Effectiveness and safety of red yeast rice predominated by monacolin K β-hydroxy acid form for hyperlipidemia treatment and management
2022-07-28CHENBenjianHUANGXiaodanPENGHuitingLIYishiCAOYongtaoWUHuanlinXUDanping
CHEN Benjian,HUANG Xiaodan,PENG Huiting,LI Yishi,CAO Yongtao,WU Huanlin,XU Danping
CHEN Benjian,Department of Medical,Guangdong Provincial Hospital of Chinese Medicine,The Second Affiliated Hospital of Guangzhou University of Chinese Medicine,Guangzhou 510120,China
HUANG Xiaodan,the Second Clinical College,Guangzhou University of Chinese Medicine,Guangzhou 510405,China
PENG Huiting,LI Yishi,the First Clinical College,Guangzhou University of Chinese Medicine,Guangzhou 510405,China
CAO Yongtao,Department of Mathematical &Computer Sciences,Indiana University of Pennsylvania,Indiana 15705,PA,USA
WU Huanlin,Department of Cardiology,Dongzhimen Hospital,Beijing University of Chinese Medicine,Beijing 350122,China
XU Danping,Department of Traditional Chinese Medicine,the Eighth Affiliated Hospital,SunYat-Sen University,Shenzhen 518033,China
Abstract OBJECTIVE:To assess the lipid-lowering activity and safety of a dietary supplement containing monacolin K βhydroxy acid form (MKA),Heye (Folium Nelumbinis),and Cangzhu (Rhizoma Atractylodis Lanceae),compared to lifestyle modifications.METHODS:Totally 117 subjects with moderate to severe dyslipidemia (according to Chinese guidelines) and low CV risk were randomly assigned into three treatment groups:lifestyle modification (LM),LM plus a low dosage of MKA,LM plus a high dosage of MKA,and treated for 60 d.The primary endpoint was the reduction of low density lipoprotein cholesterol (LDL-C) and total cholesterol (TC).Safeties along with Traditional Chinese Medicine Syndromes were assessed through the study.RESULTS:A low dosage of MKA along with lifestylemodifications caused a significant decrease in LDL-C by 15.6% on average (95% CI,9.6% to 21%) with,a decrease in TC by 15.3% on average (95% CI,9.26% to 21.4%),and a decrease in non-HDL-C by 35.4% (95% CI,25.76% to 41.34%).Weak evidence of a reduction of triglycerides but an increment of HDL-C was observed in patients with severe hyperlipidemia.No severe adverse events occurred during the study.CONCLUSION:Our results confirm the LDL-C and TC lowering properties of MKA is clinically meaningful.It also produces a significant reduction of non-HDL-C,and slightly effects on TG and HDL-C as well.
Keywords: hydroxy acids; lovastatin; hyperlipidemias;cholesterol;cardiovascular prevention;lifestyle modifications;red yeast rice
1.INTRODUCTION
Within the last few decades,red yeast rice (RYR) has been widely used as a natural remedy to lower serum cholesterol levels,promote heart health,and with the hope to reduce statin-associated adverse side effects.It has been noted however that the effectiveness at reducing blood cholesterol is mainly due to its high level of monacolin K in lactone form (MKL),which is identical to lovastatin.Therefore,the MKL rich RYR (RYR-MKL)shares the same statin-associated adverse side effects.Due to the safety concerns,RYR products that contain a specific amount of MKL are prohibited in USA and Canada.1The European Food Safety Authority (EFSA)approved a health claim regarding the consumption of RYR as a food supplement containing MK (10 mg) for maintaining normal blood LDL-C concentrations.2
It has been found that MK exists in two forms,MKL and monacolin K β-hydroxy acid form (MKA) forms.3Further study has found that the MKL is inactive,and its lipid-lowering effects depend on its conversion into an active MKA form.3But this process requires the consumption of carboxylases,which may cause liver and kidney damage.MKA,on the other hand,does not undergo liver enzyme metabolism and directly binds to HMG-CoA reductase without increasing the burden on the liver.Therefore,MKA is considered to be safer than statins.Unfortunately,according to Mornaret al,4in most tested RYR samples,MKL predominates over the MKA.More specifically,the recent scientific opinion from EFSA reports that the MKL form represents approximately 85% of the total MK content,and the MKA form only represents approximately 15%.2
In order to improve the safety of RYR supplements,and to retain their effectiveness at managing blood cholesterol,we developed a tea drink containing RYR that is enriched with MKA (RYR-MKA).The aim of this study was to assess the lipid-lowering activity and safety of the proposed formulation in patients with moderate to severe hyperlipidemia,compared to simple lifestyle modifications.
2.MATERIALS AND METHODS
Trial registration:Chinese Clinical Trial Registry ID:ChiCTR1800016578.
2.1.Composition of the tea product
A single tea bag contains 3 g of Hongqu (Utivarietas Oryzae Sativae et Monasci),also called RYR,predominated by the RYR-MKA in form of micropowder,5 g of Heye (Folium Nelumbinis) powder,and 2 g of Cangzhu (Rhizoma Atractylodis Lanceae)powder. The RYR-MKA (patent number:ZL200910095494.5) was purchased from Tongjuntan®(Hangzhou,Zhejiang,China).The total MK content is 4 mg/g,with more than 90% represented by MKA.5Heye(FoliumNelumbinis) and Cangzhu (Rhizoma Atractylodis Lanceae) are both natural herbs.The former was found to have anti-obesity,antioxidant,hypoglycemic,and hypolipidemic effects,6while the latter is well known for anti-inflammatory and antiobesity effects.7
2.2.Patients selection
Between May 2017 and May 2018 eligible patients were recruited from outpatients of the Second Affiliated Hospital of Guangzhou University of Chinese Medicine.Inclusion criteria were:(a) ages 18 to 80,(b) ability to provide informed written consent,and (c) LDL-C >3.4 mmol/L and <4.9 mmol/L,or TC >5.2 mmol/L and<7.2 mmol/L,and without ASCVD based upon Chinese guidelines on adults with dyslipidaemia.8 Exclusion criteria were:pregnancy or breast feeding;history of family hyperlipidemia;endogenous creatinine clearance rate <60 mL/min/1.73 m2;impaired liver function;secondary hyperlipidemia caused by specific drugs or other diseases;accompanied by heart failure,cardiac function >NYHA Ⅲ;history of severe arrhythmia;suffered from acute myocardial infarction,cerebrovascular accident or PCI,etc.;needed to take lipid-lowering drugs for a long time;uncontrolled 3rd stage hypertension;fasting blood glucose >15 mmol/L;use of Heparin,Thyroxine and other drugs affecting blood lipid metabolism in the past two weeks;history of mental disorder,alcohol or drug dependence;malignancy or related history;history of serious adverse reactions or allergies to statins;severe gastrointestinal diseases requiring current treatment;severe hypoxic lung disease;participation in other clinical trials within the last 3 months.This study has been approved by the ethics committee and patients have signed informed consent.
2.3.Study design
The study was conducted at the Second Affiliated Hospital of Guangzhou University of Chinese Medicine(including 4 clinical centers) according to a controlled,randomized,double-blind,and repeated measures design.During the screening visit,study physicians assessed the patients’ eligibility and widely discussed CV primary prevention and the importance of lifestyle changes concerning smoking and drinking,physical activity and a healthy diet based on the Chinese Guidelines for Prevention and Treatment of Adults with Dyslipidemia(2016) Revised Edition.After evaluation,the eligible patients were randomly divided into three groups:LM group,i.e.,the control group;LM+a low-dose RYRMKA group (MKA-low);and LM+high-dose RYRMKA group (MKA-high).All study participants received education on the lifestyle modifications including basic prevention and treatment knowledge of dyslipidemia,smoking cessation,alcohol restriction,diet,and weight control.Also,exercise and psychological guidance were offered,focusing on appropriate physical activity (30 min/d),aerobic exercise more than 3 times a week and the importance of good psychology for health.In addition to education about lifestyle modifications,patients in MKA-low group consumed one tea bag/d and patients in the MKA-high group consumed two tea bags/d.Participants were instructed to brew the tea bag(s)in 250-300 mL boiling water for 15 minutes before consume.
On the (31 ± 3) day,participants returned for clinical evaluation and recording any adverse events in detail.Compliance was assessed by asking participants about their adherence with prescribed lifestyle modifications,and whether or not they were preparing and consuming the tea as instructed.Drug compliance was calculated as=(dosage-not used)/ applied dose × 100%.
On the (61 ± 1) day,the end of study visit was performed.Participants returned for blood collection and were once again asked about adherence with prescribed lifestyle modifications,compliance with tea consumption,and any adverse effects.
2.4.Outcome
The primary outcomes were changes in low-density lipoprotein cholesterol (LDL-C),total cholesterol (TC),triglycerides,and high-density lipoprotein cholesterol(HDL-C).As changes in non-HDL-C,apolipoprotein-A1(Apo-A1),apolipoprotein-B (Apo-B),and lipoprotein (a)[LP (a)] were the secondary outcome measures.Safety outcomes include 60 d change in liver function including alanine transaminase (ALT),aspartate transaminase(AST),renal function including blood urea nitrogen(BUN),serum creatinine (Scr),uric acid (UA),blood routine,urine routine,stool routine.In addition,the incidence and severity of adverse events were also recorded.As for the TCM syndrome measures,we assessed if participants experienced any dizziness,chest distress,head heavy,fatigue,heavy limbs,vomiting/phlegm,bloating,taste changes,syrigmus,reduced appetite,ventosity,lower limb edema,and loose stools based on the Guiding Principles for Clinical Research of New Drugs in Traditional Chinese Medicine (Trial).9The scores were then converted to yes vs.no according to Albertiet al.10
2.5.Statistical analysis
All statistical analysis were performed using the R statistical package,version 3.5.3 (R Core Team,2019).Standard descriptive analysis was performed to summarize the study charac-teristics of the patients at entry.All values are expressed as mean ± standard deviation or as percentages ± standard error.Baseline characteristics in the three groups were compared using one-way analysis of variance or χ2 test of independence as appropriate.Changes in outcome measures from baseline within each group were assessed using paired ttest or McNemar exact test.11Repeated measures modeling,i.e.,linear mixed model for quantitative measures and generalized linear mixed model with Binomial assumption for qualitative measures,was also performed to evaluate and compare treatment effects on these parameters.The mixed models were fitted with R package “lme4”,andP-values from the fitted mixed models were obtained by using the R package “afex”.Tukey adjusted pairwise comparisons from the fitted mixed models were performed with the R package“emmeans”.The minimum level of statistical significance was set toP <0.05two-sided,therefore 95%confidence intervals (95%CIs) were calculated.
3.RESULTS
3.1.Patient characteristics at entry
From May 2017 to May 2018,138 subjects were screened,of which 117 subjects met eligibility criteria were randomized to receive LM(n=39),LM+MKAlow (n=37) or LM+MKA-high (n=41).Of these,6 patients (four in the LM+MKA-high group and two in the LM+MKA-low group) withdrew from the study.The remaining 111 patients who completed the study were included in the analysis (Figure 1).
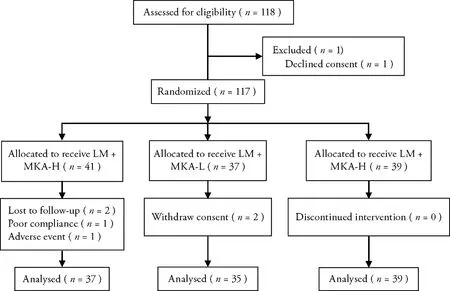
Figure 1 CONSORT diagram depicting flow of the patients through the trial
Table 1 shows the main characteristics of study population at baseline.There are no differences among the three groups in terms of demographics.Lipid profiles of the three groups were also very similar,with triglycerides as the only exception.Triglycerides level in the LM+MKA-high group is significantly higher than that of the other two groups (P=0.035).In terms of the safety parameters,AST,CK,LDH,RBC and HB are all different among the three groups.Regarding the 13 TCM syndromes,only vomiting and reduced appetite were significantly different among the three groups.Most of these aforementioned differences are disappeared after the 60-day treatment,but differences in HB and vomiting were still reported.
3.2.Efficacy
The effect of treatment on both the primary and secondary lipid profiles are reported in Table 2.After 60 d,LDL-C decreased by 15.5% on average (P <0.001)during treatment with LM+MKA-high,by 15.6% on average during treatment with LM+MKA-low(P <0.001),and by 1.9% on average (P <0.53) during treatment with only LM.However,we did not observe a significant difference between the MKA-high and MKA-low groups.
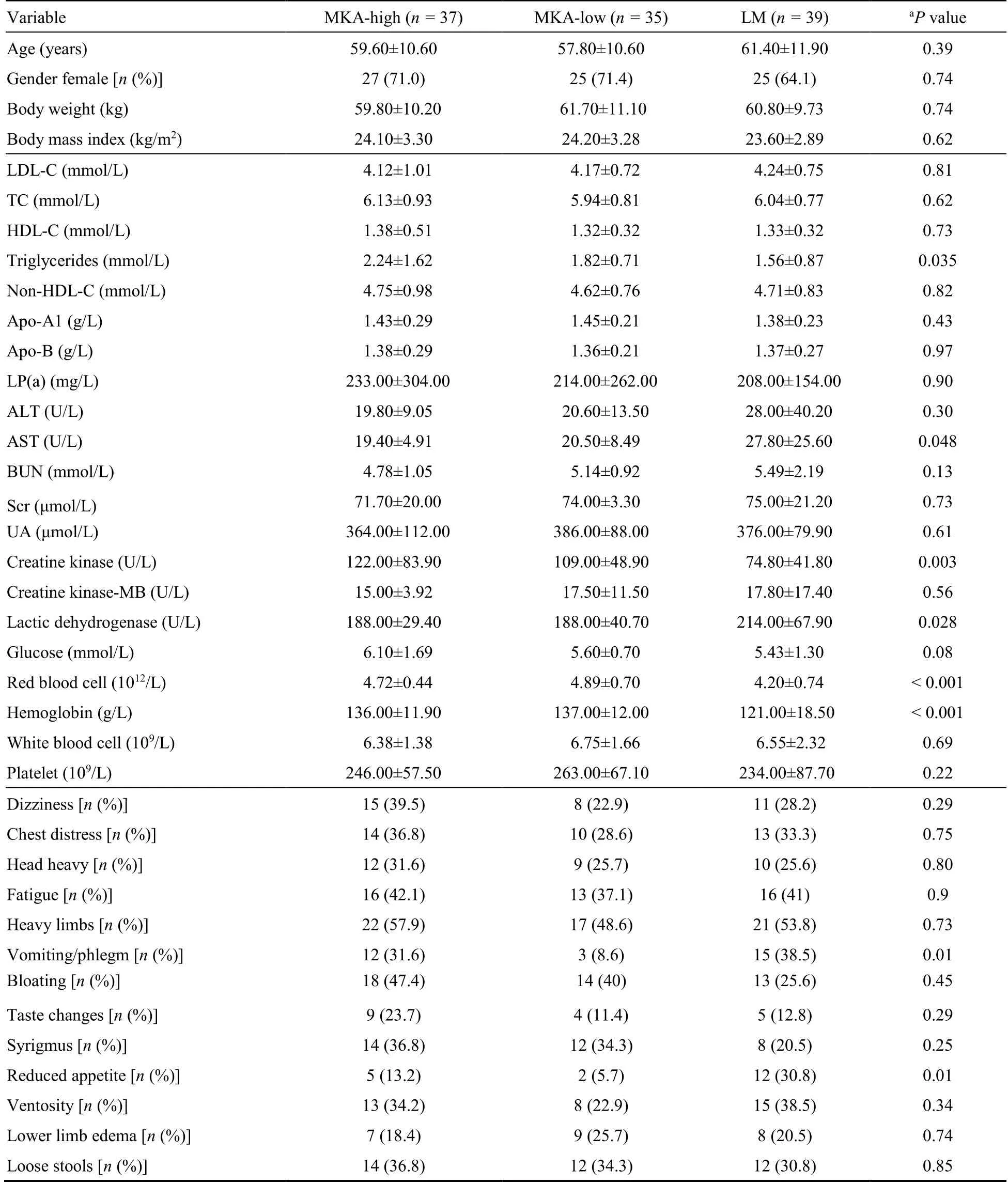
Table 1 Baseline characteristics and lipid profile of the study populations
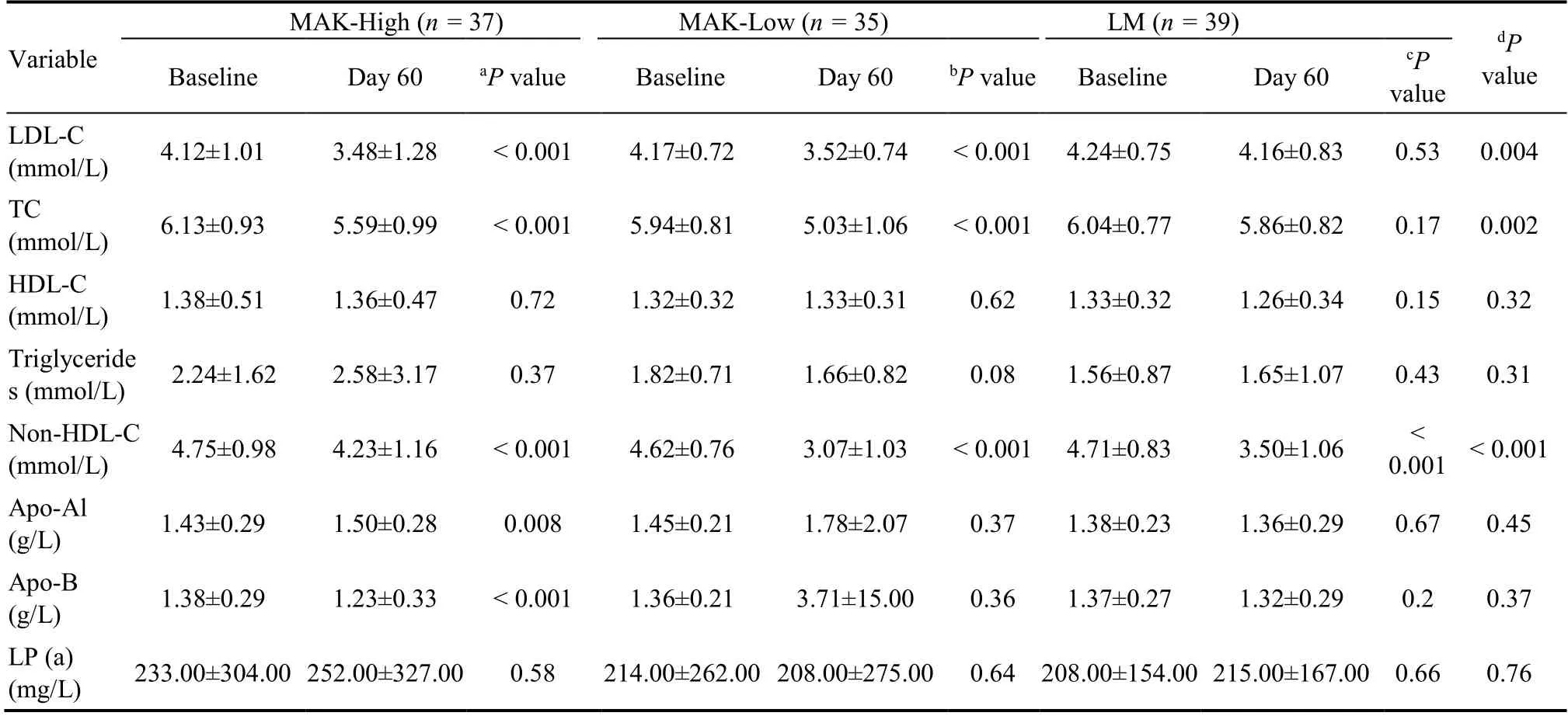
Table 2 Lipid profile before and after the treatment
The MKA-high — MKA-low difference,i.e.the mean difference between the within-period changes observed with MKA-high and MKA-low,was-0.1% (the minus sign meaning a greater reduction during treatment with MKA-low compared to MKA-high).The 95%CIof this was between-2.3% and+2.5%,entirely within the interval of- 10% to+10% defined as clinicalequivalence and used in sample size calculation.A Tukey adjusted multiple comparison of the LDL-C reductions within each treatment,as absolute values,is visualized in Figure 2a.Numerically,the mean absolute LM — MKA-high difference was 0.68 mmol/L (95%CI,0.187 to 1.17);the mean absolute LM — MKA-low difference was 0.64 mmol/L (95%CI,0.142 to 1.14);and MKA-high —MKA-low difference was -0.037 mmol/L(95%CI,-0.544 to 0.47).
TC also decreased significantly within both the MKAhigh and MKA-low groups(P <0.001),while the between-treatment comparison showed a different pattern (Figure 2b).Firstly,the MKA-low has the highest reduction in TC (15.3%,P <0.001),and there was a significant difference in the reduction of TC between MKA-low and MKA-high (-0.557,95%CI,-1.06 to-0.057).Secondly,there was no difference between the LM and MKA-high (95%CI,-0.21 to 0.77).
Among the 4 secondary outcomes,a significant reduction in Non-HDL-C was observed in all the three treatment groups.Specifically,non-HDL-C decreased by 35.4% on average within the MKA-low group,25.7% on average in the LM group,and only 10.9% on average in the MKA-high group.Though the mean absolute LM —MKA-low difference in Non-HDL-C was 0.43 mmol/L(95%CI,-0.11 to 0.97) (Figure 3a),the difference tends to be significant as the lower limit of theCIis very close to 0.The mean absolute MKA-high — MKA-low difference in non-HDL-C is significantly different from 0,suggesting that a low dosage of MKA is better than a high dosage.Though a reduction in both of Apo-A1 and Apo-B was observed within the MKA-High group,the between-treatment comparisons,as seen from Figure 3b and 3c,showed slightly non-significant results.
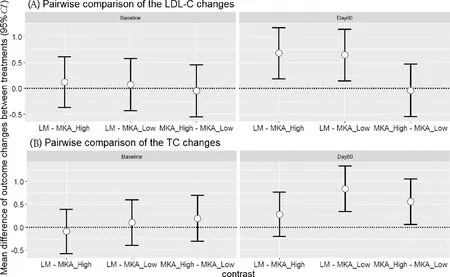
Figure 2 Tukey pairwise comparison of (A) the LDL-C changes,and (B) TC changes
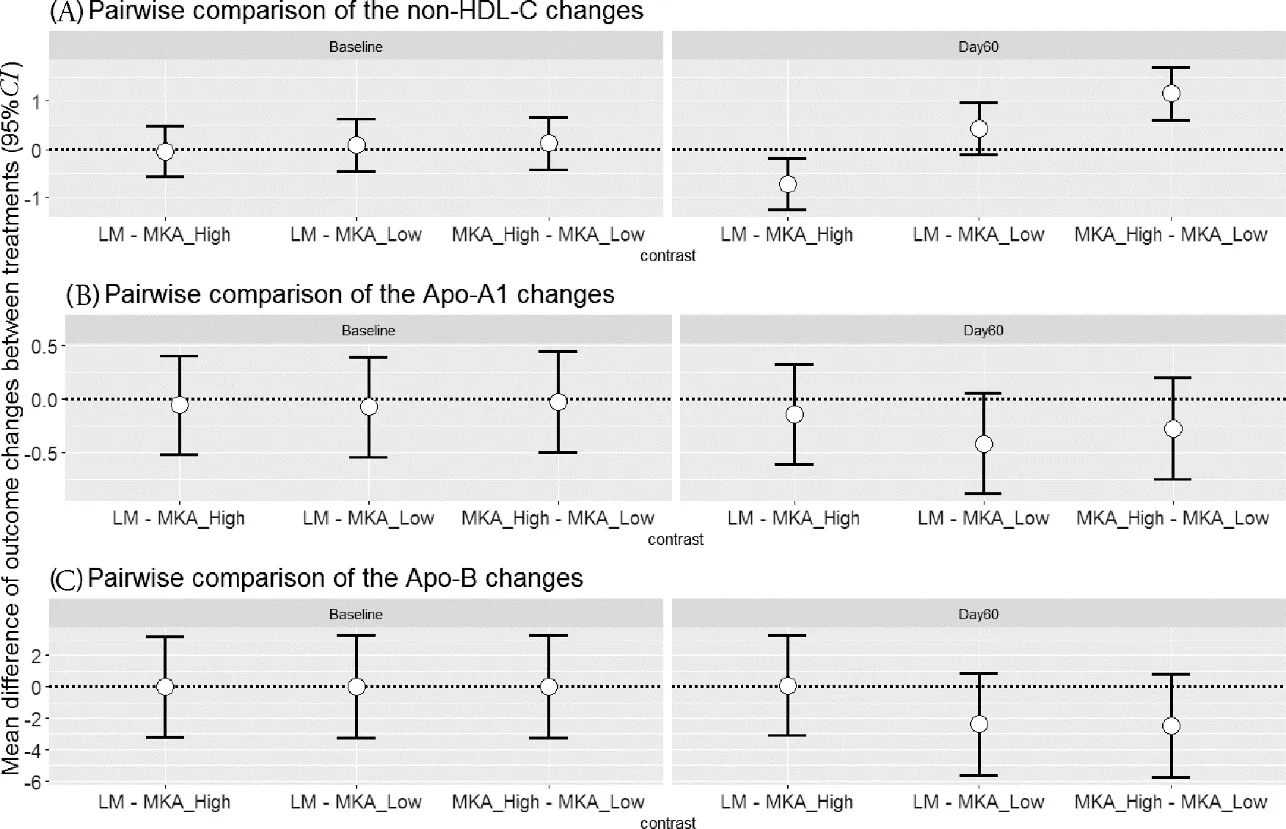
Figure 3 Tukey pairwise comparison of (A) the non-HDL-C changes,(B) Apo-A1 changes,and (C) Apo-B changes
Since we did not see a difference between a low dosage of MKA (1 tea bag/d) and a high dosage of MKA (2 tea bags/d) in terms of both the primary and secondary outcomes,we next investigated how a low dosage of MKA works for different subgroups of patients.Based on the Chinese guidelines for prevention and treatment of adults with dyslipidemia (2016 edition),we divided the patients in the MKA-low group,according to their baseline outcomes,into groups with high LDL-C (>4.1 mmol/L),high TC (>6.2 mmol/L),high TG (>2.3 mmol/L),high non-HDL-C (>4.9 mmol/L),and low HDL-C (<1 mmol/L) as well as the corresponding nonhigh (non-low) groups.As shown in Table 3,when their baseline levels are high in LDL-C and non-HDL-C,patients experienced a higher reduction in the two than that in the non-high groups after 60 d.Though not highly statistically significant,TG tended to decrease and HDLC tended to increase for patients with high TG and low HDL-C levels,respectively.
3.3.Safety
No severe adverse events occurred during the study;no event required treatment interruption or remedial therapy.Moreover,there were no clinical changes in any of the safety parameters during the course of the study.
3.4.TCM Syndromes
Regarding the 13 TCM syndromes we investigated(Table 4),no changes were found for chest distress,heavy head,fatigue,bloating,syrigmus,reduced appetite,and ventosity.It was detected that a low dosage of MKA can reduce dizziness (by 20% on average) and loose stools (by 25.7% on average);lifestyle modifications can reduce heavy limbs (by 17.9% on average) and lower limb edema (by 12.8%).The only side effects with in MKA-low group were the syndromes of vomiting/phlegm and taste changes increased by 25.7% and 31.5%,respectively.These two phenomena,however,were not observed in MKA-high group.
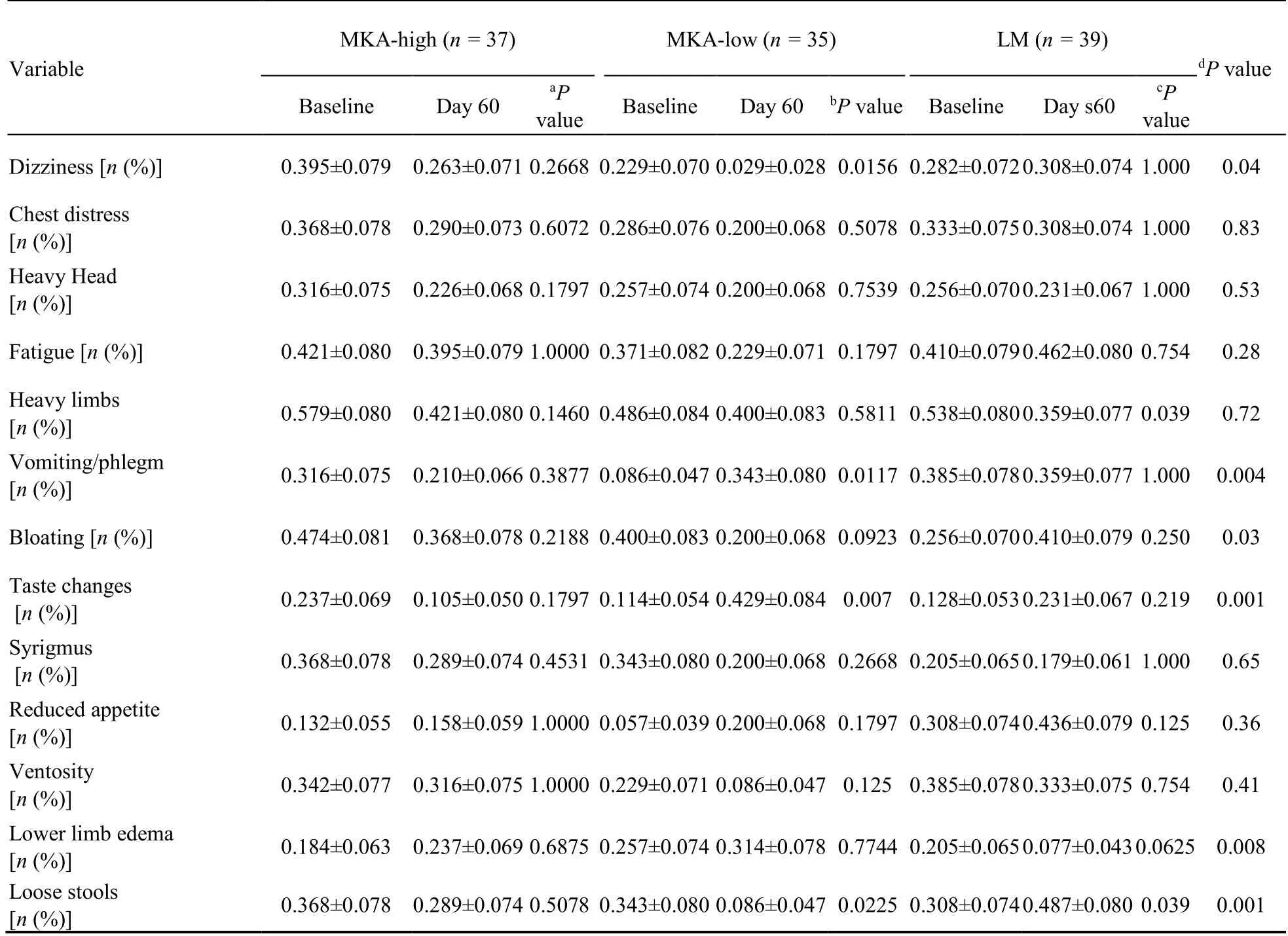
Table 4 TCM Syndrome before and after the treatment
4.DISCUSSION
Red yeast rice,as a nature provided lovastatin,is currently one of the most commonly used lipid-lowering dietary supplements.But the safety,especially the long-term safety of using RYR supplements remains unclear.It should be emphasized that it is the MKL rather than the MKA in RYR that causes safety concerns.However,MKA has been rarely clinically studied.2Unlike other works on limiting the daily dosage of using RYR,1,2,12we herein highlight the benefits of using a RYR that is predominated by MKA for hyperlipidemia treatment and management.To the best of our knowledge,this is the first comprehensive study on the dosage,effectiveness,safety,as well as TCM syndromes of using RYR-MKA for treating moderate to severe hyperlipidemia.Our results were in agreement with previous research on MKA5and showed a statistically significant reduction of both LDL-C and TC levels.Moreover,we showed that the effectiveness of MKA is more promising than MKL.13We were able to document a marked dosage of using MKA as a dietary supplement,that is,a daily dosage of 10.8 mg (one tea bag) can result in a promising hyperlipidemia treatment effect.
It should also be noted that,unlike many other clinical studies,we did not give a placebo to the patients in the control group.Rather,we prescribed enhanced lifestyle modifications (compared to the lifestyle modification activities given in the most recent Chinese guidelines on dyslipidemia) as we believe everyone can benefit from preventative lifestyle strategies to manage their heart health.Instead of simply employing lifestyle modifications,another possible way to set up the control group is to give patients RYR that is totally free of MK as a recent study demonstrated that a 110 mg/d of Ankascin 568-R can result in a 20% reduction of LDL-C after 8 weeks.14
Although in line with other studies,one limitation of the present study is the short study period.13A 60-day,or about 8-week study period may not be adequate to evaluate the long-term efficacy of MKA.However,a 3-month study5showed that MKA indeed can significantly reduce TG and improve HDL-C.
In conclusion,our results confirm the clinically meaningful lipid-lowering properties of monacolin K βhydroxy acid form and the efficacy of a novel association of it with lotus leaf and rhizoma atractylodis.Furthermore,use of RYR predominated by monacolin K βhydroxy acid form was not associated with reports of adverse events.In addition to the very effective LDL-C and TC lowering capacity,it is worth noting that reduction of triglycerides and increment of HDL-C as well may be achieved by patients with severe hyperlipidemia.
杂志排行
Journal of Traditional Chinese Medicine的其它文章
- Mechanisms of immune regulation for acupuncture on chronic respiratory diseases
- Mechanism of Huashi Xingyu Qingre recipe (化湿行淤清热方) in treating oral lichen planus based on network pharmacology and clinical trial verification
- Anti-inflammatory mechanism of rhein in treating asthma based on network pharmacology
- An international multicentric phase Ⅲ randomized controlled trial of time-acupoints-space acupuncture for the prevention of chemotherapy-induced fatigue in patients with early stage breast cancer:a study protocol
- Mining intrinsic information of convalescent patients after suffering coronavirus disease 2019 in Wuhan
- Menstrual cycle characteristics as an indicator of fertility outcomes:evidence from prospective birth cohort study in China
