Higher cost of arthroplasty for hip fractures in patients transferred from outside hospitals vs primary emergency department presentation
2022-08-19EmanuelHaugHakanPehlivanRyanMacdonellWendyNovicoffJamesBrowneThomasBrownQuanjunCui
lNTRODUCTlON
The Centers for Medicare and Medicaid Services (CMS) began the Comprehensive Care for Joint Replacement (CJR) model in 2016, which aims to hold hospitals accountable for the quality of care delivered from surgery until 90 d after discharge. As has already been reported, episode-of-care payments for elective Total Joint Arthroplasty (TJA) can vary widely and depend on a number of factors. These factors may include the type of procedure, patient comorbidities, discharge disposition, and readmission rates[1,2]. In July 2016, the CMS proposed implementing bundled payments for hip fracture care in order to control costs and improve quality[3]. This has led to concern that patients with multiple comorbidities or surgically complex patients may either be denied necessary care or transferred to other facilities to prevent financial loss at the initial institution. Transfer to a tertiary care facility is necessary in medically complex or critically ill patients and is protected by the Emergency Medical Treatment and Active Labor Act of 1986 (EMTALA). Furthermore, while EMTALA requires hospitals with special capabilities to accept transfers from less specialized facilities, there are no guidelines defining appropriateness of transfers. The implementation of this bundled care model may result in an increase in unnecessary transfers of high-risk patients to tertiary care centers and safety-net hospitals[4,5]. As a result, it is important to understand not only the greater financial risk associated with accepting these patients, but also, the potential for increased morbidity and mortality of patients who are transferred.
Transfers to tertiary care centers, in general, can reduce mortality associated with critically ill and complex patients[6,7]. However, several studies in the orthopaedic literature demonstrate that transfers can be influenced by factors such as insurance status and time of the week with inappropriate transfers rates ranging between 16%-52%[8-13]. Other studies have shown that the transfer of medically and surgically complex patients can negatively impact the receiving hospitals’ outcome measures and mortality rates[4,14]. These hospital quality metrics are available to the public. If these metrics are negatively influenced by inappropriate transfers, this may deter a patient from undergoing an elective procedure at these institutions. However, this has not been demonstrated in the literature as of yet.
The goal of this study was to examine financial and clinical outcomes in hospitalizations for unplanned arthroplasty in hip fractures between patients transferred from outside hospitals, patients presenting to the emergency department, and patients transferred from skilled nursing facilities. This study will help to further characterize the differences in cost and outcomes between these subsets of unplanned arthroplasty patients, which has not been previously documented to the best of our knowledge. This information is useful to physicians, hospital administrators, and payers as it may identify patient groups that utilize increased resources and suffer increased morbidity and/or mortality.
MATERlALS AND METHODS
Between 2010 and 2015, demographic, financial, and outcomes data were collected on all arthroplasty patients at our institution, a tertiary care center, as part of an Institutional Review Board-approved patient safety initiative. All patients underwent either total hip arthroplasty or proximal femoral hemiarthroplasty by one of three fellowship trained arthroplasty surgeons at this institution. In all cases, the procedural billing code for the arthroplasty procedure was the primary code submitted to the patient’s insurance or medicare. For the purposes of this study, we included all patients with a diagnosis of basicervical, midcervical, or transcervical femoral neck fractures. Exclusion criteria included pathologic fractures, periprosthetic fractures, and fracture non-unions.
This is a retrospective study of a single hospital system evaluating the observed cost of care for patients presenting with hip fractures from the emergency department, skilled nursing facilities and outside hospital transfers.
Statistical analysis
The data was utilized to examine differences in morbidity, mortality, cost, length of stay, and discharge disposition between hip fracture patients based on the individual point of origin prior to presenting to our institution. Each diagnosis, ASA score, Charlson comorbidity index, and surgical procedure performed were confirmed with individual chart review. For categorical variables, a Pearson chi-square analysis was performed.
RESULTS
A total of 223 patients met the inclusion criteria and were included in the study. The number of patients that presented primary to the ED at our institution, typically by EMS or medical transport, was 135 (60.54%). The number of patients that were transferred from an outside hospital to an inpatient unit or to the emergency department was 58 (26.01%). Lastly, the number of patients transferred from a SNF or intermediate care facility was 30 patients (13.43%). Patient cohorts and demographics are presented in Table 1.
Haug EC wrote and revised the manuscript and collected data; Pehlivan H and Macdonell JR contributed equally and helped design the study and collect data; Novicoff W did the statistical portion; Browne J, Brown T and Cui Q are the senior surgeons; and All authors contributed to this study equally.

ED patients and SNF patients were significantly older than OSH patients (= 0.001). ED and SNF patients were not significantly different from each other in age.
He couldn t have been more than four years old. With chubby2 checks and wispy3 blond hair going in several directions, he trotted4 behind his mother down the main aisle5 of the department store. His boots caught my eye. They were green. Really green. Bright, shiny, Kermit-the-Frog, green. Obviously new and a little too big, the boots stopped just below his knees leaving a hint of dimpled legs disappearing into rumpled6 shorts. Perfect boots for the rainy transition from summer to fall.
The coachman perceived that the shepherd wished to follow her, and warned him not to do so if he valued his life; but the shepherd wouldn t listen to his advice
Cost data analysis showed that OSH patients demonstrated significantly greater total cost for their hospitalization ($43302) compared to ED patients ($28875,= 0.000) and SNF patients ($28282,= 0.000). OSH patients’ costs per hospitalization average 149% and 153% of the cost per hospitalization of ED patients and SNF patients, respectively. There was no significant difference in total cost between ED patient and SNF patients (= 0.805). This data is summarized in Figure 1. For reference purposes, the average total inpatient cost for the 1540 elective total hip arthroplasties performed at our institution during the same time period as our study population is $22,182. Therefore, the non-elective hip arthroplasty patients’ costs per hospitalization average 193%, 130%, and 127% of the cost per hospitalization of elective total hip patients for OSH, ED, and SNF patients, respectively.
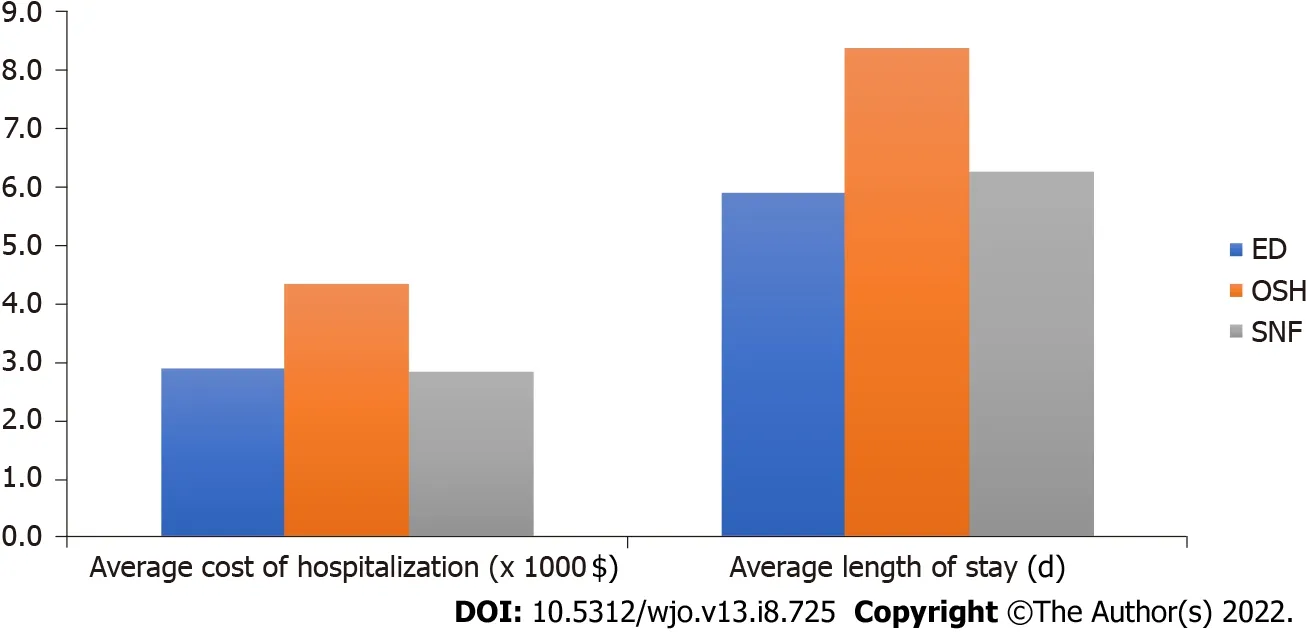
Average LOS was significantly greater in the OSH patients (8.38 d) compared to ED patients (5.89 d,= 0.003) and SNF patients (6.27 d,= 0.027). No significant difference was found between ED patients and SNF patients in average LOS (= 0.599). This data is also summarized in Figure 1.
And when she lay dead, the young King remembered what he had promised, and it made him shudder4 to think of lying in her grave alive, but there was no escape
Of the 135 ED patients, there were 3 in-hospital deaths (2.22%). There were 2 in-hospital deaths among the 58 patients transferred from outside hospitals (3.45%) and 3 in-hospital deaths among the 30 patients transferred from SNFs or intermediate care facilities (10.00%). Owing to the low number of mortalities, these differences did not reach statistical significance.
Average intensive care unit (ICU) days per hospitalization was significantly greater in the OSH patients (1.86 d) compared to ED patients (0.28 d,= 0.001) and SNF patients (0.80 d,= 0.002). There was no significant difference in ICU days per hospitalization between SNF and ED patients. This data is summarized in Figure 2.

It is clear from our data that patients transferred from an OSH more significantly strain the resources of the receiving tertiary care hospital compared to those patients who present primarily to the ED. This is an important finding in light of proposed bundled care programs. Bundled care programs, which can disincentive hospitals and providers from taking care of sick and costly patients, may increase the number of hip fracture patients being transferred to tertiary care centers especially with clear appropriate transfer guidelines lacking. This would further strain the resources of the receiving hospital and could potentially penalize those centers that are willing to provide care for these vulnerable patients. This is a strong argument for robust risk-adjustment models that potentially even include patient point of origin.
DlSCUSSlON
Transfers to regional trauma centers and tertiary care centers of critically ill and severely injured patients have been shown to decrease morbidity and mortality[15,16]. As one might expect given the illness severity seen in many of these transferred patients, increased morbidity, length of stay, blood transfusion requirements, and intensive care utilization has been previously documented in transferred patients[8,11,17]. To our knowledge, this study is the first to document this phenomenon in patients with femoral neck fractures being treated with arthroplasty.
The aim of this study was to compare demographic information, procedure utilization, cost differences, morbidity, and mortality in non-elective hip arthroplasty performed for fracture at an academic medical center based upon patient point of origin. With the nationwide implementation of bundled payments looming, determining the additional risks and costs associated with providing referral services for community and regional hospitals is essential. It is not surprising that patients transferred from an OSH incurred greater costs for their hospitalization than ED and SNF patients. Medically complex patients with significant comorbidities, associated injuries, or critical illness are often difficult for community hospitals to manage and are frequently transferred to tertiary care centers. Previous studies have also found increased cost with non-elective hip arthroplasty compared to elective total hip replacement[4,5].
This study is not without its limitations. We did not examine the reason for transfer to our facility. This analysis may have allowed us to subcategorize patients based on the indication for the transfer and further determine which specific patient groups or which comorbidities are most likely to lead to increased cost, prolonged hospitalization, increased morbidity, or mortality. Additionally, we did not examine surgical complications, readmissions, or transfusion requirements which are further indicators of morbidity. Another limitation is that this is a retrospective analysis of prospectively collected data. Finally, our entire study was limited to a single institution and is subject to institution specific policies and biases that may limit the generalizability of our conclusions. However, we feel that any tertiary medical center with a large referral basis is likely to find similar results.
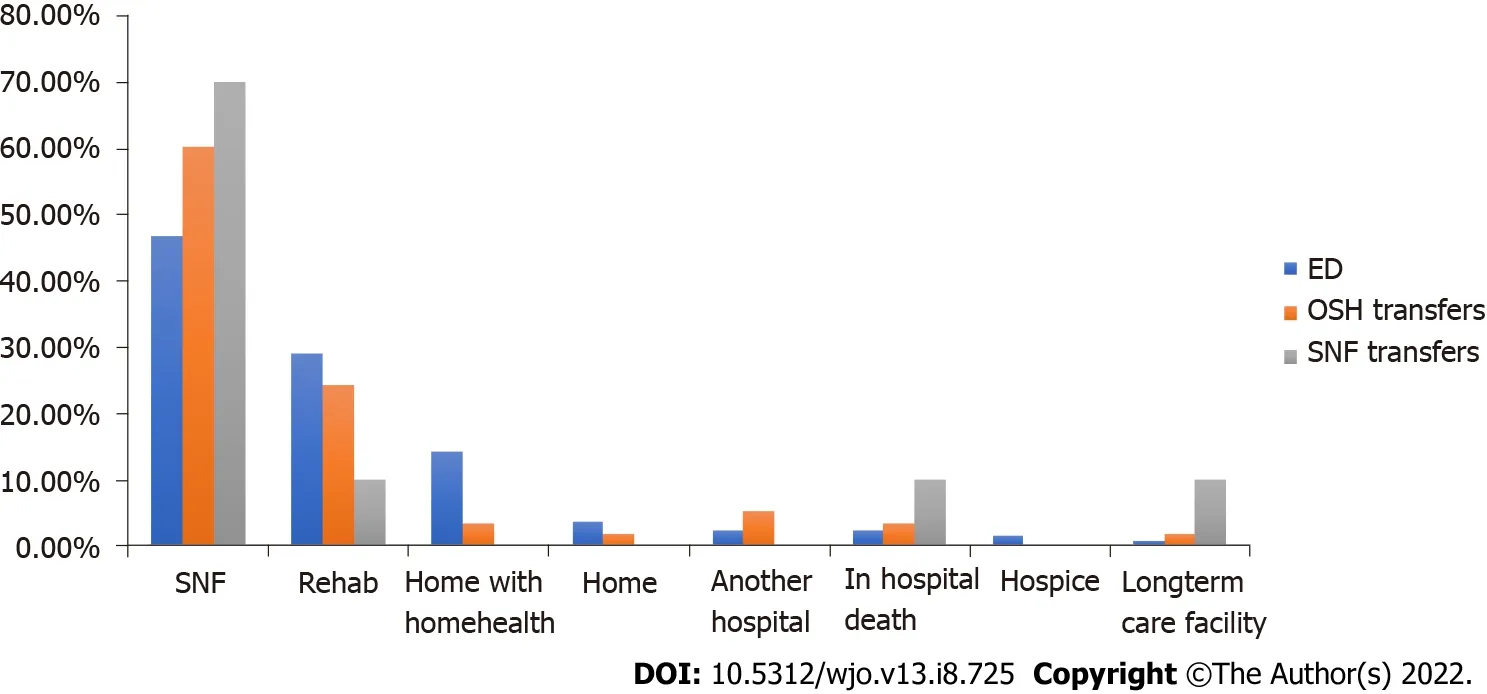
Analysis of patient discharge destination showed that ED patients were more likely to be discharged home than OSH and SNF patients. There were no other statistically significant differences in discharge destination based on point of origin. This data is summarized in Figure 3.
One obvious strength of our study is that it is the first to specifically look at cost and morbidity of hip fracture patients undergoing arthroplasty based on their point of origin. We were able to include a large number of patients over nearly a five year period. All total hip arthroplasty and hemiarthroplasty procedures were performed by three fellowship trained arthroplasty surgeons and therefore, variation in surgeon skill and experience is minimal. The data from our initial database was able to be corroborated through our electronic medical records and any disparities or omissions corrected. Finally, our study was able to determine differences in cost for hospitalizations, not charges, a more accurate representation of reimbursement from Medicare, Medicaid, or private insurance.
Our study showed increased length of stay and increased number of average ICU stays per hospitalization for transfered patients from an OSH compared to those patients presenting to our ED. These results are not surprising but demonstrate the greater burden OSH patients place on facilities, staffing, and healthcare providers. It may also reflect that a delay in getting the patient to the operating room can lead to medical complications and morbidity. Our study also found that ED patients were more likely to have ASA 1 or ASA 2 scores compared to SNF and OSH patients. Patients transferred from an OSH also incurred greater costs than those who presented primarily to our ED.
CONCLUSlON
Patients transferred from an outside hospital incurred greater costs for their hospitalization than patients presenting from an emergency department or SNF. This is a strong argument for riskadjustment models when bundling payments for the care of hip fracture patients.
Patricia handed her a box. I overheard4 you talking to your son yesterday, she said, and I know that it is hard to explain things to kids. This is a baseball glove for Jessie because he may not understand how important he is, even though you have to pay bills before you can buy gloves. You know we can t pay good people like you as much as we would like to; but we do care, and I want you to know you are important to us.
ARTlCLE HlGHLlGHTS
Research background
Rising healthcare expenditure, especially with the projected rise in total joint arthroplasty has lead the Center for Medicare Services to propose bundled payments.
Research motivation
Possible effects of bundle payments on tertiary hospital systems have not been evaluated.
The mound then opened, and his youngest daughter came out of it, and said, Why, father! why are you not coming in to see me? Oh, said he, if I had known that you lived here, and had seen any entrance, I would have come in
Soon after this the false bride30 said to the Prince: Dearest husband,31 I pray you grant me a favor. He answered: That I will. Then let the slaughterer19 cut off the head of the horse I rode here upon, because it behaved very badly on the journey. But the truth was she was afraid lest the horse should speak and tell how she had treated the Princess. She carried her point, and the faithful Falada was doomed20 to die.32
There was a larger percentage of ASA 4 patients amongst OSH and SNF patients and significantly lower percentage of ASA 1 and ASA 2 patients compared to the ED patients (= 0.001). There was no significant difference in average age-adjusted Charlson comorbidity index across all three groups. There was a significantly higher number of female patients (80.00%) who presented to the ED compared to transfers from OSHs (53.45%) and SNFs (53.33%) (= 0.000). There was a trend toward increased utilization of hemiarthroplasty in SNF patients compared to ED and OSH patients that did not reach statistical significance (= 0.070). Finally, there was no significant difference in race (whitenonwhite) between the three groups (= 0.583).
Research objectives
This study aims to evaluate potential effects of bundled payment systems on a large tertiary hospital system.
Research methods
The data collected for the patient safety initiative included age, sex, race, diagnosis, facility of origin, secondary diagnoses, American Society of Anaesthesiologists (ASA) score, length of stay, length of intensive care unit stay, total observed cost, charges, mortality, discharge disposition, and procedure codes. Total observed cost include all costs related to the arthroplasty procedure and subsequent inpatient care of the patient. The patient’s point of origin was determined to be our own institution’s emergency department (ED), outside skilled nursing facility (SNF) or intermediate care facility, and outside hospital (OSH). These locations were verified by reviewing the patient’s individual medical record. Patients who were transferred from an outside hospital or nursing facility to the emergency department were considered as transfers from an outside hospital or SNF, respectively. Patients who were transported to the emergency department from a physician’s office or urgent care were considered emergency department patients. Finally, two patients that were directly admitted from clinic with a diagnosis of femoral neck fracture were not included in the study as they were previously known to and followed by the treating team and could be a potential source of bias in the analysis.
Research results
Cost data analysis showed that patient transferred from an outside hospital demonstrate significantly higher costs compared to patients from a skilled nursing facility or the emergency department.
Research conclusions
Given the increased costs associated with patients transferred from outside hospitals this may call for a risk adjustment models when bundling for the care of hip fracture patients.
Research perspectives
Future research will have to further evaluate cost originators to adjust payment models appropriately.
This had gone on so long that now there were no men left, and he had been obliged to send his own daughter instead, and the poor girl was waiting till the monster got hungry and felt inclined to eat her
FOOTNOTES
The little mermaid could not help thinking of her first rising out of the sea, when she had seen similar festivities and joys; and she joined in the dance, poised116 herself in the air as a swallow when he pursues his prey117, and all present cheered her with wonder
The study was reviewed and approved by the Institutional Review Board of the University of Virginia and was IRB exempt.
None of the authors have any conflicts of interests to report for this study.
Dataset available from the corresponding author at qc4q@hscmail.mcc.virginia.edu.
The authors have read the STROBE Statement, and the manuscript was prepared and revised according to the STROBE Statement.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
United States
At last one of the other animals overheard him, and called out, Little hare, little hare! what is that you are saying? But the little hare hastily replied, I only asked you to pass me my stick
Emanuel C Haug 0000-0002-7655-6326; Hakan Pehlivan 0000-0002-7528-2386; Wendy Novicoff 0000-0002-5146-7706; James Browne 0000-0003-0367-7976; Quanjun Cui 0000-0003-4285-4488.
So she bought a large wrench6, and climbed up the tall 60 foot crane. She carefully climbed out onto the horizontal part of the crane, and unbolted one of the end sections. She happily climbed down and carried the steel section into her basement.
Ma YJ
A
When my oldest son was in high school, he planned to attend a Christian1 contemporary concert with the youth group from our church. To my amazement2, Aaron invited me to go along; he knew I enjoyed the music of one of the performers. I readily accepted; however, by the time the date of the concert arrived, I had questions about going. My youngest son, who has Down syndrome3 and progressive heart disease, had been ill, and I was concerned about him. My husband encouraged me to attend the concert, assuring me he was quite capable of taking care of our youngest. I wavered.
Ma YJ
杂志排行
World Journal of Orthopedics的其它文章
- Rates of readmission and reoperation after operative management of midshaft clavicle fractures in adolescents
- Bilateral hip heterotopic ossification with sciatic nerve compression on a paediatric patient-An individualized surgical approach: A case report
- Quantitative alpha-defensin testing: ls synovial fluid dilution important?
- Effect of pelvic fixation on ambulation in children with neuromuscular scoliosis
- Epidemiology of pelvic and acetabular fractures across 12-mo at a level-1 trauma centre
- Risk modeling of femoral neck fracture based on geometric parameters of the proximal epiphysis
