Inner limiting membrane peeling prevents secondary epiretinal membrane after vitrectomy for proliferative diabetic retinopathy
2022-09-14RongHanWuMingNaXuKeLinMingXueRenHanWenKeMiFengHongJiaZhouNivedMoonasarZhongLin
INTRODUCTION
Secondary epiretinal membrane (ERM) is not a rare complication after vitrectomy. About 8.97% to 47.7%patients occurred secondary ERM after vitrectomy without internal limiting membrane (ILM) peeling for rhegmatogenous retinal detachment (RRD)
. The location of retinal breaks at the equator is a significant risk factor [odds ratio (OR),3.9; 95% confidence interval (CI), 1.3-11.2]
. It might cause visual impairment or metamorphopsia
, thus requiring further membrane peeling surgery. A series of clinical studies found ILM peeling prevent the development of secondary ERM for RRD, although better best-corrected visual acuity (BCVA)among ILM peeling patients was not found
. There were also some studies found ILM peeling can be as a prophylactic treatment to prevent macular pucker formation in patients who underwent retinectomy
.
2.2.2.1 危害症状。叶片先出现水渍状青灰色斑点,沿叶脉向两端扩展,形成边缘暗褐色、中央淡褐色或青灰色的大斑。后期病斑常纵裂,严重时融合,叶片变黄枯死(图2)。
However, in practice, there are no uniform criteria for the surgical removal of the secondary ERM after vitrectomy for PDR. We encountered rapid and apparent development of secondary ERM in some cases with a mild postoperative reaction. We investigated the original ILM peeling for the prevention of secondary ERM and postoperative visual acuity(VA) and risk factors for secondary ERM development.
治疗结果:试验组28例,一次治愈2例,6-12月后二次治愈13例,6-12月后行第三次131-I治疗者13例;第一次治愈(以下均含甲低)2例,第二次治愈13例,第三次治愈(含甲低)13例,1年后甲低11例。对照组29例,一次治愈(含甲低)25例,二次治愈(含甲低)4例,1年后甲低26例。血管杂音:试验组与对照组血管杂音消失治愈后基本相同,甲低发生率对照组高于实验组,有统计学意义。结果见表1。
农业经济管理是指在市场环境和社会经济条件的实际情况下,根据国家相关的经济政策方针而对农村经济施行的一种管理活动。具体到不同的地区,农业经济管理就要充分考虑到各地不同的市场环境和经济条件,并要在国家相关经济政策方针的框架内实现对农业经济发展的指导,制定相关的发展目标。而其中核心的部分就是将规划、决定、调控及组织协调的过程实施于生产资料再生产过程中的生产、分配、交换、消费等环节,或与农业、金融、销售、物流等资源进行跨行业整合,打通现代农业发展的产业链条,实现对农村经济发展的法制化、规范化、科学化,以促进农村经济发展水平、社会稳定和人们整体生活水平的提高。
SUBJECTS AND METHODS
ERMs were assessed by two experienced ophthalmologists(Wen H and Lin Z) using the OCT (Heidelberg Spectralis OCT, Heidelberg, Germany) photographs. In the OCT scan,postoperative ERM was defined as hyper-reflective line internal to the ILM. If there were inconsistencies on the ERMs, the photographs were sent to the 3
senior vitreoretinal surgeon with equal or more experience for consultation (Wu RH). To reduce subjective bias, the blind method was applied during assessment.
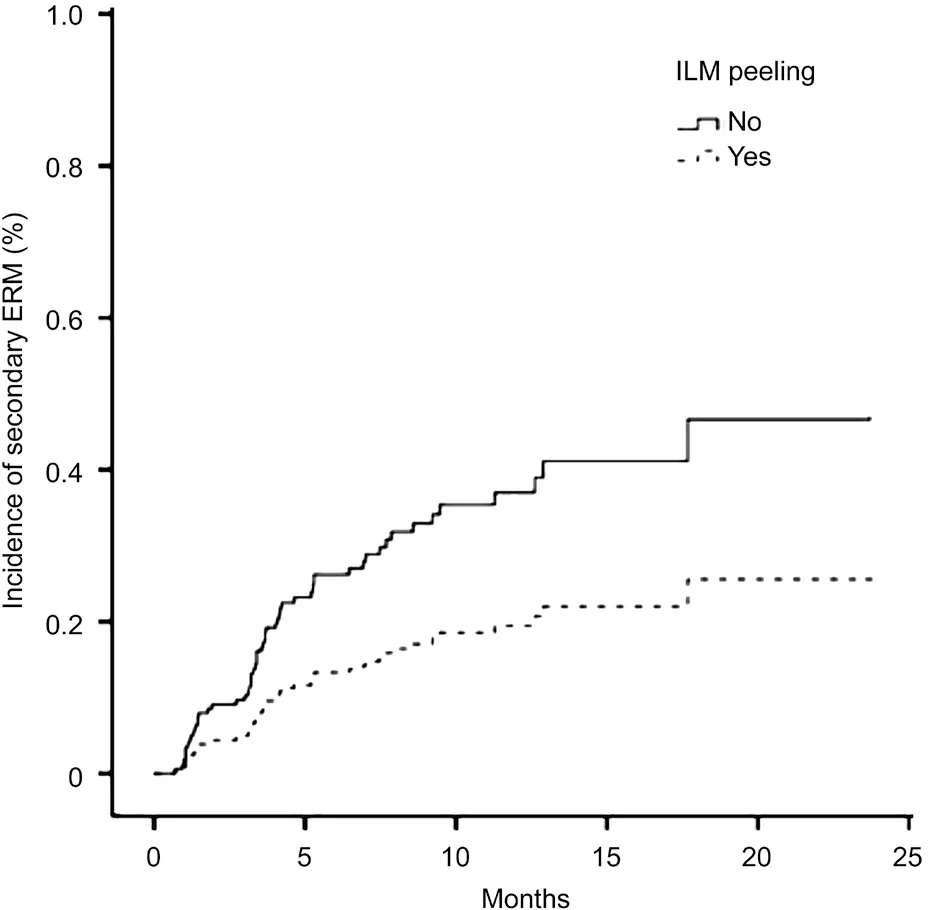
Although the occurrence of secondary ERM after diabetic vitrectomy is common, its mechanism remains unclear. Several factors are likely contributed to the high incidence of ERMs.First, residual native vitreous collagen and ILM in the macular area may act as a scaffold for cellular proliferation. Second,VH, postoperative inflammation, and the damaged retinal surface may provide an ideal environment for the growth of secondary ERMs. ILM peeling may therefore decrease the incidence of secondary ERM because it removes the scaffold that proliferates astrocytes, myofibroblasts, and retinal pigment epithelium cells
. Our results confirm that ILM peeling could effectively reduce the formation of secondary ERM. This result is consistent with previous studies that ILM peeling significantly reduced postoperative ERM after PPV for PDR
. In the current study, we observed that the overall incidence of secondary ERM was 26.9%. Furthermore, from the Cox proportional curve, we observed that the incidence of secondary ERM was lower in ILM peeling group that in ILM non-peeling group at any follow-up point. The incidence of ERM was 37.0% in ILM non-peeling group and 14.0% in ILM peeling group. Several previous studies have reported similar incidences of secondary ERM in ILM non-peeling groups, ranging from 20% to 52.8%, depending on the case mix and the methods of detection
. In fact, more factors associated with ERM formation were presented in ILM peeling group. In ILM peeling group, the patients had a higher rate of preoperative ERM, fibrovascular membrane, retinal attachment, PRP, and air tamponade. PDR eyes with more severe preoperative vitreoretinal changes may be more prone to secondary ERM
. Under diabetic conditions, a local proinflammatory and proangiogenic environment in eyes provides a strong stimulation for tissue proliferation, which is associated with the frequent incidence of ERM
. As well as head-down tilt after gas injection in the postoperative period,a higher number of cells on the macular surface would also result in an increased risk of ERM. In the current study, when considering the comprehensive risk factors, ILM peeling was the only independent risk factor for postoperative secondary ERM, which strongly emphasized the importance of ILM peeling during vitrectomy for patients with PDR.
The 23- or 25-gauge PPVs were performed under retrobulbar(50% mixture of 2% lidocaine and 0.75% bupivacaine) or general anesthesia using three different vitrectomy machines(Accurus Surgical System, Alcon Laboratories, Fort Worth,TX; Stellaris PC, Bausch & Lomb, Bridgewater Township,NJ; Constellation Vision System, Alcon Laboratories) by 5 surgeons. The ERM will be peeled off if there was already ERM at the time of first vitreous surgery. But the removal of ILM was depended on the doctor’s judgment. The ILM was stained with indocyanine green (Dandong Yi Chuang Pharmaceutical Co., Ltd, Liaoning Province, China) and then removed by ILM peeling forceps. ILM was peeled in the entire macular area (at least 2 disc diameters around the fovea). A combined surgery (PPV + phacoemulsification or intraocular lens implantation), pan retinal photocoagulation (PRP), and intraocular tamponade with air were performed, if necessary,depending on the surgeons’ experience.
The research protocol complies with the ethical guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Wenzhou Medical Eye Hospital. The informed consent was waived. Patients’ clinical information was obtained from archived electronic medical records.
The VA in decimal fraction was converted into logarithm of the minimum angle of resolution (logMAR)values. A BCVA of <0.02 was recorded as a logMAR value of 1.7. The normally distributed parameters were presented as mean±standard deviation, whereas median and quartile range was used for non-normally distributed parameters. The Chisquare or Fisher’s exact test, as appropriate, was performed to compare discrete categorized data. Univariate logistic regressions were used to assess the relationship between postoperative ERM development and risk factors, including age, sex, history of retinal laser treatment, and ILM peeling.Next, multivariate logistic regression was performed for postoperative ERM, adjusted age and sex, and factors with a
value of <0.1 in the univariate analysis. The OR, hazard ratio, and 95%CIs were presented. A Cox proportional hazard regression was conducted for postoperative ERMs with adjustment of covariates. Statistical analysis was performed using SAS for Windows (Statistical Analysis System, version 9.1.3, SAS Inc., Cary, NC, USA).
RESULTS
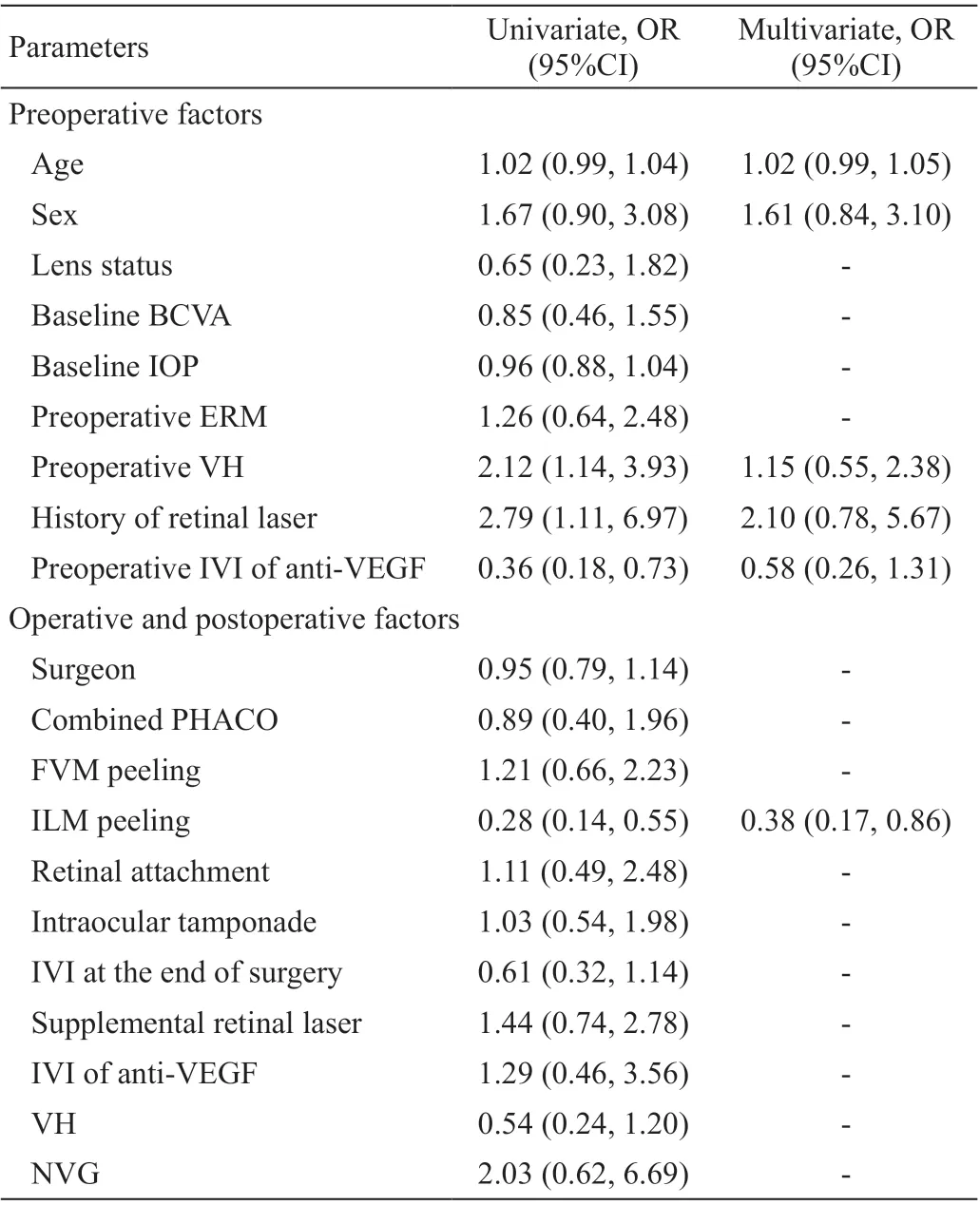
As showed in Figure 2, after adjusting for the factors screened from the univariate model, a Cox proportional hazard regression for the incidence of secondary ERM was performed.which showed only ILM peeling remained significant (hazard ratio, 0.47; 95%CI, 0.23-0.98;
=0.04).
We evaluated perioperative factors to identify their potential effect on the postoperative development of secondary ERM(Table 3). Univariate logistical regression showed that the incidence of secondary ERM significantly increased in cases without ILM peeling, preoperative intravitreal injection of anti-VEGF, preoperative VH, and history of retinal laser treatment.Multivariate analysis revealed that ILM peeling was highly associated with the prevention of secondary ERM development(OR, 0.38; 95%CI, 0.17-0.86,
<0.05).
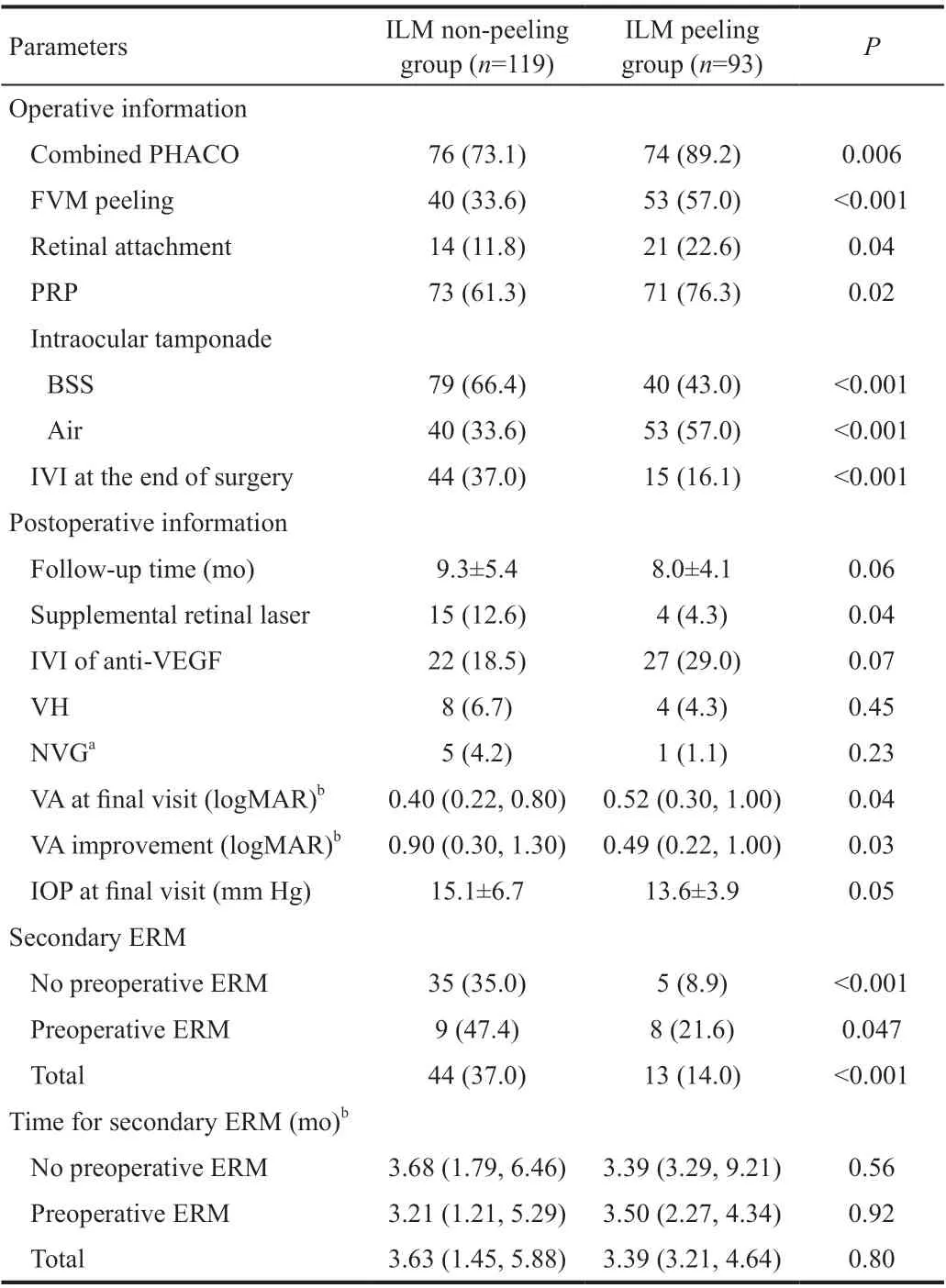
The intra- and postoperative details for both groups are presented in Table 2. More patients in ILM peeling group underwent combined surgery with phacoemulsification (89.2%
73.1% ;
=0.006), fibrovascular membrane peeling (57.0%
33.6%;
<0.001), retinal attachment (22.6%
11.8%;
=0.04), PRP(76.3%
61.3%;
=0.02), and air tamponade (57.0%
33.6%;
<0.001). The follow-up duration was 9.3±5.4mo in ILM non-peeling group and 8.0±4.1mo in ILM peeling group(
=0.06). During the follow-up period, supplemental PRP treatment was more common in ILM non-peeling group thanin ILM peeling group (12.6%
4.3%;
=0.04). At the final follow-up, in ILM non-peeling group, the median logMAR VA was statistically better than in ILM peeling group (0.40
0.52;
=0.04). The median logMAR VA improvement was 0.90 in ILM non-peeling group and 0.49 in ILM peeling group with significant difference (
=0.03). Compared with patients in ILM peeling group, patients in ILM non-peeling group had higher incidence of secondary ERM (37.0%
14.0%;
<0.001; Table 2). There was no difference between ILM nonpeeling group [3.63mo (interquartile range, 1.45-5.88mo)]and ILM peeling group [3.39mo (interquartile range, 3.21-4.64mo)] in the timing of secondary ERM development during the follow-up (
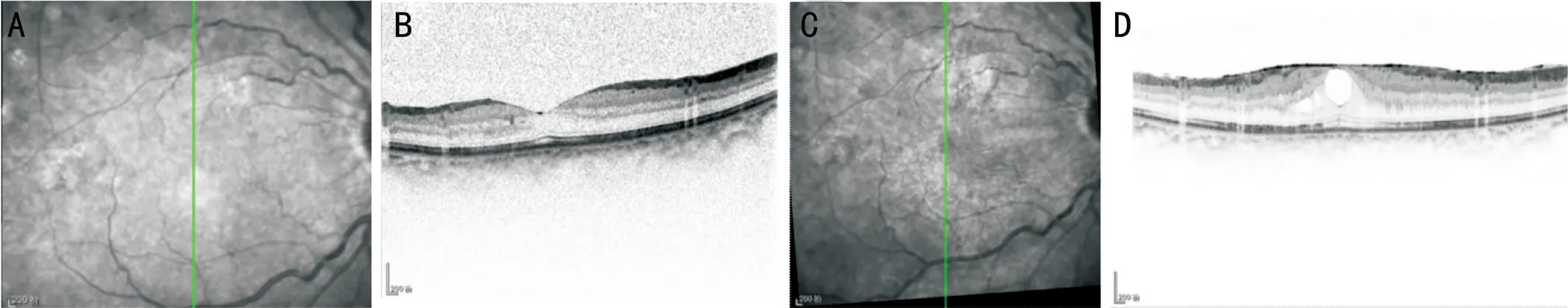
=0.80). Figure 1 shows a typical example of ERM development in ILM non-peeling group.
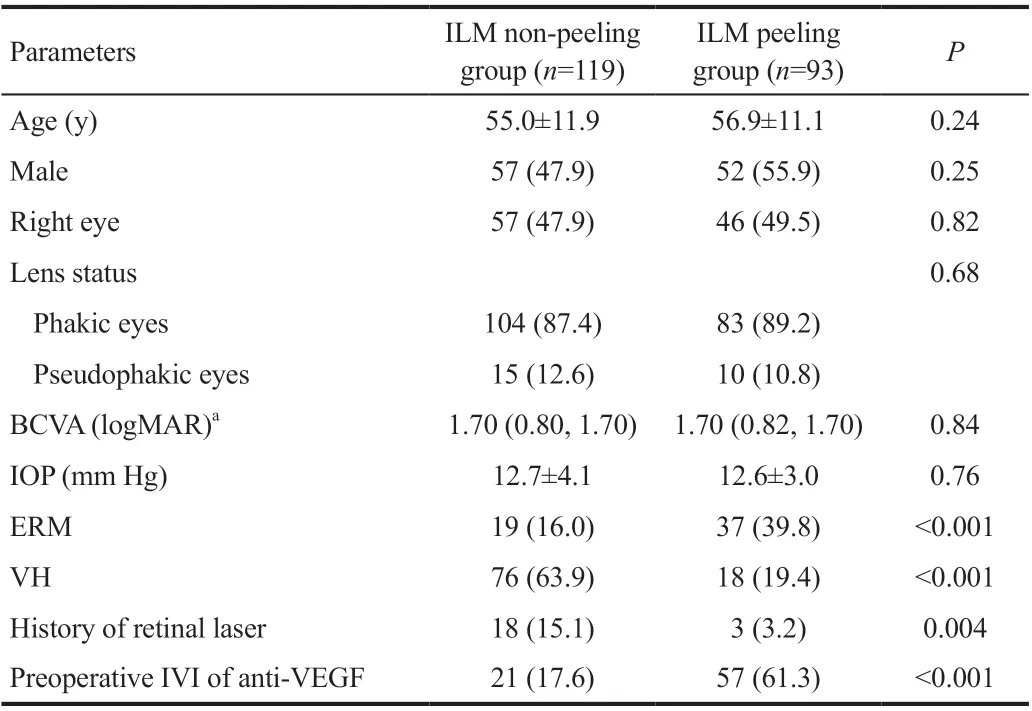
Total 212 eyes of 197 patients (average age, 55.8±11.6y;49.8% men) were enrolled in our study. The overall duration of follow-up was 8.7±4.9mo. There were 93 eyes in ILM peeling group and 119 in ILM non-peeling group. The baseline clinical characteristics of all patients are shown in Table 1.There were no differences in patient age, sex, status of lens,BCVA, and intraocular pressure between the groups. Patients in ILM peeling group had a higher proportion of preoperative ERM (39.8%
16.0%;
<0.001) and preoperative intravitreal anti-VEGF injection (61.3%
17.6%;
<0.001), a lower proportion of VH (19.4%
63.9%;
<0.001) and retinal laser treatment history (3.2%
15.1%;
=0.004) compared with those in ILM non-peeling group.
DISCUSSION
Secondary ERM development causes visual deterioration and macular disorders such as macular cysts or macular thickening after successful surgical treatment of PDRs
. Recently, it has been reported that ILM peeling might decrease the ERM formation and diabetic macular edema
. Although a previous randomized clinical trial that enrolled 207 patients with PDR reported a beneficial role of ILM peeling in patients with PDR for improvement in VA
, ILM peeling was evaluated in patients with PDR undergoing PPV for the primary indication of VH as the primary objective. Most of these patients had VH, making the cohort different from our patient population. This study examined the effectiveness of ILM peeling during vitrectomy for PDR in reducing secondary ERM as well as identifying risk factors.
广垦旅游集团主营酒店、旅游和出租车三大业务板块。作为垦区十大产业集团之一的旅游集团,近年来在省农垦集团“走出去”发展经营理念的指导下,大力整合垦区酒店、旅游、出租车资源,目前已将业务领域由广州辐射到茂名、湛江、汕头、揭阳等广东地市以及北京地区。集团旗下拥有广东农垦燕岭大厦有限公司、广东绿色国际旅行社、北京赛达福出租汽车有限公司、茂名燕岭绿湖湾酒店、湛江燕岭翠园饭店、广垦(茂名)国家热带农业公园、北京国信达福汽车租赁公司等十多家法人单位,经营规模不断壮大。
We retrospectively reviewed patients’ information who underwent pars plana vitrectomy (PPV) for PDR at the Eye Hospital of Wenzhou Medical University between January 2018 and December 2019. PDR was defined by the presence of neovascularization of the disc (NVD) or elsewhere (NVE) or vitreous hemorrhage (VH) or preretinal hemorrhage
. Patients who underwent PPV for PDR and had readable postoperative(≥3mo after operation) OCT photographs were included. The exclusion criteria were as follows: 1) history of PPV surgery;2) history of ocular penetrating trauma; 3) history of retinal vein occlusion, uveitis, age-related macular degeneration,or other fundus disease that may influence the macula; 4)traction retinal detachment involving the posterior pole; 5)silicone oil tamponade; 6) postoperative endophthalmitis. Preand postoperative retinal photocoagulation and intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF)or triamcinolone acetonide were considered risk factors for postoperative ERM development but were not exclusion criteria.
2011年,中央安排41亿元支持中西部地区新建、改扩建特殊教育学校1001所。为重视和支持民族教育事业,中央安排近210亿元改善民族教育办学条件、资助困难学生,稳步推进双语教育,举办西藏、新疆内地中职班,培养技能人才近万人。目前,内地各级各类教育民族班在校生达9.6万人。
Regarding secondary ERM after vitrectomy for proliferative diabetic retinopathy (PDR), two pilot studies have reported the incidence to be 38.5% and 49%
, respectively. ILM peeling can significantly minimize this frequency. Recently,Mehta
reported that ILM cleaning without ILM peeling can reduce the incidence of ERM formation after vitrectomy for PDR compared with that after standard procedure (4%
20%;
=0.01). Lin
had reported that ILM peeling can treat diabetic macular edema, although this has been refuted by some studies
.
For this study, we have also analyzed the time of secondary ERM. The median timing of secondary ERM development was similar at approximately 3mo for both groups. Most of the cases developed secondary ERM between 3 and 6mo postoperatively, similar to that observed in a study with a mean interval of 2.3mo (range, 1-4mo)
.
According to our study, history of retinal laser treatment and preoperative VH was associated with an increased risk of secondary ERM. Chehaibou
found that the eyes with laser treatment developed proliferative tissue along the border of the laser scar, which may induce a gliotic reaction.Furthermore, intravitreal anti-VEGF injection prior to surgery decreased the risk of secondary ERM. Preoperative intravitreal anti-VEGF injection may enhance the absorption of VH by reducing the dissemination of blood cells, thereby decreasing the formation of ERM. However, these three factors were no longer significant in the multivariate analysis, after adjusting for ILM peeling. This may be because of the higher proportion of preoperative VH and laser treatment in ILM non-peeling group and the higher proportion of preoperative intravitreal anti-VEGF injection in ILM peeling group. Additionally, both preoperative retinal laser treatment and PRP were performed away from the retinal vessel arch/posterior polar area (no macular grid pattern laser treatment was performed), rather than adjacent to the macular area.
Considering the visual prognosis after surgery to treat postoperative ERMs, there might be a case for not peeling the ILM
. Meanwhile, several studies have demonstrated that the ILM peeling group had a better BCVA than the ILM nonpeeling group
. In our study, although the improvement in VA was significant in both groups, the final median VA in ILM non-peeling group was better than that in ILM peeling group, and the most significant reason was an apparent higher proportion of VH in the former than that in latter (63.9%
19.4%); therefore, a more apparent VA improvement was gained in ILM non-peeling group.
没有人是永动机,忙碌如他,我一直很好奇他何以如此目标清晰,极度专注地朝前进?他说:“当时最重要的一个机缘是觉得我不年轻了。我24岁,一事无成,大学都没毕业,浪费了很多钱,真的是不能再浪费时间了。其实我从小学习还是可以的,就是大学时有段时间比较迷茫,但没有那段时间也就没有现在的我。”回忆起当初从天体物理转到葡萄酒专业,我在他身上感受到了一直伴随着我的危机感。
Postoperative complications were similar between the two groups. Compared to previous studies, we found that the incidence of postoperative VH and neovascular glaucoma(NVG) was relatively lower at 5.6% and 2.8%, respectively(VH: 8%-25%
; NVG: 1%-9%
). In our study, PRP was extensively applied during PPV, and anti-VEGF was injected preoperatively, which may explain the relatively low rate of VH and NVG
.
Although the current study had a relatively large sample size, there are some limitations. First, because the study was retrospective in nature, there was certain to be some degree of subject heterogeneity. Second, pre- and postoperative intervention and operative procedures varied among different surgeons. Third, the length of follow-up was relatively short.Nonetheless, this is the first study to examine the prevention of secondary ERM for patients with PDR after ILM peeling.It would be beneficial to conduct further randomized clinical trials to support the efficacy of initial ILM peeling for PDR.In conclusion, ILM peeling might prevent secondary ERM development during PPV for PDRs and should be considered by sophisticated vitreoretinal surgeons.
The study was designed by Wu RH,Xu MN and Lin Z; Xu MN, Feng KM and Zhou HJ did data analysis; Wu RH, Xu MN, and Lin Z drafted the manuscript;all authors conducted the acquisition of data; the final manuscript has been read and approved by all authors.
1.基层矛盾预防化解机制的建构必须贯彻法治的原则。党的十八大报告提出“运用法治思维和法治方式化解矛盾、维护稳定”的要求。新时期,让法治思维融入社会的血脉,提高执法者的制度执行力,进而破解社会管理难题,维护社会的稳定,让法律铭刻在公民的心里,应作为基层社会矛盾预防化解机制中长期部署的任务和应当遵循的一个原则。如何让基层社会矛盾解决的过程变成公众真正理解法律、服从法律的行动是要探索的问题。提高公职人员的法律思维,引导群众按法定途径解决纠纷则是法治原则的应有之义。只有回到法治的轨道,才能重树政府和法律的权威。我们期待基层社会矛盾能够在法治的框架内有效得到解决,在全社会重塑法治的信仰。
None;
None;
None;
None;
None;
None;
None;
None;
None.
1 Fallico M, Russo A, Longo A, Pulvirenti A, Avitabile T, Bonfiglio V, Castellino N, Cennamo G, Reibaldi M. Internal limiting membrane peeling versus no peeling during primary vitrectomy for rhegmatogenous retinal detachment: a systematic review and Metaanalysis.
2018;13(7):e0201010.
2 Akiyama K, Fujinami K, Watanabe K, Tsunoda K, Noda T. Internal limiting membrane peeling to prevent post-vitrectomy epiretinal membrane development in retinal detachment.
2016;171:1-10.
3 Sousa K, Calvão-Santos G, Costa J, Ferreira L, Mendonça L, Gentil R,Gomes NL. Anatomical and functional results of ILM peeling
nonpeeling in macula-off rhegmatogenous retinal detachment.
2020;258(10):2105-2110.
4 Martínez-Castillo V, Boixadera A, Distéfano L, Zapata M, García-Arumí J. Epiretinal membrane after pars Plana vitrectomy for primary pseudophakic or aphakic rhegmatogenous retinal detachment: incidence and outcomes.
2012;32(7):1350-1355.
5 Arias L, Padrón-Pérez N, Flores-Moreno I, Giralt L, Cobos E, Lorenzo D, García-Bru P, Dias B, Caminal JM. Internal limiting membrane peeling versus nonpeeling to prevent epiretinal membrane development in primary rhegmatogenous retinal detachment: a swept-source optical coherence tomography study with a new postoperative classification system.
2020;40(7):1286-1298.
6 Akiyama K, Fujinami K, Watanabe K, Fukui M, Tsunoda K, Noda T. Validity and efficacy of internal limiting membrane peeling during initial vitrectomy for rhegmatogenous retinal detachment:visual outcomes in macula-sparing cases.
2021;15(2):114-119.
7 Mahmood SA, Rizvi SF, Khan BAM, Khan TH. Role of concomitant internal limiting membrane (ILM) peeling during rhegmatogenous retinal detachment (RRD) surgery in preventing postoperative epiretinal membrane (ERM) formation.
2021;37(3):651-656.
8 Blanco-Teijeiro MJ, Bande Rodriguez M, Mansilla Cuñarro R,Paniagua Fernández L, Ruiz-Oliva Ruiz F, Piñeiro Ces A. Effects of internal limiting membrane peeling during vitrectomy for maculaoff primary rhegmatogenous retinal detachment.
2018;28(6):706-713.
9 Kohli GM, Shenoy P, Shetty S, Sangole A, Sen A. Macular internal limiting membrane peel for eyes undergoing vitrectomy for retinal detachment: rationalizing selection based on the severity of proliferative vitreoretinopathy.
2021;69(5):1356-1357.
10 Michalewska Z, Bednarski M, Michalewski J, Jerzy N. The role of ILM peeling in vitreous surgery for proliferative diabetic retinopathy complications.
2013;44(3):238-242.
11 Chang PY, Yang CM, Yang CH, Chen MS, Wang JY. Pars plana vitrectomy for diabetic fibrovascular proliferation with and without internal limiting membrane peeling.
2009;23(4):960-965.
12 Mehta A, Rana-Rahman R, Klaassen I, Rees J, Steel DH. The effect of internal limiting membrane cleaning on epiretinal membrane formation after vitrectomy for proliferative diabetic retinopathy.
2020;243(6):426-435.
13 Lin HC, Yang CM, Chen SN, Hsieh YT. Vitrectomy with internal limiting membrane peeling versus nonsurgical treatment for diabetic macular edema with massive hard exudates.
2020;15(7):e0236867.
14 Rinaldi M, Dell’Omo R, Morescalchi F, Semeraro F, Gambicorti E,Cacciatore F, Chiosi F, Costagliola C. ILM peeling in nontractional diabetic macular edema: review and metanalysis.
2018;38(6):2709-2714.
15 Ghassemi F, Bazvand F, Roohipoor R, Yaseri M, Hassanpoor N, Zarei M. Outcomes of vitrectomy, membranectomy and internal limiting membrane peeling in patients with refractory diabetic macular edema and non-tractional epiretinal membrane.
2016;28(4):199-205.
16 Kamura Y, Sato Y, Isomae T, Shimada H. Effects of internal limiting membrane peeling in vitrectomy on diabetic cystoid macular edema patients.
2005;49(4):297-300.
17 Wilkinson CP, Ferris FL III, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales.
2003;110(9):1677-1682.
18 Guo J, Bi X, Chen SN, Chen S, He GH, Wu B, Zhang W, Wang J.Efficacy of internal limiting membrane peeling for diabetic macular edema after preoperative anti-vascular endothelial growth factor injection.
2020;13(11):1758-1764.
19 Rush RB, Del Valle Penella A, Reinauer RM, Rush SW, Bastar PG. Internal limiting membrane peeling during vitrectomy for diabetic vitreous hemorrhage: a randomized clinical trial.
2021;41(5):1118-1126.
20 Rush RB, Rush SW. Pars plana vitrectomy with internal limiting membrane peeling for treatment-Naïve diabetic macular edema: a prospective, uncontrolled pilot study.
2021;15:2619-2624.
21 Someya H, Takayama K, Takeuchi M, Yokoyama H, Kimura T,Morioka M, Takamura Y, Sameshima S, Ueda T, Ogata N, Tashiro M,Kitano S, Sakamoto T. Outcomes of 25-gauge vitrectomy for tractional and nontractional diabetic macular edema with proliferative diabetic retinopathy.
2019;2019:5304524.
22 Im JC, Kim JH, Park DH, Shin JP. Structural changes of the macula on optical coherence tomography after vitrectomy for proliferative diabetic retinopathy.
2017;238(4):186-195.
23 Yang CM, Yeh PT, Cheng SF, Yang CH, Chen MS. Macular appearance after diabetic vitrectomy for fibrovascular proliferation:an optical coherence tomography study.
2010;88(2):193-198.
24 Hsu YR, Yang CM, Yeh PT. Clinical and histological features of epiretinal membrane after diabetic vitrectomy.
2014;252(3):401-410.
25 Chehaibou I, Pettenkofer M, Govetto A, Rabina G, Sadda SR,Hubschman JP. Identification of epiretinal proliferation in various retinal diseases and vitreoretinal interface disorders.
2020;6:31.
26 Gelman R, Stevenson W, Prospero Ponce C, Agarwal D, Christoforidis JB. Retinal damage induced by internal limiting membrane removal.
2015;2015:939748.
27 Ahn J, Woo SJ, Chung H, Park KH. The effect of adjunctive intravitreal bevacizumab for preventing postvitrectomy hemorrhage in proliferative diabetic retinopathy.
2011;118(11):2218-2226.
28 Hernández-Da Mota SE, Nuñez-Solorio SM. Experience with intravitreal bevacizumab as a preoperative adjunct in 23-G vitrectomy for advanced proliferative diabetic retinopathy.
2010;20(6):1047-1052.
29 Takayama K, Someya H, Yokoyama H, Takamura Y, Morioka M,Sameshima S, Ueda T, Kitano S, Tashiro M, Sugimoto M, Kondo M, Sakamoto T, Takeuchi M. Risk factors of neovascular glaucoma after 25-gauge vitrectomy for proliferative diabetic retinopathy with vitreous hemorrhage: a retrospective multicenter study.
2019;9(1):14858.
30 Guan J, Cai N, Liu LM, Zhao N, Liu NN. Ranibizumab pretreatment in vitrectomy with internal limiting membrane peeling on diabetic macular edema in severe proliferative diabetic retinopathy.
2020;11(6):1397-1406.
猜你喜欢
杂志排行
International Journal of Ophthalmology的其它文章
- What can we learn from negative results in clinical trials for proliferative vitreoretinopathy?
- Suggestions on gut-eye cross-talk: about the chalazion
- A novel mutation of RPGR in a Chinese family with X-linked retinitis pigmentosa
- Novel technique of penetrating keratoplasty in high-risk grafts with significant corneal neovascularization
- COVlD-19 infection with keratitis as the first clinical manifestation
- Corneal histomorphology and electron microscopic observation of R124L mutated corneal dystrophy in a relapsed pedigree
