维持性血液透析患者NLR与心血管疾病关系分析
2022-07-18丁忻史秀岩张庆红
丁忻 史秀岩 张庆红

[摘要] 目的 探究維持性血液透析患者的中性粒细胞/淋巴细胞比值(NLR)与心血管疾病的关系。方法 回顾性分析2018年9月~2021年8月于湖北省十堰市太和医院接受治疗的维持性血液透析患者的诊疗情况,选取193例作为维持性血液透析组,并选择同期接受体检的健康志愿者60名作为对照组。根据患者情况将维持性血液透析组分为心血管疾病组及非心血管疾病组。比较各组的性别、年龄、血钙(Ca)、血磷(P)、血红蛋白(Hb)、白蛋白(Alb)、高敏C-反应蛋白(hs-CRP)、中性粒细胞数量、淋巴细胞数量及NLR,分析其对维持性血液透析患者合并心血管疾病的影响。结果 维持性血液透析组的Ca、Hb、Alb、淋巴细胞数量均低于对照组,P、hs-CRP、中性粒细胞数量、NLR均高于对照组,差异有统计学意义(均P<0.05)。心血管疾病组的年龄、Ca、P、hs-CRP、中性粒细胞数量、NLR均高于非心血管疾病组,Hb、Alb、淋巴细胞数量均低于非心血管疾病组,差异有统计学意义(均P<0.05)。经Logistic回归分析发现,年龄、Hb、Alb及NLR均是影响维持性血液透析患者合并心血管疾病的危险因素(均P<0.05)。结论 维持性血液透析患者的NLR呈升高状态,是影响心血管疾病发生的独立危险因素。
[关键词] 维持性血液透析;心血管疾病;中性粒细胞/淋巴细胞比值;独立危险因素
[中图分类号] R692.5;R459.5 [文献标识码] A [文章编号] 1673-9701(2022)17-0011-04
Analysis on the relationship between NLR and cardiovascular disease in patients undergoing maintenance hemodialysis
DING Xin1,2 SHI Xiuyan2 ZHANG Qinghong2
1. Postgraduate Training Base of Jinzhou Medical University, Taihe Hospital of Shiyan in Hubei Province, Shiyan 442000, China; 2. Department of Nephrology, Taihe Hospital of Shiyan in Hubei Province, Affiliated Hospital of Hubei University of Medicine, Shiyan 442000, China
[Abstract] Objective To explore the relationship between the neutrophil to lymphocyte ratio (NLR) and cardiovascular disease in patients undergoing maintenance hemodialysis. Methods The diagnosis and treatment conditions of the patients undergoing maintenance hemodialysis in Taihe Hospital in Shiyan in Hubei Province from September 2018 to August 2021 were retrospectively analyzed. A total of 193 patients were selected as the maintenance hemodialysis group, and 60 healthy volunteers who underwent physical examination in the same period were selected as the control group. According to the conditions of patients, the maintenance hemodialysis group was subdivided into the cardiovascular disease group and the non-cardiovascular disease group. Gender, age, blood calcium (Ca), blood phosphorus (P), hemoglobin (Hb), albumin (Alb), high-sensitivity C-reactive protein (hs-CRP), neutrophil count, lymphocyte count and NLR were compared among the groups. Its effects on cardiovascular disease in patients undergoing maintenance hemodialysis were analyzed. Results The levels of Ca, Hb and Alb and lymphocyte count in the maintenance hemodialysis group were lower than those in the control group, and the levels of P and hs-CRP, neutrophil count and NLR were higher than those in the control group, with statistically significant differences (all P<0.05). The age, the levels of Ca, P and hs-CRP, neutrophil count and NLR in the cardiovascular disease group were higher than those in the non-cardiovascular disease group, and the levels of Hb and Alb and lymphocyte count were lower than those in the non-cardiovascular disease group, with statistically significant differences (all P<0.05). Logistic regression analysis showed that age, Hb, Alb and NLR were the risk factors for cardiovascular disease in patients undergoing maintenance hemodialysis (all P<0.05). Conclusion NLR in patients undergoing maintenance hemodialysis is elevated and is an independent risk factor for cardiovascular disease.
[Key words] Maintenance hemodialysis; Cardiovascular disease; Neutrophil to lymphocyte ratio; Independent risk factors
目前全球范围内慢性肾脏病(chronic kidney disease,CKD)患病率逐年升高,其中终末期肾脏病(end stage renal disease,ESRD)及透析患者人数以20%~30%比例增长。虽然血液净化技术不断提高,但患者病死率仍较高[1],研究表明维持性血液净化(maintenance hemodialysis,MHD)患者的心血管疾病(cardiovascular disease,CVD)病死率较同年龄和性别匹配的健康个体相比高出9倍,且CVD可在一定程度上促进肾脏疾病的进展,更易进入终末期肾病。因此积极掌握影响MHD患者合并CVD的因素对其生存率的提高有着不可或缺的意义。外周血中性粒细胞/淋巴细胞比值(NLR)是近年来新提出的反映机体炎症状态的指标,在CVD中可提示炎症,且可提前评估MHD患者的生存率[2,3]。因此,本研究通过观察MHD患者的NLR水平变化,并分析其与合并CVD的关系,现报道如下。
1 资料与方法
1.1 一般资料
选取2018年9月~2021年8月湖北省十堰市太和医院收治的MHD患者193例,其中男105例,女88例;原发病:慢性肾小球肾病99例,糖尿病肾病67例,高血压肾病24例,多囊肾3例。另選取同期接受体检的健康志愿者60名作对照组。纳入标准:①明确诊断并接受维持性血液透析治疗的ESRD患者;②每周透析3次,每次至少4 h,维持透析3个月以上;③年龄>18岁;④临床资料完整,同意参加研究。排除标准:①合并恶性肿瘤、结核等消耗性疾病者;②服用免疫抑制剂、激素等治疗者;③近期出现感染、接受手术或输血的患者。心血管疾病的诊断标准:根据欧洲心脏协会(ESC)诊断为急性及陈旧性心肌梗死、不稳定心绞痛、心源性猝死、需入院治疗的心力衰竭。MHD患者合并心血管疾病的排除标准:原发性高血压引起心肌梗死、心绞痛、心衰;先天性心脏病、肥厚梗阻性心脏病、感染性心内膜炎、心肌炎或风心病、主动脉夹层、心律失常等;慢性肾脏病发生前出现的心血管疾病。本研究经湖北省十堰市太和医院医学伦理委员会批准[批件号:(2022KS008)号]。
1.2方法
采集对照组晨起空腹外周静脉血,维持性血液透析组在透析前采集空腹静脉血。采用全自动血液分析仪检测Ca、P、Hb、Alb、中性粒细胞数量、淋巴细胞数量,同时采用日立7600生化分析仪检测hs-CRP。计算出NLR值。并根据患者情况将维持性血液透析组分为心血管疾病组及非心血管疾病组。检测并比较两组以上各指标的差异。
1.3 统计学方法
应用SPSS 22.0统计软件进行数据分析,计量资料以均数±标准差(x±s)表示,组间比较采用t检验,计数资料以[n(%)]表示,组间比较采用χ2检验,采用Logistic回归分析影响血液透析患者合并心血管疾病的相关因素,P<0.05为差异有统计学意义。
2 结果
2.1 两组受试者临床指标比较
两组的性别、年龄比较,差异无统计学意义(均P>0.05);维持性血液透析组的Ca、Hb、Alb、淋巴细胞数量均低于对照组,P、hs-CRP、中性粒细胞数量、NLR均高于对照组,差异有统计学意义(均P<0.05)。见表1。
2.2 有无合并心血管疾病患者临床指标比较
心血管疾病组的年龄、Ca、P、hs-CRP、中性粒细胞数量、NLR均高于非心血管疾病组,Hb、Alb、淋巴细胞数量均低于非心血管疾病组,差异有统计学意义(均P<0.05)。见表2。
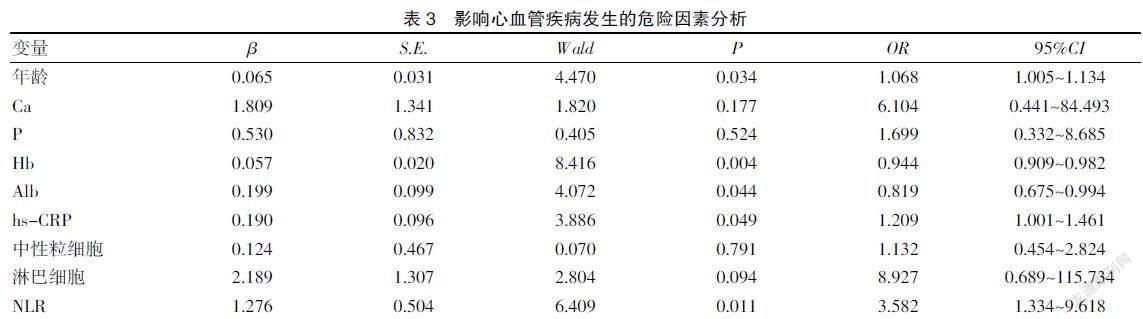
2.3 影响心血管疾病发生的危险因素分析
经Logistic回归分析发现,年龄、Hb、Alb、hs-CRP、NLR均是影响维持性血液透析患者合并心血管疾病发生的危险因素(P<0.05)。见表3。
3 讨论
众所周知,慢性肾脏病患病率逐年升高,已成为全球关注的重要公共卫生问题之一。CKD 的全球患病率估计为13.4%,需要肾脏替代治疗的终末期肾病患者估计在490.2万~708.3万之间,CKD直接影响全球的发病率和病死率[4]。终末期肾病患者存在免疫低下的情况,同时伴有炎症因子的高表达,且维持性血液透析的治疗进一步加重机体炎症反应,而炎症除加重营养不良、贫血等情况外,还容易诱导心血管疾病的发生,从而对患者的生存率及生活质量造成直接影响[5,6]。有研究表明,当前炎症被定义为终末期肾病患者营养不良-炎症-动脉粥样硬化(malnutrition-inflammation-atherosclerosis,MIA)综合征的一部分[7]。与此同时,越来越多的研究证明炎症对心血管疾病的发展和预后的重要性,而心血管疾病又是引起MHD患者不良预后的最主要的原因,炎症因子通过促进低密度脂蛋白胆固醇与血管内皮细胞结合、组织因子释放,进一步导致粥样斑块形成,增加血液透析患者发生心血管疾病的危险性。炎症反应引起的营养不良可降低心肌细胞的体积及心肌纤维的含量[8,9]。而维持性血液透析患者存在明显的NLR表达升高,对其检测可反映患者的系统炎症状态,并作为一种新的炎症标志物,NLR 已被引入心血管疾病中来[10,11]。
本研究结果显示,除年龄、Ca、P、Hb、Alb、hs-CRP是影响维持性血液透析患者合并心血管疾病的危险因素外,NLR也是影响维持性血液透析患者合并心血管疾病发生的危险因素。分析原因如下:①Turkmen等[12]的研究表明NLR可用来预测MHD患者的炎症状况。Guasti等[13]的研究结果显示,NLR是急性冠脉综合征、心力衰竭和冠脉血管重建患者发生心血管不良事件的预测因子。Wan等[14]的研究证明NLR的水平变化与糖尿病患者发生心血管疾病及糖尿病肾病的患病率增加有关。Botu等[15]的研究推测NLR作为炎症标志物可预测MHD患者的心肌不均匀性增厚。②维持性血液透析期间体内的微炎症状态可刺激中性粒细胞凋亡延迟,造成其表达升高,而中性粒细胞的激活可使血液流变学发生改变,增加血管黏附性,并对中性粒细胞功能造成损伤,致使NLR水平升高;且在中性粒细胞被激活的过程中会损伤到血管内皮细胞,从而增加心血管疾病的发生率,最终影响患者的预后[16]。因此,在维持性血液透析期间,除可检测常规的临床指标之外,可进一步结合NLR 水平指导临床的治疗,提前评估心血管疾病发生的可能性,从而预防心血管疾病的发生,提高患者的生存率。
综上所述,NLR作为一种评估炎症的新型指标,拥有廉价便捷、可动态检测的优点;而维持性血液透析患者的NLR处于升高状态,可作为影响维持性血液透析患者合并心血管疾病发生的独立危险因素。
[参考文献]
[1] Johansen KL,Chertow GM,Foley RN,et al. US renal data system 2020 annual data report: Epidemiology of kidney disease in the United States[J].American Journal of Kidney Diseases,2021,77(4):A7-A8.
[2] 邵彩荣,杨小娟.中性粒细胞/淋巴细胞比值,血小板/淋巴细胞比值在慢性肾脏病中的研究进展[J].临床医学进展,2021,11(3):10.
[3] 叶晓梅,张敏,曹含弘,等.中性粒细胞与淋巴细胞比值在糖尿病肾病中的变化及对早期糖尿病肾病的预测价值[J].临床内科杂志,2018,35(9):4.
[4] Lv JC,Zhang LX. Prevalence and disease burden of chronic kidney disease[J].Advances in Experimental Medicine and Biology,2019,53(4):3-15.
[5] 朱愛民,王军升,罗晓燕,等.204例维持性血液透析患者流行病学和病因分析[J].中国当代医药,2011,18(30):160-161.
[6] 李富强.血液透析和腹膜透析对慢性肾衰竭尿毒症患者微炎症状态的影响及与心血管疾病的关系[J].临床内科杂志,2019,36(11):748-750.
[7] Huang Z,Fang J,Song A,et al. The association between self-management ability and malnutrition-inflammation-atherosclerosis syndrome in peritoneal dialysis patients: A cross-sectional study[J].BMC Nephrology,2021,22(1):2-9.
[8] Golia E,Limongelli G,Natale F. Inflammation and cardiovascular disease: From pathogenesis to therapeutic target[J].Current Atherosclerosis Reports,2014,16(9):435.
[9] 高小夏,潘家荣,邹芸,等.腹膜透析患者C反应蛋白水平与营养不良及心血管疾病的相关性[J].中国血液净化,2012,11(11):626-629.
[10] Tamhane UU,Aneja S,Montgomery D,et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome[J].American Journal of Cardiology,2008,102(6):53-57.
[11] Mccluney SJ,Alexandros G,Angela S,et al. Neutrophil: Lymphocyte ratio as a method of predicting complications following hepatic resection for colorectal liver metastasis[J].Journal of Surgical Oncology,2018,117(5):1058-1065.
[12] Turkmen K,Guney I,Yerlikaya FH,et al. The relationship between neutrophil-to-lymphocyte ratio and inflammation in end-stage renal disease patients[J].Renal Failure,2012,34(2):155.
[13] Guasti L,Dentali F,Castiglioni L,et al. Neutrophils and clinical outcomes in patients with acute coronary syndromes and/or cardiac revascularisation. A systematic review on more than 34,000 subjects[J].Thrombosis & Hae-mostasis,2011,105(10):591-599.
[14] Wan H,Wang Y,Fang S,et al. Associations between the neutrophil-to-lymphocyte ratio and diabetic complications in adults with diabetes: A cross-sectional study[J].Journal of Diabetes Research,2020,4(28):1-9.
[15] Botu K,Bociek A,Dziugie R,et al. Neutrophil-lymphocyte ratio (NLR) reflects myocardial inhomogeneities in hemodialyzed patients[J].Mediators of Inflammation,2020, 9(3):1-6.
[16] Efthymios PM,Spiridoula M,Periklis K,et al. The effect of dialysis modality and membrane performance on native immunity in dialysis patients[J].Prilozi,2019,40(2):25-32.
(收稿日期:2021-12-02)
