Development and validation of a rapid psychosocial well-being screening tool in patients with metastatic breast cancer
2022-07-31BhumiptThnsnsomboonSongphnChompryongNpPrinynitikulUthiTnlmiMnikWisssthornYupinPtrpongsnt
Bhumipt Thnsnsomboon ,Songphn Chompryong ,Np Prinynitikul ,Uthi Tnlmi ,Mnik Wisssthorn ,Yupin Ptrpongsnt
a Technopreneurship and Innovation Management,Graduate School,Chulalongkorn University,Bangkok,Thailand
b Department of Library Science,Faculty of Arts,Chulalongkorn University,Bangkok,Thailand
c Behavioral Research and Informatics in Social Science Research Unit,Sasin Graduate Institute of Business Administration,Chulalongkorn University,Bangkok,Thailand
d Division of Therapeutic Radiology and Oncology,Faculty of Medicine,Chulalongkorn University,Bangkok,Thailand
e Department of Accountancy,Chulalongkorn Business School,Chulalongkorn University,Bangkok,Thailand
f Department of Psychology,Faculty of Education,Ramkhamhaeng University,Bangkok,Thailand
Keywords:Breast neoplasms Focus groups Information seeking behavior Measurement Psychosocial functioning Quality of life
ABSTRACT Objective:The aim of this study was to develop and validate a rapid psychosocial well-being screening tool for metastatic breast cancer patients (MBC-PsySoc-Well-being).Methods:Applying a mixed method approach,the study was conducted in two phases.Phase 1,a focus group method was employed for item development,and three focus group sessions were conducted,with patients,caregivers,and medical professionals,respectively.Phase 2,validity and reliability testing were performed.Five experts reviewed items for content validity.Construct validity,criterion-related validity,internal consistency,and test-retest reliability were conducted among a sample of 53 patients with metastatic breast cancer.Results:Six themes were qualitatively analyzed based on focus group participants’responses.Eight items were then developed based on these themes.The index of Item-Objective Congruence scored by the experts ranged from 0.6 to 1.0.An exploratory factor analysis yielded three factors:Being curious and active in information seeking,Enthusiasm to return to a normal life,and Adjusting to positive lifestyle.The total scores of MBC-PsySoc-Well-being and the European Organization for Research and Treatment of Cancer’s Quality of Life Core Questionnaire (EORTC QLQ-C30) were moderately correlated (r=0.404,P=0.003).Cronbach’s α coefficient of the overall scale was 0.686.Pearson correlation coefficients of items between two tests within 14-day ranged from 0.410 to 0.673.Conclusion:This study represents an initiative to develop a rapid psychosocial well-being screening tool for patients with metastatic breast cancer.The results from validity and reliability testing indicate that the scale is moderately suitable for application to patients with metastatic breast cancer.However,a larger scale study should be further administered to confirm the validity and reliability of the measurement.
What is known?
• Psychosocial well-being plays substantial roles in the overall effectiveness of treatment and prognosis of patients with metastatic breast cancer (MBC).
• It would be helpful for healthcare professionals to observe psychosocial-oriented well-being of MBC patients continuingly throughout the patient's treatment journey.
• There are an abundance of developed instruments measuring psychosocial-oriented quality of life for cancer patients.They tend to be lengthy and require a great amount of time and effort to complete which can be challenging to be used on a routine basis.
What is new?
• Six themes were extracted based on insights obtained from patients,caregivers,and healthcare professionals about psychosocial well-being of MBC patients,including 1)Being curious and active in information seeking,2) Aspiring to be healthy,3)Willingness to treatment adherence,4) Adjusting to positive lifestyle,5) Hope,and 6) Enthusiasm to return to a normal life.
• An 8-item rapid screening tool was developed and evaluated to observe psychosocial well-being of MBC patients.The scale was designed to be easily utilized by healthcare professionals in various stages of treatment,care,and settings.
• The developed scale,MBC-PsySoc-Well-being,can be used as a standalone measure or may also be used as a supplement to other schemes of quality-of-life evaluation.
1.Introduction
Breast cancer is a common disease worldwide.Approximately 0.5 million people worldwide die from metastatic breast cancer(MBC) every year;however,prognosis in such cases varies depending on BC subtypes which mostly are rarely cured by current systemic therapies [1].Treatments for MBC,using palliative chemotherapy,endocrine therapy,and/or targeted approaches,impact disease control,increase progression-free and overall survival,and improve quality of life.
Findings from a previous study show that almost 74%of patients with breast cancer experience chronic pain for up to 7.4 years since diagnosis [1].Physical problems related to pain that can affect quality of life include fatigue,tiredness,nausea,anorexia,arm swelling,hair loss,and weight loss,among others.Although,there have been attempts to improve the quality and efficacy of physical disease treatment provided by medical systems,the effectiveness of therapy also depends on the mental health and well-being of patients living with the disease.
Patients with chronic diseases including MBC patients,who need continuous treatment for an extended period,present with important changes in quality of life[2].The key goal of MBC therapy is to prolong survival,with an emphasis on restricting treatmentrelated toxicity as far as possible [3];however,the key issues and problems faced by patients with MBC are emotional and psychological[4].Surviving patients are concerned about their daily lives,during and after treatment,such as returning to work,social life,living expenses,and disease recurrence [5].These issues cause uncertainty about the future for patients who want to return to normal and healthy life [6].Anxiety and depression are the most prevalent psychiatric symptoms in patients with breast cancer.If untreated,such symptoms can have long term psychological effects that reduce quality of life [7].
Numerous research studies report that 90% of patients undergoing breast cancer surgery have dramatic psychological effects on the quality of life of breast cancer survivors [8].The psychological issues would still be carried over up to 5 years after receiving a surgery[9].Such psychiatric disorders have significant impacts on patient psychosocial well-being,self-care,adaptability to treatment,and,over the course of time,cancer severity and prognosis,as well as response to treatment [10].Hence,the diagnosis and remediation of psychiatric conditions can be helpful in increasing treatment consistency and patients’ psychosocial well-being [11].
Psychosocial well-being can normally be improved through social support,which can stimulate behavioral changes through various social factors,such as promotion of mental and emotional health,information seeking,and self-assessment [12].In addition,rehabilitation support can improve patient feelings of self-efficacy,particularly in difficult times,and reduce emotional distress and mood disorders [13].Therefore,early and effective observation of MBC patients’psychosocial state during a routine clinical practice is essential to provide sufficient and appropriate support [14].Generally,MBC patients’ mental health is fluctuated dynamically due to the rapid and drastic transition of physical health and other psychosocial factors in response to treatment routes[15].Hence,a screening tool that could help healthcare professionals quickly assess and/or monitor the psychological state of MBC patients during clinical visits is essential for effective comprehensive care[16].
The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30(EORTC QLQ-C30)and the European Organization for Research and Treatment of Breast Cancer Quality of Life Questionnaire (EORTC QLQ-BR23) [17] are among the most adopted instruments to evaluate quality of life of breast cancer patients.Moreover,the World Health Organization Quality-of-Life Scale (WHOQOL-BREF) [18],the Satisfaction with Life Domains Scale for Breast Cancer (SLDS-BC) [19],and the Medical Outcome Study 36-Item Short Form Health Survey(SF-36)[20] also have been used for evaluating quality of life of breast cancer patients.However,these instruments tend to focus more on physical health and center less on psychosocial well-being.The understanding of attitudes and behavior toward the end of life may help MBC patients to endure negative aspects of poor health and the side effects of treatment [21].While the existing comprehensive quality of life measures for cancer and breast cancer patients have been reportedly used in MBC patients[22],these instruments are not specifically developed for MBC patients[23],given that the goal of treatment of MBC is distinct from the treatment goals of cancer or breast cancer,in general.Particularly,the emphasis of palliative care for MBC patients should rather address psychosocial well-being[24].Besides,the currently available measurements are quite lengthy,making them impractical to be administered to patients having limited or deteriorating physical health.
The objectives of this study were to develop a rapid instrument to evaluate the psychosocial well-being of MBC patients as well as to assess the validity and reliability of the instrument.Psychosocial well-being,in this context,is defined as a cognitive state,including perception,attitude,and emotion,of an individual reflecting the quality of relationships with others in any social groups to which s/he belongs [25,26].The observed construct,psychosocial wellbeing,is considered temporal and dynamic in nature.The goal of the development of this instrument is to create a tool that can be easily utilized by healthcare professionals in diverse settings with MBC patients undergoing various stages of treatment.
Based on a review of relevant literature such as social cognitive theory [27],and cognitive behavior therapy [7,28],psychosocial well-being can be characterized into three major dimensions including affection,cognition,and behavior.These three dimensions were used as an initial framework to develop a rapid psychosocial well-being screening tool for MBC patients.They were also used to evaluate the content validity of the newly developed screening tool.
2.Methods
2.1.Study design
Based on the COSMIN reporting guideline of studies on measurement[29],this study employed a mixed-method approach to develop and validate a rapid psychosocial well-being screening tool in MBC patients,consisting of two phases,1)item development and 2)validity and reliability testing.The goal of the first phase was to generate questions relevant to the psychosocial dimensions of MBC patients’ well-being.The second phase involves assessments of construct validity,content validity,criterion-related validity,internal consistency,and test-retest reliability.
Due to different methodologies employed in both phases,the details about participants as well as data collection and analysis are grouped by study phases consequently.
2.2.Phase 1:Scale development
2.2.1.Participants
To gain an insight in terms of the psychosocial well-being of MBC patients,three focus group sessions were conducted,with patients,caregivers,and medical professionals in March 2020.The diversity among key informants addresses the triangulation of data sources.
The first group of informants comprised 8 patients with MBC.By using a combination of convenience and purposive sampling technique,the patients who had an appointment on the day of the focus group sessions were invited.The selection of invited patients was based on the evaluation of their perspectives toward the prognosis and treatment by the nurse case manager and physicians in charge.It is noteworthy that patients with MBC are very heterogeneous in general (common traits).Thus,the selection of participants also considered various extents of metastasis and treatment modality.The number of informants in each session was based on Morgan’s guideline published in the Annual Reviews of Sociology,which was approximately 8-12 people[30].All patients must meet the following inclusion criteria:1) 30-70 years old female,2)diagnosed with MBC within 12 months,and 3)being able to consciously communicate and not being bed-bound.Bed-bound patients were excluded due to their physical limitations to access the study site.The exclusion criteria were:1)patients who had not received treatment at Chulalongkorn Hospital,2) patients who were at risk and may be in danger during the research period,3)unwilling/unable to give consent or unable to join focus group meetings.
Among all informants in the patient group,4 participants were between 31 and 40 years old(mean=38.5),6 employed,5 married,and 3 singles.The majority(6)of informants had personal income between 10,000 and 30,000 baht per month (1 baht=0.03 US$).Four informants had been diagnosed with MBC for 9-12 months,3 participants for 1-3 months,and 1 participant for 3-9 months.Furthermore,4 participants were receiving hormone therapy,2 participants were receiving chemotherapy,and another 2 receiving chemotherapy and radiotherapy.
Adopting a convenience sampling method,the second group comprised 5 caregivers of the informants in the first group.The following inclusion criteria were used to screen for eligibility:1)currently providing any kind of support and are biologically or socially related to patients,2)agreed to participate in the research,and 3) being able to consciously communicate.The exclusion criteria include 1)professional healthcare providers who were not biological or socially related to patients,and 2)unwilling/unable to give consent or join the focus group sessions.
Almost all of the participants,except one,in the caregiver group were older than 40 years old.Three participants were business owners and 2 were unemployed.In terms of relationships with MBC patients,3 participants in this group were spouses of the patients in the first group and 2 were family members.
Also,using a convenience sampling method,the third group included 3 oncology medical professionals.The included informants in this group were physicians and professional nurses specializing in oncology who was in charge of MBC patients at the Faculty of Medicine,Chulalongkorn University.In this group,there were 2 oncologists and 1 registered nurse.All informants in this group had worked for more than 10 years as medical professionals.At the study site,there were,in total,2 oncologists and 4 registered nurses in the outpatient breast cancer clinic.Both oncologists who specialized in breast cancer and were in charge of all breast cancer in the clinic participated in the focus group.Due to the time constraint with other nurses,only the nurse case manager participated in the focus group.While the number of participants in this group may seem small for a focus group session in general,the participants represented almost half of the staff in the department.
2.2.2.Data collection and analysis
The setting of the focus group sessions was an oval-shaped meeting room.Each session took approximately 90 min.BT was the main moderator of all sessions.Semi-structured questions,developed based on relevant literature on the psychosocial wellbeing of MBC patients from both patients’ and caretakers’ perspectives[23,31,32],were used as guidelines to conduct sessions.
The questions used in the first session covered patients’ experiences,reactions,thoughts,emotions,behavior,coping strategies or mechanisms,and social support after being diagnosed with MBC.The construction of the questions and probing strategies to obtain insights from the participants also concerned the psychosocialoriented quality of life from both negative and positive sides.
The second focus group session addressed how caregivers perceived patients’ experiences and reactions,how they aided the patients (particularly emotional and behavioral support),and how they managed changes in their own lifestyle and family relationship.
The focus group session with medical professionals included questions regarding the process of communicating difficult situations,the perceptions about factors influencing patients’treatment plans (particularly those associated with psychosocial well-being aspects),and how they managed the communication issues and gaps between patients and medical professionals.
All focus group sessions were moderated,recorded,and transcribed verbatim by BT (the first author).The transcriptions were redacted for privacy protection and coded using NVivo version 10.The coding was based on thematic analysis approach.All codes were reviewed by a subject expert in psychology to ensure the quality of the coding process and its outcomes.Cluster analysis was performed based on coding similarity and reviewed by BT,SC,NP,UT,and MW to generate the relevant themes and operational definitions.The resulting themes and codes were then used to construct questions.In addition,the question development process also considered the coverage of all psychosocial dimensions (i.e.,affection,cognition,and behavior) found in previous literature.
2.3.Phase 2:Validity and reliability testing
2.3.1.Participants
To validate the developed scale,we recruited 53 MBC patients from a medical oncology unit at Chulalongkorn University in Bangkok,Thailand.By employing a convenience sampling technique,the patients were invited to complete the developed scale from the first phase based on their availability and willingness at the clinic at the end of the visit in October 2020.The decision on sample size was primarily based on available resources which were constrained by limitations of the recruitment method and the small size of the population in the study site,approximately only 200 MBC patients a year.In addition,relevant recommendations on sample size for an initial scale development study indicate that the number of 30 participants is reasonable minimum sample size for a pilot study of an initial scale development[33].Moreover,based on simulations conducted by Winter,Dodou,and Wieringa [34],an exploratory factor analysis with a sample size of 50 or below can yield reliable results,even with a minor degree of some distortions.Additionally,Kaiser-Meier-Olkin (KMO) test and Bartlett’s Test of Sphericity were performed to evaluate the adequacy of the sample size of this study at this phase.The inclusion and exclusion criteria were the same as the criteria used to recruit patients in Phase 1.
In terms of demographics,most of the participants(81%,43/53)were older than 40 years old (mean=48.7),36 participants (68%)were employed,27(51%)married,and 26(49%)single.The majority(74%,39/53) of participants had personal income between 10,000 and 30,000 baht per month.In this phase,19 participants (36%)were receiving hormone therapy,21(40%)receiving chemotherapy,and another 13 (25%) receiving both chemotherapy and radiotherapy.Only one participant in Phase 1 was included in the second phase.All 53 participants completed all instruments without missing data.
2.3.2.Data collection and analysis
The administration of the questionnaire was conducted at the clinic using a paper-based form.In addition to the newly developed scale,MBC-PsySoc-Well-being,the participants were asked to complete EORTC QLQ-BR23 and EORTC QLQ-C30 scales.The participants were also asked to complete a 14-day follow-up questionnaire containing MBC-PsySoc-Well-being.
To address the various dimensions of validity and reliability of the scale,this phase involved multiple analyses.
To assess the content validity,5 subject experts in psychology evaluated each item on the ordinal scale (+1,0,or -1) as having high to low degree of relevance to the objective of the questions(including themes and psychosocial dimensions).The index of Item-Objective Congruence (IOC) was calculated to evaluate the content validity for each item.The cutoff score of the index used in this study is 0.5,according to Rovinelli and Hambleton [35].
To evaluate construct validity,principal component analysis(PCA) method using Varimax rotation was applied to explore factors among all items.Prior to applying PCA,the result from an itemtotal correlation analysis shows that all items that are mildly correlated with the overall scale (r ≤0.2) [36].The results from KMO test (0.71) and Bartlett’s test of sphericity (P <0.001) also indicate that the sample size is sufficient for factor analysis and PCA can be an appropriate method for factor analysis.The report on construct validity testing only includes results from the PCA method.
Apart from the newly developed items,the questionnaire also includes items obtained from EORTC QLQ-BR23 (8 items from functional scales and 15 items from symptom scales) and EORTC QLQ-C30 (2 items from global health status,15 items from functional scales,and 13 items from symptom scales).The responses from these questionnaires were used as controlled measures in the assessment of criterion-related validity by assessing correlations between relevant measures.
In terms of reliability,the data collected from the first survey was also used to evaluate the internal consistency,which was assessed by using Cronbach’s α coefficient.For test-retest reliability,an additional follow-up survey with the same group of participants was conducted 14 days after the initial survey.All participants completed the follow-up survey (100% follow-up rate).While the first survey was conducted using the paper-based form,the second survey was conducted online due to the impact of COVID-19 and the availability of the patients.The order of the question statements of the second test was the same as the first test.We tried to replicate the paper form onto the online form as much as possible.Therefore,the responses from the follow-up test were also used to address parallel form reliability which addressed potential bias obtained from different methods of data collection,although early studies show that data collected via the online method had the same quality as the paper-based method [37-39].
2.4.Ethical approval
This study was approved by the institutional review board of the Faculty of Medicine,Chulalongkorn University,Thailand,(IRB NO.543/62)and conducted in compliance with international guidelines for protection of humans in research,according to the Declaration of Helsinki,The Belmont Report,the CIOMS Guideline,and the International Conference on Harmonization in Good Clinical Practice(ICH-GCP).All participants into the study were voluntary after being informed of the information of the study by the physician and research team then written informed consent.Patients’privacy and confidentiality were always maintained in all items in accordance with the Declaration of Helsinki.
3.Results
3.1.Constructs of psychosocial well-being of MBC patients
The verbatim transcripts from the focus group were grouped into 50 codes regarding psychosocial well-being of patients with MBC.Based on coding similarity,the cluster analysis method categorized all codes.Then,the results were grouped into six themes:Being curious and active in information seeking,Aspiring to be healthy,Willingness to treatment adherence,Adjusting to positive lifestyle,Hope,and Enthusiasm to return to a normal life.The description and selected verbatim quotes of each theme are examined below.
Theme 1:Being curious and active in information seeking describes an interest to know about their own health status,illness,and the approach to treating their illness.It also includes patients’eagerness to assess whether they had insufficient information or knowledge and seek additional knowledge or information.
“At first,I didn’t know what metastatic meant,then,I went home and searched on YouTube to find out about what metastatic was.”(Patient #1)
“I started looking for information related to the disease.I found that we all have cancer cells.That’s just when they showed symptoms.”(Patient #5)
“When I got chemotherapy,I read a lot of information,I follow the doctor’s directions on how to prepare myself,and what I have to do.” (Patient#8)
“Most of the patients knew that they have metastatic breast cancer.They desired to know the progress of the disease.Most of them replied that they wanted to know.” (Medical professional #1)
“I always ask the patient how it has been received all information from the doctor.Do you have any questions about the issue you discussed with the doctor?Do you know your doctor’s approach for the next step?” (Medical professional #3)
Theme 2:Aspiring to be healthy refers to behaviors and/or perceptions that encourage patients to be healthier.
“She has always been a very positive person and strongly believed that she will get rid of the disease.” (Caregiver #2)
“I have tried to exercise every day in the morning.” (Patient #6)
“[I am]trying not to be stressed by watching the movies and doing the housework.” (Patient #8)
“The patient is trying to eat as recommended to keep them healthy to be ready for further treatment.” (Medical professional #1)
Theme 3:Willingness to treatment adherence refers to cooperation with treatment,by strictly following the doctor’s instructions.From a psychological perspective,adherence also implies a willingness to overcome all obstacles for an improvement of health status.
“I strictly follow the doctor’s instructions.” (Patient #3)
“I always take medicine on time,stop drinking alcohol,and follow up with a doctor’s appointments.” (Patient #7)
“Assessing the overall factors such as never missing an appointment,having relatives come along with them,not losing weight and being ready for the treatment.” (Medical professional #2)
“One week before an appointment for chemotherapy,she will sleep more and take a rest as much as she can to keep her body healthy.”(Caregiver #3)
Theme 4:Adjusting to positive lifestyle refers to improvements in lifestyle and modification of various aspects of behavior.
“I have to start taking care of myself seriously because,in the past,I never paid attention to it.” (Patient #2)
“[I am trying to]be better in my daily lifestyle such as going to bed early,strictly eating on time.” (Patient #5)
“The positive thing is that the patients have adjusted their lifestyle and behaviors such as stopping drinking,stopping smoking,and taking care of their dietary.” (Medical professional #2)
Theme 5:Hope refers to feelings of hope or encouragement from people around the patient,such as family,friends,and the need for support from society.
“I want to help society in ways that I have not done before,such as donating things for other people.” (Patient#4)
“I was shocked,but I had to control my emotions and calm down my sister,I knew that this disease is serious,but there must be a solution.” (Caregiver #5)
“People around me and my colleagues encourage me and cheer me up.So I feel that I’m not living alone.” (Patient #1)
“Sometimes patients like to talk and encourage each other because being in the same situation would make them understand each other like treatment experience,and like a friend helping a friend.”(Medical professional #1)
Theme 6:Enthusiasm to return to a normal life refers to an attempt or activity to maintain a normal lifestyle.It also includes an implication that a patient wishes to continue their usual lifestyle,despite illness.
“I’m still working as usual.” (Patient #8)
“I wake up every day and try to do normal daily activities like I am not an ill person.” (Patient #5)“She said,she wanted to recover from the disease because there is still a lot of work to do,and our children are young.”(Caregiver#4)“The patient is trying to do everything to recover from the disease and be able to return to a normal life.”(Medical professional#3)
3.2.Item statements and measurement scale
Based on the above themes,eight statements regarding psychosocial well-being were constructed as illustrated in Table 1.The phases and terms used in these statements adopted the informant’s verbatim quotes (particularly from the patient group) as much as possible.In addition to emerging themes from focus group sessions,the construction of questions was conducted in juxtaposition to cover all psychosocial dimensions of quality of life (i.e.,affection,cognition,and behavior).Questions 1,7 and 8 represent the affective dimension.Question 2 covers the cognitive dimension.Questions 3,4,5,and 6 address the behavioral dimensions.
To measure how likely the participants agree with the developed statement,a four-point Likert scale was applied ranging from 1 (I strongly disagree) to 4 (I strongly agree).It is noteworthy that the eight items of the proposed psychosocial well-being scale developed and tested in this study are in Thai(see the Scale in Thai version in Appendix A).The English-translated version,as shown in Table 1,has yet to be validated in the future.
3.3.Validity testing
The results of validity testing of MBC-PsySoc-Well-being can be divided into three parts,content validity,construct validity,and criterion-related validity.
3.3.1.Content validity
To evaluate the content validity of the scale,5 experts who are university lecturers and hold a doctoral degree in varying subfields of psychology,including counseling psychology,clinical psychology,and developmental psychology,reviewed the relevance of items with the designed themes,the psychosocial dimensions,and the applicability in the target population.The responses from experts were analyzed using the Index of statistics.Item 3 has the lowest IOC score(0.60),while other items have a score between 0.8 and 1.0.Since the IOC scores of all items are higher than 0.5,none of the eight items was removed.
3.3.2.Construct validity
An initial PCA was conducted to identify the number of components based on Eigenvalues and cumulative component loading.As shown in Fig.1,the eight items can be categorized into three components,which can explain approximately 73.15% of the variance.Subsequently,PCA using Varimax rotation was performed on the retained eight candidate items.As a result,the rotated factor loadings as well as the visualizations clearly yield the division of eight items into three groups(Table 2).(see the visualizations of the three-Component PCA using Varimax Rotation in the appendices).
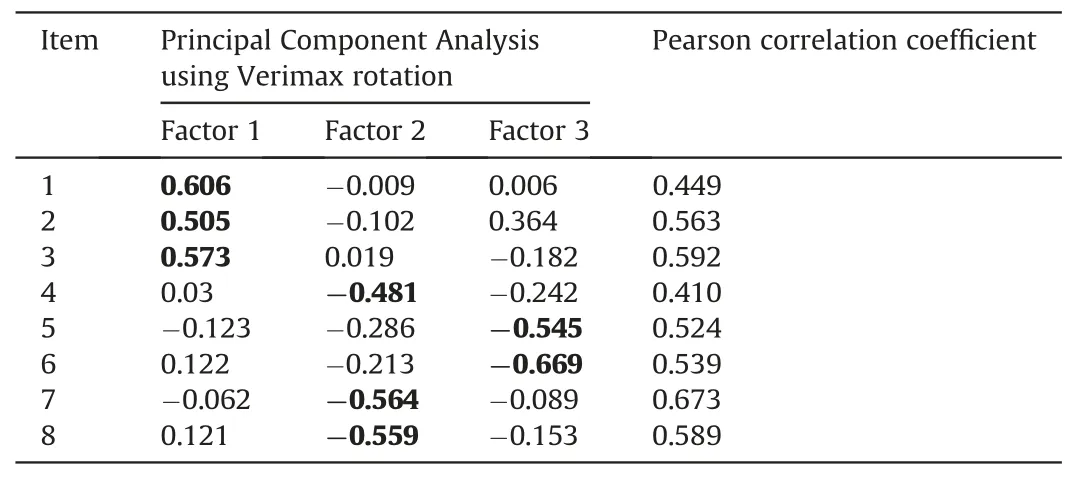
Table 2 Principal Component Analysis using Varimax rotation,and Pearson correlation coefficient between two tests as test-retest reliability index of MBC-PsySoc-Well-being(n=53).
Based on the classification of items as well as supported by relevant literature,the three components can be identified as the following constructs:1) Being curious and active in information seeking(Items 1-3),2)Enthusiasm to return to a normal life(Items 4,7,8),and 3) Adjusting to positive lifestyle(Items 5,6).
Being curious and active in information seeking represents the desire and ambition to actively find information about their symptoms and treatment plan.Being curious can be associated with openness to a broader range of treatments as well as acceptance of support from several sources [40].The desire for moreinformation and the curiosity about their disease can drive patients to seek and use information sources to achieve a better understanding of the disease and treatment [41].As a result,this construct typifies the dynamics of changes in coping strategies and is one of the essential mechanisms to improve patients’ quality of life [42,43].
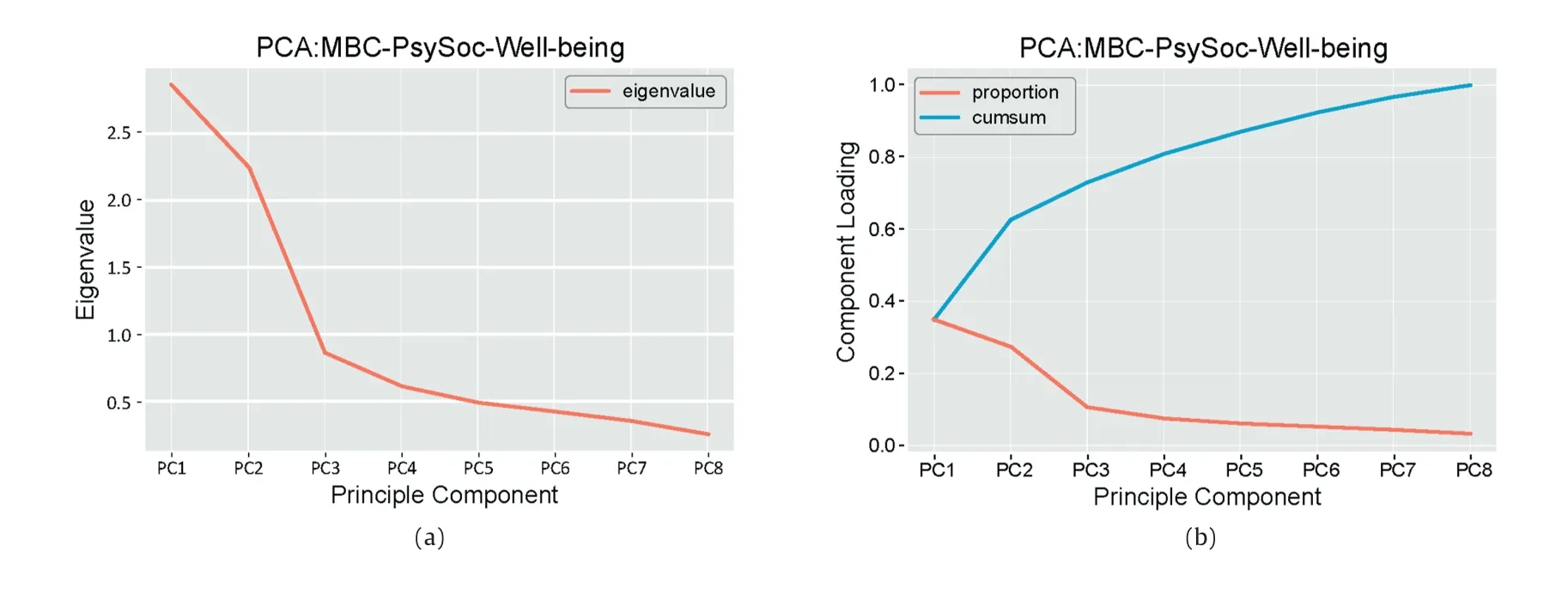
Fig.1.Eigenvalue and Component Loading of an initial Principal Component Analysis.
Enthusiasm to return to a normal life primarily concerns an expectation and self-evaluation in different prospects of life in comparison to life prior to being diagnosed with the illness.Activities of concern include,for instance,disclosing the diagnosis to their employers and relatives,dealing with uncertainties about physical appearance,and actively working during and after treatment sessions [44].
Adjusting to positive lifestyle refers to changes in everyday life activities,personal beliefs,and lifestyle as a coping mechanism with the illness [45].Resilience has been widely discussed as an indicator of quality of life of breast cancer patients [46].This construct can also be implied to the level of self-efficacy to maintain a healthy lifestyle and positive mental health [9].
3.3.3.Criterion-related validity
To assess criterion-related validity,the responses of the new scale were compared with two related instruments (i.e.,EORTC QLQ-C30 and EORTC QLQ-BR23).Pearson correlations were performed among total scores of these three instruments and among total scores in the subscale level.
The total scores of MBC-PsySoc-Well-being and EORTC QLQ-C30 were moderately correlated(r=0.404,P=0.003).The coefficient of Pearson correlation between total scores of MBC-PsySoc-Wellbeing and EORTC QLQ-BR23 is 0.200 (P=0.155) indicating a mild correlation.This may be due to the fact that EORTC QLQ-C30 contains items somewhat related to overall wellbeing in the Global Health Status,Role Functioning,and Social Functioning subscales.On the other hand,the items in EORTC QLQ-BR23 mostly address functional and symptom constructs.
Statistically significant moderate correlations(r ≥0.3,P<0.05)between total scores in the subscale level were also found in certain pairs,mostly ones with subscales of EORTC QLQ-C30.Being curious and active in information seeking in MBC-PsySoc-Well-being is moderately correlated with Emotional functioning (r=0.583,P <0.001) and Social functioning (r=0.305,P=0.026) in Functional scales of EORTC QLQ-C30.Emotional functioning refers to a feeling of being tense,worried,and depressed,while Social functioning reflects physical condition or medical treatment that interfered with family life and social activities.Emotion and the desire for information can usually be cooccurring.After being diagnosed,MBC patients may respond to difficult news or situations with emotion then followed by reactions showing that they are curious and seek more information[47,48].It is also found in other studies that cancer patients suffering from their treatment were curious about their daily life during and after treatment[49].
There are also moderate positive correlations between Curiosity about the illness and some symptom scales in EORTC QLQ-C30 including Fatigue (r=0.377,P=0.005),Dyspnea (r=0.305,P=0.026),and Insomnia (r=0.456,P=0.001).In this regard,symptoms including fatigue,nausea and vomiting are normally a primary concern for patients undergoing cancer treatment[50].By having these symptoms,cancer patients pay more attention to the experiences of the present moment which can lead to being curious about their health status [51].
Adjusting to positive lifestyle is moderately correlated with role functioning (r=0.344,P=0.012) in Functional scales of EORTC QLQ-C30.Role functioning includes limitations or obstacles in performing either work or other daily activities.This is supported by activities of daily living which are defined that individuals generally perform for themselves as part of their daily selfadjustment [52] and the cognitive behavioral therapy.This significantly improved insomnia symptoms and patients’ well-being[53],supporting moderate positive correlations with insomnia(r=0.344,P=0.012) in Symptom scales of EORTC QLQ-C30.
For correlations with subscales in EORTC QLQ-BR23,Curiosity about the illness is moderately correlated with two constructs in Functional scales of EORTC QLQ-BR23,Body image (r=0.301,P=0.029),and Future perspective (r=0.588,P <0.001).Body image refers to a feeling about being physically attractive and feminine.At the same time,Future perspective refers to patients’concerns about their health in the future.For women who had undergone mastectomy due to breast cancer,they were highly concerned about their body image and,therefore,would possibly seek more information about body disclosure and reconstruction[54,55].For the association with Future perspective,it is typical for cancer patients to be curious and feel uncertain about cancer recurrence [56].
3.4.Reliability testing
The results of reliability testing of MBC-PsySoc-Well-being can be divided into two parts,internal consistency,and test-retest reliability.
3.4.1.Internal consistency
For internal consistency,Cronbach’s α coefficient of the overall scale was performed.As a result,the overall scale had a low degree of internal consistency(α=0.686).In addition,all three constructs had a high degree of internal consistency (α=0.793 for Being curious and active in information seeking;α=0.725 for Enthusiasm to return to a normal life;α=0.698 for Adjusting to positive lifestyle).
3.4.2.Test-retest reliability
The administration of the second test of the newly developed scale was conducted 14 days after the first test.Pearson correlation efficient analysis was performed to indicate the test consistency over time as shown in Table 2.As a result,seven items(Items 1-6,8)had a fair consistency between two tests(0.40 ≥r ≥0.59),while Item 7 had a good consistency(0.60 ≥r ≥0.74).The threshold was adopted from Chichetti [57,58].Perhaps due to the small sample size and the likelihood of drastic change in quality of life of the participants,none of these items has a high level of test-retest reliability.Thus,all items should be investigated further in a study with larger samples [59].
4.Discussion
4.1.Measurement properties of MBC-PsySoc-well-being
The measurement properties of the scale evaluated in this study include content validity,construct validity,criterion-related validity,internal consistency,and test-retest reliability.
In terms of content validity,the IOC scores of all items were higher than 0.5,which is satisfactory to include all items.Construct validity evaluated by conducting PCA yielded three principal constructs:1) Being curious and active in information seeking (Items 1-3),2)Enthusiasm to return to a normal life(Items 4,7,8),and 3)Adjusting to positive lifestyle(Items 5,6).Criterion-related validity of the scale was tested against two related instruments including EORTC QLQ-C30 and EORTC QLQ-BR23.Low positive correlation was found between the total scores of MBC-PsySoc-Well-being and EORTC QLQ-C30,while the correlation with the total score of EORTC QLQ-B23 was very low to none.In a subscale level,moderate positive correlations were found between Being curious and active in information seeking of MBC-PsySoc-Well-being and Emotional functioning and Social functioning in Functional scales of EORTC QLQ-C30.Low to moderate positive correlations between Curiosity about the illness of MBC-PsySoc-Well-being and certain Symptom scales in EORTC QLQ-C30 including Fatigue,Nausea and vomiting,Dyspnea,Insomnia,and Appetite loss are also presented in the analysis [50,51].Curiosity about the illness of MBC-PsySoc-Wellbeing is also found to be moderately correlated with two constructs,Body image and Future perspective,in functional Scales of EORTC QLQ-BR23[54-56].These correlations seem reasonable and can be supported by relevant literature.
The results of reliability testing are divided into 2 parts.Using Cronbach’s α coefficient of the overall scale,the three constructs had a high degree of internal consistency.For reliability between two tests performing 14 days apart,only Item 7 had a good level of reliability on this regard [57,58].For other items,the test-retest reliability results can be interpreted as fairly reliable.
It seems understandable that test-retest reliability did not show a relatively high consistency.It can be explained by two major reasons.Firstly,the administration of the first test may affect patients’ awareness of the disease.Their emotions,perceptions,attitudes,and behaviors may change as triggered by the statements in the questionnaire.Secondly,MBC patients may have drastic changes in overall health due to treatment side effects and physical deterioration which also impact psychosocial well-being.The 14-day period may be challenging to evaluate test-retest reliability in a dynamic population and context in this study.
Another possible rationale considers the impact of palliative care that may help improve quality of life which might subsequently have an impact on some results.However,the patients in this study were diagnosed in an early timeline (i.e.,less than one year).Palliative care has either rarely been provided or at the early.Besides,the 14-day period might be too short to evaluate the impact of palliative care.Therefore,receiving palliative care might not be considered as a major determinant in this study.
The overall results of the validity and reliability tests are moderately satisfied,with major concerns about reliability of certain items.As an initial development,the scale can be further improved in multiple directions.
4.2.Practical relevance and generalizability
We describe the development of a rapid psychosocial well-being screening tool in patients with MBC,particularly from a positive perspective.The goal of MBC treatment is to prolong patient survival and ensure better quality of life.Patients with MBC are concerned about many areas of their daily life as well as effects during and after receiving treatments.Patients with poor quality of life can have an impact on overall treatment and prognosis[60,61].Therefore,it would be more useful to have a tool for attending physicians or medical team members to be informed about the patient's psychosocial state in a convenient manner.
In previous studies,standard questions related to quality of life in breast cancer patients have been framed in a negative tone and mostly focused on physical health [17].The WHOQOL-BREF [18],the SLDS-BC[19],and the Medical Outcome Study SF-36[20]have also been used for evaluating quality of life of breast cancer patients.Since psychosocial well-being should be considered from an integrative perspective [62,63],an instrument that adds consideration of psychosocial well-being aspects to the existing measure is essential to comprehensively and efficiently observe in psychosocial well-being of MBC patients[64].Unfortunately,in the previous studies,there are no psychosocial well-being screening tools to be found specifically for MBC [65,66].
Nevertheless,in the context of the healthcare system for MBC patients with limited resources like in Thailand and other developing countries,an effective psychosocial screening tool is considered a critical part of preventive care in outpatient clinical practice for MBC patients.Ideally,medical professionals should be able to evaluate patients’ quality of life before undergoing each treatment.However,employing those comprehensive and conventional questionnaires for quality of life in MBC patients before beginning a new treatment or undergoing treatment on a routine basis is very challenging because it requires tremendous effort and resources from all stakeholders.MBC-PsySoc-Well-being scale is promising to make the evaluation easy and acceptable.
4.3.Strengths and limitations
This study reports the initial development of a short,concise,and easy-to-use psychosocial wellbeing screening tools for MBC patients in outpatient clinics.While the results of measurement property evaluations might not be more robust than other comprehensive quality of life scale developed,MBC-PsySoc-Wellbeing was proven to be a fair instrument to be administered even with relatively small sample size.
It is noteworthy that the limitations of the sample size were remarked and managed from the item development stage.Traditionally,items were developed directly based on qualitative analysis.Several studies used individual codes to develop questions.Nonetheless,in this study,we decided to focus on the final themes,rather than codes,to improve the efficiency of the scale development.Initially,50 codes were analyzed during Phase 1.We could have developed 50 items and reduced them using a factor analysis technique.However,since we estimated a small sample size and the burden for MBC patients to complete all questions (including one from EORTC QLQ-C30 and EORTC QLQ-BR23),we decided to optimize the dimensions early on during the qualitative analysis process.
The questions in the MBC-PsySoc-Well-being scale may seem to be generic statements and lack specific key terms in the context of MBC patients.It is important to note that all statements were constructed heavily based on terms and phrases used by focus group informants who were MBC patients and their caregivers and healthcare professionals.Therefore,the specific context of MBC was omitted in the question statements.Besides,the context of MBC patients is generally complicated and varied depending on the physical health status,treatments,and prognosis.Thus,the statements were designed to be applicable to MBC patients across various contexts.The application of MBC-PsySoc-Well-being scale outside MBC context should be extremely cautious.
Since the number of participants in this study is small,this would undeniably yield an underpowered effect [67].This limitation impacts the implication of factor analysis.Nevertheless,in certain medical research areas,it is commonly difficult to collect a large sample of patients suffering from a certain disease[68].This is a major limitation of this study.Recruiting MBC patients who met all recruitment criteria in an outpatient clinic was a challenging process.A number of MBC patients were not physically ready to participate in the study.In addition,MBC patients were very vulnerable subjects.It took quite some time for them to process information about the study and make decisions.Therefore,we decided to use a practical number of participants.A larger-scale multi-center study is needed to improve the instrument in the future.
4.4.Future directions for research and practice
The predictive validity test using confirmatory factor analysis was not included in this study.Performing such a test requires a new data set and a larger sample size which is impractical in the context of this study.It is recommended that future study should include the evaluation of predictive validity using confirmatory factory analysis with a large sample size.
In addition,the questions in this study were developed and tested in Thai version only.English-translated version has not been assessed for validity and reliability.The validity and reliability tests of the questionnaire in other languages should be conducted prior to the adoption.
Three constructs emerged and were tested for internal consistency.While these constructs are applicable to assess the psychosocial domains of MBC patients’ well-being,these constructs can also be utilized by healthcare professionals and psychology experts to improve the quality of life of MBC patients.There are several factors contributing to the psychosocial wellbeing of MBC patients such as physical,economic,social,mental,emotional,cultural,and spiritual determinants of health etc.Indeed,an in-depth measurement specific to these factors may be helpful.Nevertheless,developing these specific instruments still need further investigation.Moreover,it is certainly useful to develop a short questionnaire for MBC patients that focuses on psychosocial well-being dimensions.
5.Conclusion
Here we describe an initiative to develop a rapid psychosocial well-being screening tool for patients with MBC,covering affection,cognition,and behavior dimensions.A qualitative approach compiling results from content analysis of relevant literature and a focus group method was applied to develop an operational framework (i.e.,psychosocial dimensions) and initial themes.An eight-question scale was developed and the results from validity and reliability testing indicate that the scale is moderately suitable for application to patients with metastatic breast cancer.This may be due to the low number of participants who were MBC patients.The developed screening tool (MBC-PsySoc-Well-being) can be reasonably applicable to MBC patients with caution,although additional improvements including validity and reliability testing should be further conducted.
Funding
This study was financially supported by the 90th anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund)and partially supported by the Behavioral Research and Informatics in Social Science Research Unit,Chulalongkorn University,Thailand.
CRediT authorship contribution statement
Bhumipat Thanasansomboon:Conceptualization,Methodology,Investigation,Writing -original draft.Songphan Choemprayong:Conceptualization,Methodology,Investigation,Writingreview &editing,Supervision.Napa Parinyanitikul:Conceptualization,Methodology,Resources,Writing -review &editing,Supervision.Uthai Tanlamai:Methodology,Investigation,Writing -review &editing,Supervision.Manika Wisessathorn:Methodology,Investigation,Supervision.Yupin Patarapongsant:Resources,Supervision.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
None of the authors has any conflict of interest with this study.
Acknowledgments
This study could not be completed without a tremendous cooperation and support from all participants.We also would like to thank Tirayut Vilaivant,Praima Israsena Na Ayudhya,Tada Sueblinvong for their valuable feedback and guidance,Pattama Angspatt and Chalita Lagampan for their assistance during the recruitment process,as well as Nozomi Yamada,Papatsara Arsa,and Karuna Yampray for their assistance in the data analysis process.We also would like to express our deep gradtitude to anonymous reviewers for their insightful and constructive recommendations.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.06.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of white noise on procedural pain-related cortical response and pain score in neonates:A randomized controlled trial
- Preventive strategies for feeding intolerance among patients withsevere traumatic brain injury:A cross-sectional survey
- Effects of multidisciplinary exercise management on patients after percutaneous coronary intervention:A randomized controlled study
- Implementation strategies to improve evidence-based practice for post-stroke dysphagia identification and management:A before-andafter study
- The relationship between acceptance of illness and quality of life among men who have sex with men living with human immunodeficiency virus:A cross-sectional study
- Implementation and evaluation of the peer-training program for village health volunteers to improve chronic disease management among older adults in rural Thailand
