Effect of cardiac output - guided hemodynamic management on acute lung injury in pediatric living donor liver transplantation
2022-10-11XiaoJingDouQingPingWangWeiHuaLiuYiQiWengYingSunWenLiYu
Xiao-Jing Dou, Qing-Ping Wang, Wei-Hua Liu, Yi-Qi Weng, Ying Sun, Wen-Li Yu
Xiao-Jing Dou, Qing-Ping Wang, Wei-Hua Liu, Yi-Qi Weng, Ying Sun, Wen-Li Yu, Department of Anesthesiology, Tianjin First Central Ηospital, Tianjin 300192, China
Abstract BACKGROUND Acute lung injury (ALI) after liver transplantation (LT) may lead to acute respiratory distress syndrome, which is associated with adverse postoperative outcomes, such as prolonged hospital stay, high morbidity, and mortality. Therefore, it is vital to maintain hemodynamic stability and optimize fluid management. However, few studies have reported cardiac output-guided (CO-G) management in pediatric LT.AIM To investigate the effect of CO-G hemodynamic management on early postoperative ALI and hemodynamic stability during pediatric living donor LT.METHODS A total of 130 pediatric patients scheduled for elective living donor LT were enrolled as study participants and were assigned to the control group (65 cases) and CO-G group (65 cases). In the CO-G group, CO was considered the target for hemodynamic management. In the control group, hemodynamic management was based on usual perioperative care guided by central venous pressure, continuous invasive arterial pressure, urinary volume, etc. The primary outcome was early postoperative ALI. Secondary outcomes included other early postoperative pulmonary complications, readmission to the intense care unit (ICU) for pulmonary complications, ICU stay, hospital stay, and in-hospital mortality.RESULTS The incidence of early postoperative ALI was 27.7% in the CO-G group, which was significantly lower than that in the control group (44.6%) (P < 0.05). During the surgery, the incidence of postreperfusion syndrome was lower in the CO-G group (P < 0.05). The level of intraoperative positive fluid transfusions was lower and the rate of dobutamine use before portal vein opening was higher, while the usage and dosage of epinephrine during portal vein opening and vasoactive inotropic score after portal vein opening were lower in the CO-G group (P < 0.05). Compared to the control group, serum inflammatory factors (interleukin-6 and tumor necrosis factor-α), cardiac troponin I, and N-terminal pro-brain natriuretic peptide were lower in the CO-G group after the operation (P < 0.05).CONCLUSION CO-G hemodynamic management in pediatric living-donor LT decreases the incidence of early postoperative ALI due to hemodynamic stability through optimized fluid management and appropriate administration of vasopressors and inotropes.
Key Words: Cardiac output; Ηemodynamic management; Child; Liver transplantation; Acute lung injury; Reperfusion injury
lNTRODUCTlON
Pediatric liver transplantation (LT) is a life-saving procedure for children with end-stage liver disease caused by biliary atresia or progressive familial intrahepatic cholestasis[1]. The number of LTs performed globally has been reported to be 4-9 per million people < 18 years, with a 10-year survival rate of > 80%[1-3]. The incidence of post-LT acute lung injury (ALI) has been reported to vary between 34.2% and 77.8%[4,5]. ALI may lead to acute respiratory distress syndrome (ARDS), which is associated with adverse postoperative outcomes, such as prolonged hospital stay, high morbidity, and mortality[6]. ARDS is often caused by hemodynamic instability during surgery, which results in liver hypoperfusion and ischemia-reperfusion injury, exaggerating the inflammatory process[7]. Additionally, hemodynamic instability accompanied by excessive administration of fluids and blood products leads to fluid imbalance during LT. Clinical studies have demonstrated that intraoperative fluid overload is the primary risk factor for postoperative pulmonary complications (PPCs)[8]. Effective fluid management strategies can reduce the occurrence of PPCs[9].
In the early stages after LT, ALI may prolong the intubation time and increase the risk of systemic infectious complications. Prolonged mechanical ventilation due to refractory respiratory failure is an extremely morbid event and a marker of poor recipient recovery that predisposes a recipient to longterm ventilator dependency and predicts further complications. Several factors are involved in the onset of postoperative ALI, among which intraoperative hemodynamic instability and fluid overload are the most important[10].
Pediatric patients with poor oxygen reserve capacity are vulnerable to ischemia and hypoxia, leading to ALI. Therefore, it is vital to maintain hemodynamic stability and optimize fluid management. A study on pediatric kidney transplantation showed that the use of the cardiac output-guided (CO-G) algorithm led to excellent renal results, with a trend toward less fluids in favor of norepinephrine[11]. However, few studies have reported CO-G management in pediatric LT. CO monitoring is extremely difficult and limited due to the anatomical characteristics and biomaterial technology in pediatric liver transplant patients. The pressure recording analytical method (PRAM) is a minimally invasive hemodynamic monitoring method that calculates hemodynamic parameters, with the advantages of being invasive, not requiring calibration, and suitable for pediatric patients weighing < 20 kg compared to other devices[12]. In this study, a randomized controlled trial was designed to evaluate the effect of CO-G algorithm management on reducing ALI events after pediatric LT and intraoperative hemodynamic stability with PRAM.
MATERlALS AND METHODS
Participants
This was a randomized controlled trial conducted at Tianjin First Central Hospital. This study was approved by the Ethics Committee of Tianjin First Center Hospital in China (Approval Number: 2019N180KY), and written informed consent was obtained from eligible guardians. The clinical trial registration number is ChiCTR1900026016. The inclusion criteria were as follows: (1) Pediatric liver recipients 5-24 mo of age; (2) American Society of Anesthesiologists physical status III or IV; and (3) Living donation. The exclusion criteria were as follows: (1) Contraindications to arterial puncture and cannulation; (2) Preoperative incomplete data; (3) Preoperative severe cardiac, renal, and other viral organ failure before LT; and (4) Sepsis and/or pulmonary complications, including pneumonia, atelectasis, pulmonary edema, pleural effusion, and ARDS within 2 wk before surgery. Every case of transplantation passed the ethical review and approval of the Tianjin First Center Hospital.
Anesthesia and surgery
Patients enrolled in this study were routinely monitored for heart rate (HR), non-invasive blood pressure, pulse oximetry, and electrocardiography. Anesthesia was induced using scopolamine (0.01 mg/kg), midazolam (0.15 mg/kg), etomidate (0.15 mg/kg), fentanyl (2-5 μg/kg), and vecuronium (0.2 mg/kg) to maintain analgesia, muscle relaxation, and sedation. After intubation, mechanical ventilation was performed with a fraction of inspired oxygen (FiO2) of 50%-60%, tidal volume of 8-10 mL/kg, respiratory rate of 20-28/min, an inspiration-to-expiration ratio of (1.0:1.5)-2.0 min, an inspiration-toexpiration ratio of (1.0:1.5)-2.0, and a postapneic end-tidal carbon dioxide pressure of 30-35 mmHg (1 mmHg = 0.133 kPa). Anesthesia maintenance included intravenous infusion of propofol (9-15 mg/kg/h), intermittent intravenous fentanyl (1-3 μg/kg), and intravenous infusion of atracurium besylate (1-2 μg/kg/h).
The operative procedure was performed using both the caval replacement and piggyback techniques. Reperfusion of the liver graft started with opening of the portal vein, followed by opening of the artery. After arterial reperfusion, the bile duct was connected to the recipient’s bile duct (choledochocholedochostomy) or to a small bowel loop (hepaticojejunostomy). A back table biopsy of the donor liver was performed before implantation.
Hemodynamic instrumentation and design
The central venous pressure (CVP) was monitored continuously with a three-lumen central venous catheter placed using ultrasound-guided right internal jugular vein puncture and arterial pressure was monitored invasively in both groups using a catheter placed in the radial artery. The mean arterial blood pressure (MAP), HR, cardiac index (CI), stroke volume index (SVI), stroke volume variation (SVV), and left ventricular contractility index, which is the maximum increase in the speed of intraventricular pressure (dp/dtmax), were continuously monitored through PRAM (Most Care monitoring system; Vytech Healthcare, Padova, Italy)viaa pressure catheter (Pulsion Medical Systems, Munich, Germany) in the CO-G group.
Hemodynamic management included fluid transfusion and use of vasopressors and/or inotropes: (1) Fluid management protocol: In the control group, fluid management was implemented mainly according to CVP, urine volume, bleeding,etc.CVP was maintained at a level of 6-12 mmHg, and the urine volume at ≥ 20 mL/h. If the urine volume was < 20 mL/h and/or CVP < 6 mmHg, 4% albumin or crystalloid was infused to expand the volume; if the urine volume was < 20 mL/h and/or CVP > 12 mmHg, 0.5 g/kg furosemide was also administered to decrease fluid load. In the CO-G group, fluid was infused at a rate of 10 mL/kg/h to maintain SVV at 12%-15%. If SVV was > 12%, 4% albumin or crystalloid was administered in combination with CI, SVI, and other parameters; and (2) Vasopressor and/or inotrope protocol: In the control group, if MAP was < 50 mmHg, norepinephrine or dopamine was pumped intravenously, and if MAP fell rapidly below 30 mmHg after the opening of the portal vein, rehydration and/or epinephrine of 1-5 mg/kg was administrated. In the CO-G group, the administration of vasopressors and/or inotropes according to the CO and other hemodynamic parameters is illustrated in the PRAM diagram (Figure 1). Other management: Albumin and blood products were infused to maintain the blood volume and hemoglobin level at ≥ 8 g/L. The electrolyte and acid-base balance were maintained within the normal range during surgery and were kept warm.
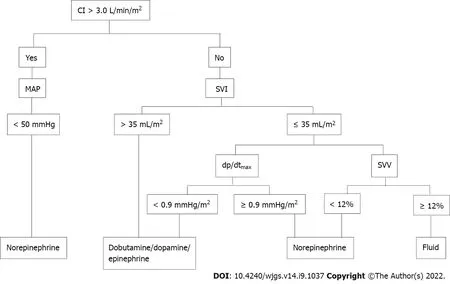
Figure 1 Pressure recording analytical method. CI: Cardiac index; MAP: Mean arterial blood pressure; SVI: Stroke volume index; SVV: Stroke volume variation.
Blood assays
Venous blood (3 mL) was collected from the right internal jugular catheter and placed into vacuum tubes containing sodium heparin. Blood samples were collected at four time points: Immediately before the induction of general anesthesia (baseline, T0), at the end of surgery (T1), 1 d after surgery (T2), and 3 d after surgery (T3). The samples were then placed in dry tubes and centrifuged. The serum was removed and stored at -80 °C until analysis. The levels of serum inflammatory factors interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), cardiac troponin I (cTnI), and N-terminal pro-brain natriuretic peptide precursor (NT-pro-BNP) were analyzed at four time points. Wuhan Huamei Biological Technology Company (Wuhan, China) was used to construct the reaction standard curves. The protein levels were calculated by comparing the optical density values of the samples with the standard curve.
Data collection
The following patients and preoperative variables were assessed: Patient characteristics, including age, weight, pediatric end-stage liver disease, and graft characteristics, including graft mass, graft-torecipient body weight ratio, cold ischemia time of the graft, and preoperative laboratory test results. The intraoperative hemodynamic parameters included baseline values, the maximum and minimum values of HR, MAP, CVP, and the incidence of postreperfusion syndrome (PRS, defined as a sudden drop in MAP of ≥ 30% within 1-5 min of reperfusion)[13], and hemodynamic management, including transfusion of red blood cells, fresh frozen plasma, and fluids (colloids and crystalloids), usage of vasopressor or inotrope agents, and vasoactive drug score (VIS) [VIS = dopamine dose (μg/kg/min) + dobutamine dose (μg/kg/min) + 100 × epinephrine dose (μg/kg/min) + 10000 × vasopressin dose (μg/kg/min) + 100 × norepinephrine dose (μg/kg/h) + 100 × milrinone dose (μg/kg/min)][14]. The postoperative variables included the occurrence of ALI and pulmonary complications in the first week after surgery, duration of mechanical ventilation, intense care unit (ICU) stay, incidence of readmission to the ICU for pulmonary complications, hospital stay, and in-hospital mortality.
Relevant definitions
ALI was defined according to the following criteria[15]: (1) Acute onset; (2) PaO2/FiO2< 300; (3) Pulmonary artery wedge pressure < 18 mmHg without clinical evidence of left atrial hypertension; and (4) Bilateral infiltrates on chest radiography.
Study outcomes
The primary outcome was early postoperative ALI. The secondary outcomes included early PPCs, ICU stay, readmission to the ICU for pulmonary complications, hospital stay, in-hospital mortality, and intraoperative hemodynamic stability.
Sample size, randomization, and blinding
Sample size:The incidence of ALI in children after LT in the control and intervention groups was 50% and 25%, respectively, based on previous reports[3,4]. The α-error was set to 0.05, β-error to 80%, and the ratio to 1:1. PASS 15 (NCSS, LLC. Kaysville, UT, United States) was used to calculate the sample size, and the results showed that at least 58 patients should be included per group, with an expected dropout rate of 10%.
Randomization and blinding:Pediatric patients were randomly assigned to the CO-G hemodynamic therapy algorithm (CO-G group) and the control group by a computer-generated random number system and individually sealed in envelopes. One investigator created computer-generated randomization codes and enrolled participants in accordance with the approved study protocol (Chi-CTR1900026016), one investigator created computer-generated randomization codes and enrolled the participants. The participants were assigned to different groups based on the codes, which were kept in sequentially numbered opaque envelopes. After anesthetic induction, the envelopes were opened by another investigator, who was an anesthesiologist conducting CO-G hemodynamic management during the LT. An additional third investigator measured the primary and secondary outcomes in a blinded manner. The surgeons were blinded to the group allocation.
Statistical analysis
Outcome analyses were performed using SPSS software package (SPSS; IBM. Corp., Armonk, NY, United States). The Kolmogorov-Smirnov test was used to analyze the distribution of the data. The results are presented as the mean (SD), median (second quartile, third quartile), or number of patients. The patient characteristics and perioperative variables were compared using an independentt-test or Fisher’s exact test, as appropriate. Changes in the above variables in the group over time were analyzed using repeated ANOVA, followed by an appropriatepost hoctest. Categorical data were compared using the chi-squared test or Fisher’s exact method. The results were evaluated within a 95% reliability index (P< 0.05).
RESULTS
Baseline patient characteristics and intraoperative data
A total of 148 patients were screened from December 2019 to October 2020, and 130 patients were enrolled and analyzed in this study. Among whom, 65 patients were randomly allocated to the CO-G group and 65 to the control group (Figure 2, Table 1). The patient characteristics were similar between the study groups (Table 1).
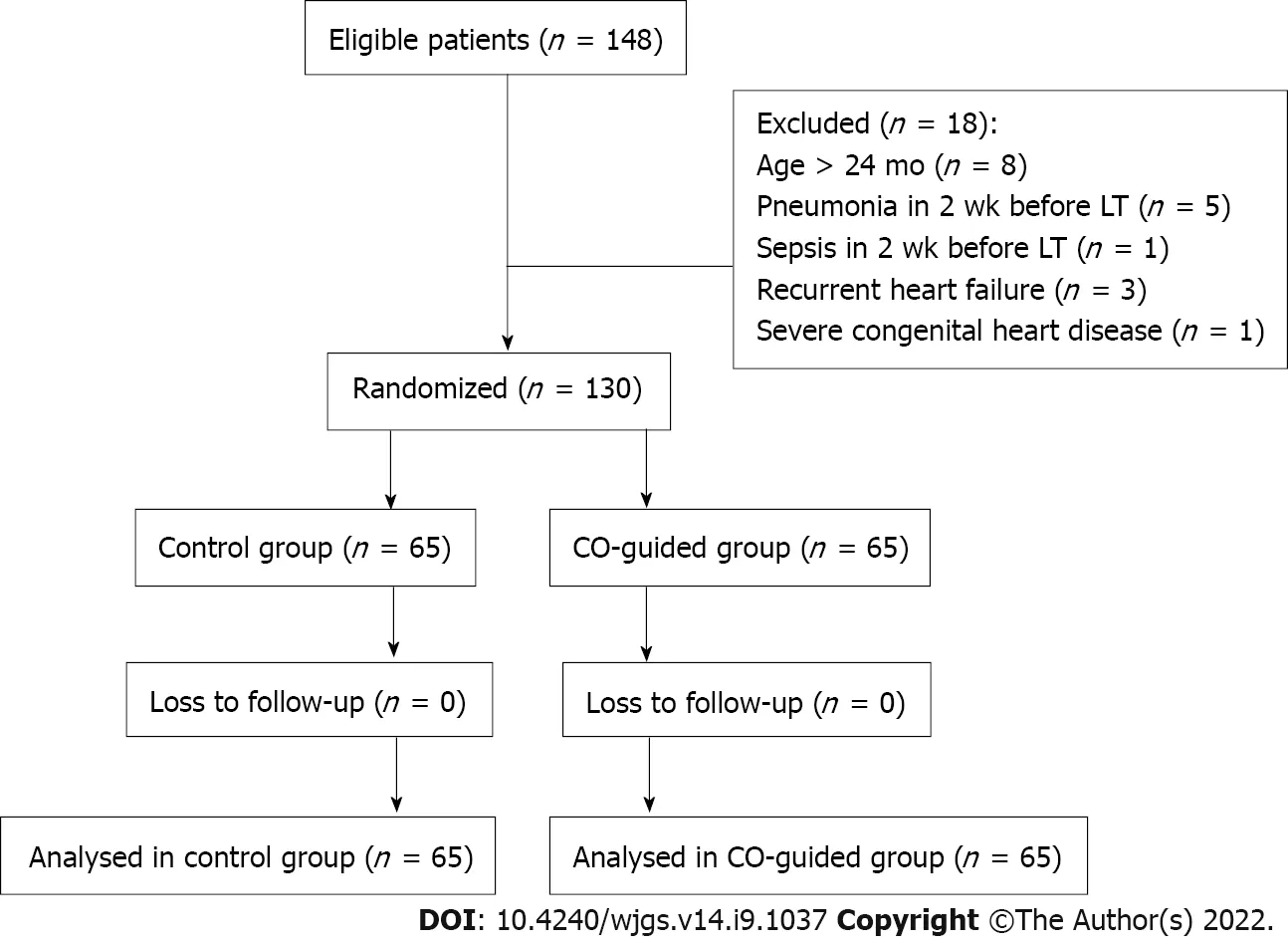
Figure 2 Trial profile. CO: Cardiac output; LT: Liver transplantation.
Primary outcome
The incidence of early postoperative ALI was 27.7% in the CO-G group, which was lower than that in the control group (44.6%) (P< 0.05) (Table 2). There were no significant differences in other pulmonary complications and ICU stay, readmission to the ICU for pulmonary complications, hospital stay, and inhospital mortality (Table 2).
Intraoperative hemodynamic changes
Compared to the control group, intraoperative fluid transfusion (865.5 ± 153.1 mLvs1222.7 ± 381.9 mL,P< 0.001), and positive fluid balance (598.8 ± 320.7 mLvs1021.4 ± 467.9 mL,P< 0.001) were lower in the CO-G group. The utilization of dobutamine before portal vein opening was higher, whereas the usage and dosage of epinephrine during portal vein opening and VIS after portal vein opening [2 (2-3)vs3 (2-7),P< 0.05] were lower in the CO-G group. The peak value of CVP was lower (9.46 ± 1.66 mmHgvs11.64 ± 2.1 mmHg,P< 0.001) while the bottom value of MAP was higher (43.3 ± 7.4 mmHgvs34.9 ± 5.5 mmHg,P< 0.001) in CO-G group. The incidence of PRS in the CO-G group was lower than that in the control group (33.8%vs53.8%,P= 0.022) (Table 3).
Differences in inflammatory factors
In both groups, the levels of inflammatory factors (IL-6 and TNF-α) and cTnI increased during the operation, decreased gradually during the following 3 d postoperatively, and returned to preoperative levels (Table 4). The NT-proBNP levels showed the same trend (Table 4). For group comparisons, at T1 and T2, the values of IL-6, TNF-α, and cTnI were significantly lower in the CO-G group (Table 4). At T1, T2, and T3, the NT-proBNP levels were significantly lower in the CO-G group (Table 4).
DlSCUSSlON
To the best of our knowledge, this is the first randomized controlled trial to evaluate the effect of COguided hemodynamic therapy in pediatric liver recipients. In this study, hemodynamic parameters, including CO, SVV, SVI, and dp/dtmax, obtained through PRAM monitoring were used to guide intraoperative hemodynamic management. The incidence of postoperative ALI was significantly lower in the interventional group than in the control group. Moreover, the inflammatory factors of IL-6, TNF-α, and cTnI decreased faster in the intervention group than in the control group.

Table 1 Patient demographic and perioperative data
Effects on ALI
The incidence of ALI in the control group was 44.6%, which was close to that used in the sample size calculation (50%). These results are similar to those of previous studies. Honget al[4] reported that the rate of ALI was 34.6% in adult LT, while Yaoet al[5] showed that the incidence of ALI in a rat LT model was 77.8%. CO-G interventions significantly decreased ALI occurrence after pediatric LT. This might be due to more stable hemodynamic parameters, which can mitigate ischemia-reperfusion injury, as well as optimized vasopressor use and fluid management in the CO-G group.
Effects on inflammatory factors
Inflammatory lung liver interactions, and the activation of nuclear factor-kappa B in particular, may be implicated in the pathogenesis of permeability-type pulmonary edema[16]. It is well accepted known that the inflammatory response is involved in the progression of ALI and that cytokines, such as TNF-α, IL-1β, and IL-6, play important roles in the massive inflammatory response that is a hallmark feature of ALI[17]. In contrast, IL-4 and IL-10 seem to exert protective roles[18].
Therefore, in the present study, we selected TNF-α and IL-6, which are typical factors that reflect inflammation and oxidative stress in the lungs. The results showed that the inflammatory factors mentioned above were elevated from the end of the operation and returned to preoperative levels 3 d after surgery. Compared with the control group, TNF-α and IL-6 levels were significantly lower from the end of the operation to 1 d after surgery in the CO-G group, indicating that CO-G hemodynamic therapy can attenuate lung inflammation during LT.
Effects on hemodynamic stability
Several triggering conditions, including bleeding, blood transfusion, and ischemia-reperfusion, can exaggerate the inflammatory process of ALI. Among them, liver ischemia-reperfusion may be the most notable factor. The greatest hemodynamic disturbance in LT is defined as PRS, which occurs during reperfusion of the donated liver after unclamping of the portal vein. PRS is characterized by marked decreases of > 30% in MAP lasting > 1 min within 5 min after reperfusion and occurring with an incidence of 12.1%-42%[19]. A dramatic drop in blood pressure and myocardial inhibition are manifestations, but are also risk factors for PRS[20]. It is noteworthy that the intraoperative stabilization of arterial pressure through the preventive use of vasopressors during the reperfusion phase is capable of decreasing the incidence of PRS[21]. In our study, the incidence of PRS in the CO-G group was lower than that in the control group, which was attributed to the appropriate cardiotonic and optimized vasopressor by the continuous monitoring of CO.

Table 2 Results for primary outcome and secondary outcomes
In our study, the use of dobutamine before portal vein opening was higher than that in the control group, whereas the usage and dosage of epinephrine during portal vein opening and VIS after portal vein opening were lower in the CO-G group. CO-G hemodynamic therapy can reduce hemodynamic fluctuations and prevent the occurrence of PRS by continuously monitoring the intraoperative CO, which can consistently summarize cardiac function, and aid to the appropriate administration of vasopressors and inotropes.
Effects on myocardial injury
Myocardial injury commonly occurs in LT[22], which leads to arrhythmias and myocardial depression, severely affecting circulatory stability and aggravating ischemia-reperfusion injury. cTnI is currently recognized as a sensitive and specific gold standard for reflecting the degree of myocardial injury, and mildly elevated cTnI levels (≥ 0.04 ng/mL) are strongly associated with postoperative mortality[23]. Shenget al[24] demonstrated that intraoperative cTnI elevation (≥ 0.07 ng/mL) was a significant prognostic risk factor in ALI after pediatric living-donor LT for children with biliary atresia. NT-proBNP is an early and reliable predictor of myocardial dysfunction onset[25]. BNP levels positively correlated with left ventricular systolic function and required inotropic support[26].

Table 3 Hemodynamic parameters and hemodynamic management
In our study, we analyzed cTnI and NT-pro-BNP levels to identify myocardial injury and cardiac dysfunction. The results showed that cTnI and NT-pro-BNP levels were elevated from the end of the operation and returned to preoperative levels 3 d after surgery. NT-pro-BNP level was lower at 3 d after surgery than at the preoperative level. Compared to the control group, the values of cTnI were significantly lower at the end of surgery and 1 d after surgery in the CO-G group. In the CO-G group, the NT-pro-BNP values from the end of surgery to 3 d after surgery were all lower than those in the control group, indicating that CO-G hemodynamic therapy can attenuate myocardial injury and cardiac volume load, which could be helpful in circulatory stability and attenuation of pulmonary edema.
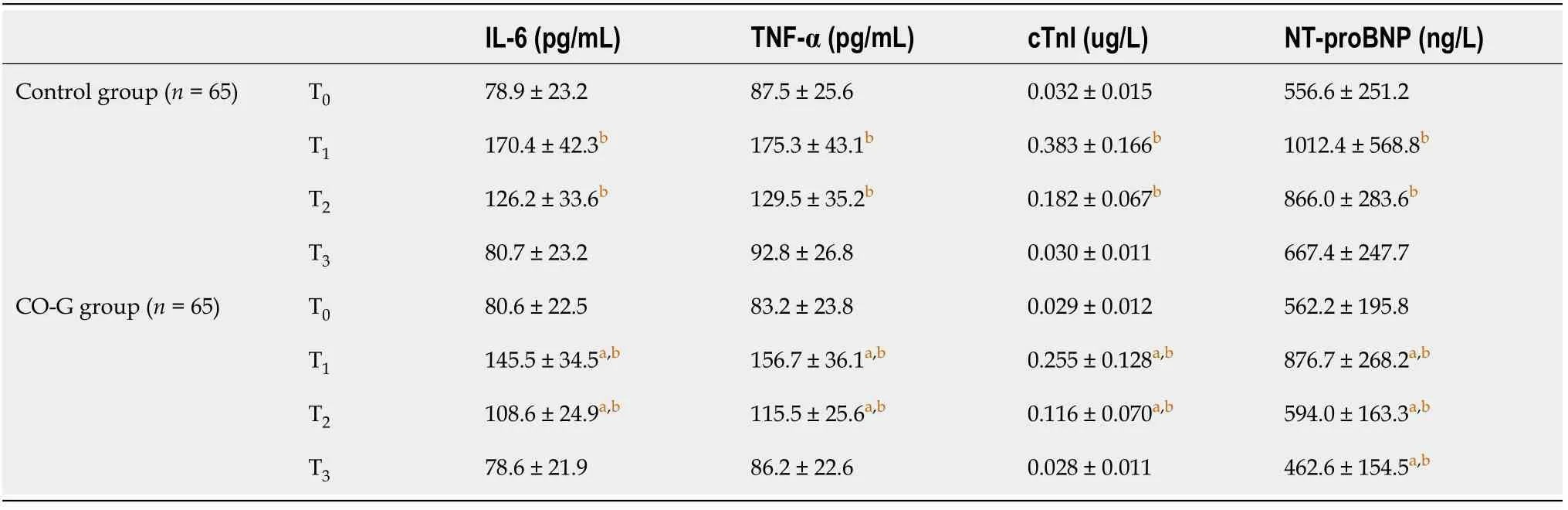
Table 4 Changes in serum interleukin-6, tumor necrosis factor-α, troponin l, and N-terminal pro-brain natriuretic peptide levels at every time point
Optimizing fluid management
Intraoperative fluid overload can exacerbate pulmonary edema and heart failure, thereby increasing the duration of postoperative mechanical ventilation, pulmonary infection, and mortality. Previous intraoperative volume management is often achieved through empirical rehydration and CVP-directed management; CVP is a pressure-based index that cannot accurately reflect volume status, and CVPdirected fluid management can result in volume overload[27,28]. Compared to pressure-monitoring metrics, volume-monitoring metrics better reflect volume status to guide hemodynamic management, and SVV < 12% and PPV < 13% are more accurate in predicting fluid responsiveness[29]. Shinet al[30] showed that the sensitivity of SVV for monitoring blood volume changes during the neohepatic period of LT was 89%, with a specificity of 80%, which was significantly better than that of CVP. In addition, studies have shown that CO-G fluid management reduces postoperative complications by 20% to 30% compared with any infusion strategy[31]. In this study, CO-directed fluid management combined with SVI and SVV showed that intraoperative fluid transfusion and maximum CVP were significantly lower in the CO-G group than in the control group. The incidence of postoperative ALI was also significantly lower, suggesting that CO-G hemodynamic management can reduce fluid overload, decrease the occurrence of pulmonary edema, stabilize cardiopulmonary function, control CVP, and reduce the occurrence of ALI.
Limitations
As this was a single center study, a multicenter study with other monitoring indicators is needed for further analysis.
CONCLUSlON
CO-G hemodynamic management in pediatric living donor LT can decrease the incidence of early postoperative ALI due to hemodynamic stability through optimized fluid management and appropriate administration of vasopressors and inotropes achieved by continuous monitoring of CO.
ARTlCLE HlGHLlGHTS
Research background
Acute lung injury (ALI) post-liver transplantation (LT) may lead to acute respiratory distress syndrome,which is associated with adverse postoperative outcomes, such as prolonged hospital stay, high morbidity, and mortality. Therefore, it is vital to maintain hemodynamic stability and optimize fluid management. However, few studies have reported cardiac output-guided (CO-G) management in pediatric LT.
Research motivation
In this study, a randomized controlled trial was designed to evaluate the effect of CO-G algorithm management on reducing ALI events after pediatric LT and intraoperative hemodynamic stability with pressure recording analytical method (PRAM).
Research objectives
To investigate the effect of CO-G hemodynamic management in pediatric living donor LT on early postoperative ALI and its influence on hemodynamic stability during surgery.
Research methods
A total of 130 pediatricians scheduled for elective living donor LT were enrolled as study participants and were assigned to the control group (65 cases) and CO-G group (65 cases). In the CO-G group, CO was considered the target for hemodynamic management. In the control group, hemodynamic management was based on usual perioperative care guided by central venous pressure, continuous invasive arterial pressure, urinary volume,etc.The primary outcome was early postoperative ALI. Secondary outcomes included other early postoperative pulmonary complications, readmission to the intense care unit (ICU) for pulmonary complications, ICU stay, hospital stay, and in-hospital mortality.
Research results
The incidence of early postoperative ALI was 27.7% in the CO-G group, which was significantly lower than that in the control group (44.6%) (P< 0.05). During the surgery, the incidence of postreperfusion syndrome was lower in the CO-G group (P< 0.05). The level of intraoperative positive fluid transfusions was lower and the rate of dobutamine use before portal vein opening was higher, while the usage and dosage of epinephrine when portal vein opening and vasoactive inotropic score after portal vein opening were lower in the CO-G group (P< 0.05). Compared to the control group, the serum inflammatory factors interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), cardiac troponin I (cTnI), and N-terminal-pro hormone BNP in the CO-G group were lower after the operation (P< 0.05).
Research conclusions
CO-G hemodynamic management in pediatric living-donor LT decreased the incidence of early postoperative ALI, which is considered to benefit from hemodynamic stability through optimized fluid management and appropriate administration of vasopressors and inotropes by continuous monitoring of CO.
Research perspectives
This is the first randomized controlled trial to evaluate the effect of CO-G hemodynamic therapy in pediatric liver recipients. In this study, hemodynamic parameters, including CO, stroke volume index, stroke volume variation, and the maximum increase in the speed of intraventricular pressure (dp/dtmax), obtained through the PRAM monitoring were used to guide intraoperative hemodynamic management. The incidence of postoperative ALI was significantly lower in the interventional group. Moreover, the inflammatory factors of IL-6, TNF-α, cTnI, decreased faster in the intervention group.
FOOTNOTES
Author contributions:Dou XJ contributed to acquisition of data, data analysis, and wrote the manuscript; Yu WL provided substantial contribution to the conception and design of the study and corrected the manuscript; Wang QP, Liu WH, Weng YQ, and Sun Y collected the data.
lnstitutional review board statement:This study was approved by the Ethics Committee of Tianjin First Center Hospital in China (Approval Number: 2019N180KY).
Clinical trial registration statement:The clinical trial registration number is ChiCTR1900026016.
lnformed consent statement:Informed consent was obtained from eligible guardians.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:Data would be shared under proper request for the corresponding author.
CONSORT 2010 statement:The authors have read the CONSORT 2010 Statement, and the manuscript was prepared and revised according to the CONSORT 2010 Statement.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Wen-Li Yu 0000-0003-1700-4844.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Prediction factors for ischemia of closed-loop small intestinal obstruction
- Successful treatment of acute symptomatic extensive portal venous system thrombosis by 7-day systemic thrombolysis
- Retrorectal mucinous adenocarcinoma arising from a tailgut cyst: A case report and review of literature
- Minimally invasive endoscopic repair of rectovaginal fistula
- Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis
- Blood index panel for gastric cancer detection