure, either if performed by EL or ES, and routine stump closure using an EL is an easy, safe, and costeffective procedure. Finally, it is important to mention the retrospective cohort study conducted by Swanket al[31] that compares the two strategies for closure of the appendiceal stump. The routine use of the ES showed no clinical advantages over the use of ELs.
Statistical data and results showed that our experience followed the trend of the evidence in literature in terms of wound infections (Figure 2 and Table 6), abdominal abscesses (Figure 3 and Table 7) and total post-operative complications (Figure 4 and Table 8). The meta-analysis proved a wide heterogeneity among analyzed groups, as the funnel plots and the forest plots confirmed. Tables 6-8 report data related to the standard deviation of wound infection, abdominal abscesses, and post-operative complications, respectively. Figures 2A, 3A and 4A are Funnel Plots showing an asymmetrical distribution of the articles (dot) among both sides indicating that bias can be present. In Figures 2A and 4A, few papers are near the middle solid line, indicating the overall effect from the meta-analysis, possibly in relation to the limited size of the samples. Figures 2B, 3B and 4B Forrest Plots prove there is no statistically significant result in favor of ES or EL for the overall incidence of wound infections, abdominal abscess, or post-operative complications.

Figure 3 Abdominal abscess Funnel plot. A: With asymmetrical distribution among both sides, indicating that bias can be present; B: The confidence interval (diamond) confirms there is no statistically significant result favoring endoloop or endostapler.

Figure 4 Post-operative complications Funnel plot. A: Asymmetrical distribution among both sides indicates that bias can be present; B: The confidence interval (diamond) confirms there is not statistically significant difference between endoloop vs endostapler.

Table 5 Complete data to meta-analyse

Table 6 Wound infection: Data standard deviation in the meta-analysis
DlSCUSSlON
Appendectomy is one of the most performed emergency surgery procedures. The laparoscopic approach is recognized and recommended internationally, but a matter of debate during the operation is the choice of the different available devices to close the appendicular stump, in consideration of the possible consequent leak leading to infection and postoperative complications.
Already previously[38], we evidenced that the routine use of EL is safe in most patients affected by AA, including cases with signs of complications. Furthermore, it is a cost-effective device, even when possible additional costs secondary to the occurrence of adverse events in the post-operative course are included. Conversely, Laseket al[48] assessedviaa multicenter observational study the stump closure only in patients affected by complicated AA. Their results highlighted some clinical benefits of ES use, but EL was superior in terms of overall morbidity and LOS, with no statistically significant difference in major complication rates and postoperative intra-abdominal abscess formation.

Table 7 Abdominal abscess: Data standard deviation in the meta-analysis

Table 8 Post-operative complications: Data standard deviation in the meta-analysis
In literature, two papers systematically analyzed the techniques for appendiceal stump closure during LA[49,50]. Ceresoliet al[49] meta-analysed randomized trials and cohort studies comparing ES with endoscopic loop ties for the closure of the appendicular stump in LA, including pediatric patients and complicated AA, such as gangrenous/necrotic appendix or the perforated ones. In their analysis, ES was associated with a similar intra-abdominal abscess rate, but a lower incidence of wound infection, while LOS, readmission and reoperation rates were similar. In a subgroup analysis ES significantly reduced the wound infection rate in pediatric patients, while no difference in the main outcomes was observed in patients with complicated AA.
Makaramet al[50] performed a systematic review evaluating all methods of stump closure (ELs, polymeric endoclips, metallic endoclips, endosuture and ES). In this study[50], no difference in complication rate, LOS or cost was found. According to their analysis, endoclips provide the most timeefficient method of closure, although not statistically significant; closure by endosuture, represents the cheapest method, but it is hindered by a high complication rate. Current evidence suggests endosuture should then be avoided. ESs appear very safe and effective for stump closure, however they seem to be associated with high postoperative complication rates; furthermore, the consequent cost limits their use to the most severe cases of appendicitis, while instead EL provides a valuable alternative for closure, with a risk of intraoperative complications of 4.61%.
Another recent retrospective cohort study[51], whose subject was to determine the safety and efficiency of the use of EL and ES in complicated and uncomplicated AA, concluded that the systematic use of EL could reduce costs in uncomplicated appendicitis, while in complicated cases both options (loop and stapler) are valid. Also a prospective randomized clinical trial[52] and a retrospective study[53] recently analyzed the technical aspects of appendix stump closure: Ihnátet al[52] reported similar postoperative morbidity and safety following the use of EL, ES or hem-o-lok and even Whiteet al[53] demonstrated non univocal superiority of one technique over the others, too.
Another point indeed to be considered is LA availability together with the fact that the different devices rely upon the resources of the hospital and the country where surgery is performed, pending possible spending reviews carried out by the government. It has been demonstrated that LA is performed more frequently in high-income countries in comparison to low-income countries (67.7%vs8.1%), with better postoperative outcomes[54]. The difference in the costs of the used surgical devices (above all stapler) represented a principal determinant for the overall economic impact of the surgical procedure in some recent reports[33,36,38,50,51], to highlight how important is the cost-effectiveness in the measured outcomes. The medium saving reported in the present paper is relevant, varying from around approximately 300 € to more than 500 € just for the device, which then must be multiplied for the many LA conducted worldwide; further cost-analysis including operative time and LOS could reach major savings.
Our study presents some limitations: The design is a retrospective analysis to investigate the safety of ELs, then the results are pooled with other reports; the comparison between studies is difficult due to heterogenous patient selection and outcomes measured. However, EL seems to have the potential for being a safe and cost-effective device.
CONCLUSlON
In conclusion, there is no evidence clearly illustrating a superior surgical method for performing stump closure in LA. Given that comparison between studies is difficult due to heterogeneous patient selection and measured outcomes, our meta-analysis shows that the data of our sample, related to wound infections, post-operative abdominal abscesses, and total post-operative complications, mirror current literature trend. The routine use of EL is safe in most patients affected by AA, even when complicated, and these findings could have above all more relevance in lower resource environments that may not have easy access to ES. Prospective studies are needed to analyze a greater number of patients and taking into account an accurate grading system for AA severity such as Disease Severity Score[55], Alvarado Score[41], AIR Score[42] or imaging severity scoring, such as the CT-Determined Severity Score[56]. Their aim should be first to stratify preoperatively the grade of AA and secondly to observe differences in postoperative complications. Finally, studies aiming at an accurate cost analysis are required, ideally in the form of randomized controlled trials comparing EL to polymeric clips, as both techniques are safe and effective, with favorable outcomes[50,52].
ARTlCLE HlGHLlGHTS
Research background
Laparoscopic appendectomy (LA) has shown advantages in terms of clinical results and cost-effectiveness,even if there is still controversy about which surgical device should be preferred to perform it.
Research motivation
To evaluate the safety cost-effectiveness of surgical devices in LA stump closure.
Research objectives
Incidence of wound infections, abdominal abscesses and total post-operative complications according to the Dindo-Clavien classification in LA stump closure with endoloop (EL) or endostapler.
Research methods
A meta-analysis was performed in terms of surgical complications, comparing the clinical data of the EL group (821 patients) to the international literature retrieved by Pubmed, according to the PRISMA principles.
Research results
There is no superiority of one or another technique in terms of surgical complications for LA stump closure.
Research conclusions
Routine use of EL is safe in most patients affected by acute appendectomy, even when complicated.
Research perspectives
Studies of EL performing accurate cost analysis are required, in addition to randomized controlled trials comparing this method to polymeric clips, as both techniques have been proved to have to be safe and effective with favorable outcomes.
FOOTNOTES
Author contributions:Zorzetti L and Bellini MI wrote and revised the article; Lauro A, Dalla Via B, Cervellera M, Tonini V, Sorrenti S, Cirocchi R and D’Andrea V designed the research study; Vaccari S, Zorzetti N, Lauro A, and Bellini MI performed the research; and all authors have read and approve the final manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
PRlSMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Noemi Zorzetti 0000-0002-7466-2336; Augusto Lauro 0000-0002-2292-5595; Maria Irene Bellini 0000-0003-0730-4923; Samuele Vaccari 0000-0001-9741-4303; Barbara Dalla Via 0000-0002-7754-8387; Maurizio Cervellera 0000-0002-8885-7660; Roberto Cirocchi 0000-0002-2457-0636; Salvatore Sorrenti 0000-0003-0427-6648; Vito D’Andrea 0000-0001-5709-2530; Valeria Tonini 0000-0003-3130-2928.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Prediction factors for ischemia of closed-loop small intestinal obstruction
- Successful treatment of acute symptomatic extensive portal venous system thrombosis by 7-day systemic thrombolysis
- Retrorectal mucinous adenocarcinoma arising from a tailgut cyst: A case report and review of literature
- Minimally invasive endoscopic repair of rectovaginal fistula
- Effect of cardiac output - guided hemodynamic management on acute lung injury in pediatric living donor liver transplantation
- Blood index panel for gastric cancer detection