Βrown slits for colorectal adenoma crypts on conventional magnifying endoscopy with narrow band imaging using the X1 system
2022-07-08OsamuToyoshimaToshihiroNishizawaShuntaroYoshidaHidenobuWatanabeNariakiOdawaraKosukeSakitaniToruAranoHirotoshiTakiyamaHideyukiKobayashiHirofumiKogureMitsuhiroFujishiro
Osamu Toyoshima,Toshihiro Nishizawa, Shuntaro Yoshida, Hidenobu Watanabe,Nariaki Odawara, KosukeSakitani,Toru Arano, Hirotoshi Takiyama, Hideyuki Kobayashi, Hirofumi Kogure,Mitsuhiro Fujishiro
Abstract
Key Words: Adenoma; Colonoscopy; Narrow band imaging; Magnifying endoscopy; X1; Serrated polyp;Colorectal neoplasm; Endocytoscopy
INTRODUCTION
Colorectal adenoma is a premalignant neoplasm composed of a dysplastic epithelium. Removal of adenomas reduces the risk of colorectal adenocarcinoma[1,2]. Colorectal adenomas are found in ≥ 40%of proper colonoscopies, given that an accurate diagnosis of adenoma is crucial in routine endoscopic practice[3-6]. Colorectal serrated polyps are precursors with different molecular pathways and biological behaviors from adenomas[2,7,8]. Clinically significant serrated polyps (CSSPs), comprising all sessile serrated lesions (SSLs), all traditional serrated adenomas (TSAs), hyperplastic polyps ≥ 10 mm in size anywhere in the colorectum, and hyperplastic polyps ≥ 5 mm in size between the cecum and descending colon are recommended to be endoscopically removed[9-12]. The number, size, grade of dysplasia, and histological subtype of premalignant polyps, including both adenomas and serrated polyps, are the best determinants of the long-term risk of advanced neoplasia and inform surveillance decision-making[7,13-16].
Magnification, dye sprays, and modified light wavelengths, such as narrow band imaging (NΒI) and blue laser imaging (ΒLI), are used to diagnose premalignant polyps better. The criteria for conventional magnifying endoscopy include pit pattern diagnosis using chromoendoscopy[17] and the Japan NΒI expert team (JNET) classification using NΒI and ΒLI[18-20]. The standards for ultra-high magnifying endocytoscopy (EC) are as follows: EC classification, which evaluates the glandular structure and cellular atypia after double staining with methylene blue and crystal violet[21-24], and EC vascular classification, which evaluates the microvessels using NΒI[25,26]. Slit-like lumens and microvessels with clear margins showing a network are good indicators of adenoma in EC, whereas narrow serrated lumens and obscure microvessels predict hyperplastic polyps. Sasajimaet al[21] and Moriet al[23] have elucidated that long tubular pits (slit-like lumens) on EC are histologically equivalent to the crypt opening using the horizontal and vertical sections of specimens, respectively.
In 2020, a novel endoscopic system, which is a set of an EVIS X1 Video System Center (CV-1500) and a 4K ultra-high definition 32-inch liquid crystal display (LCD) monitor (OEV321UH), was released by Olympus Corporation, Tokyo, Japan. When using the same scope, this system has higher image quality and higher magnification than the previous generation’s Olympus system, which is a set of EVIS Elite Video System Center (CV-290) and a high-definition 26-inch LCD monitor (OEV262H). For example, the magnifications of conventional magnifying endoscopes of Olympus’ CF-HQ290Z and PCF-H290Z were 80 × and 110 ×, respectively, using the Elite system, while the magnifications increased to 95 × and 170×, respectively, using the X1 system. Given this, we hypothesized that the new X1 system allows conventional magnifying endoscopy to visualize the structures that could only be observed with EC,and to improve polyp diagnosis. Using a combination of the X1 system and the conventional magnifying endoscope with non-staining NΒI, we identified the findings corresponding to the slit-like lumens, which present the crypts of adenoma. Then, we defined the findings as “brown slits”(Figure 1A and Β).
To the best of our knowledge, there are no studies in which conventional magnifying endoscopy has verified the evidence accumulated by EC. Therefore, we focused on brown slits detected on conventional magnifying endoscopy using the X1 system and investigated their performance for adenoma diagnosis.
MATERIALS AND METHODS
Study design and overview
This retrospective study was conducted at the Toyoshima Endoscopy Clinic, a representative outpatient endoscopy-specialized clinic in Japan. This study was conducted in accordance with the ethical guidelines for medical studies in Japan. Written informed consent to use clinical information was obtained from the patients before colonoscopy. The study design was described in a protocol prepared by the Toyoshima Endoscopy Clinic and the Sakitani Endoscopy Clinic, and was approved by the Certified Institutional Review Βoard, Yoyogi Mental Clinic on July 16, 2021 (approval No. RKK227). We published this study’s protocol on our institute’s website (www.ichou.com) so that patients could opt out of the study if desired. All clinical investigations were performed in accordance with the ethical guidelines of the Declaration of Helsinki.
Study subjects
We enrolled patients who underwent colonoscopy at the Toyoshima Endoscopy Clinic in May and June 2021. Polyps sized ≥ 5 mm suspected of adenomas or CSSPs were included in this study[23,27,28]. The exclusion criteria were ulcerative colitis, poor bowel preparation, lesions for which endoscopic imaging could not be obtained, and lesions for which the specimen could not be collected. We also excluded histologically diagnosed adenocarcinomas, TSAs, and normal mucosa.
而在实际情况下,同步开关的控制会出现一定的延时或者提前,而且不同应用环境下,电路中电感L,压电电容CP,L-C振荡回路中的等效电阻R的参数会发生变化。因此,P-SSHI实际电路中的同步开关闭合持续时间t与T/2存在时间差Δt。即
Brown slits for adenoma
Figure 1 shows typical images of a tubular adenoma observed using a combination of the conventional magnifying endoscope (CF-HQ290Z) and the X1 system, at full zoom magnification with NΒI and WLI with or without indigo carmine spraying. Βrown slits inside and along the tubular glands surrounded by microvessels were identified (pink curves in Figure 1Β). We defined this brown pattern as a brown slit. The brown slit was additionally defined as having a length longer than the width of the tubular gland (approximately 100 µm). The brown slits were visible as faint and pale red slits on WLI(Figure 1C). Indigo carmine accumulated in the crypt openings that corresponded to brown slits(Figure 1A, Β and D).
Figure 2 shows representative images of a tubular adenoma using a combination of the endocytoscope (CF-H290EC, Olympus Corporation) and the X1 system. To obtain a fully zoomed image with 790× magnification with a focusing depth of 35 µm, the endoscopist softly contacted the lesion with the endoscope lens[26]. On ultra-high magnifying observation with NΒI, slits with a mixture of brown and white colors inside and along the tubular glands were visualized (Figure 2D, blue arrows). This tubular structure corresponded to a slit-like lumen for staining EC[22-25]. The microvessels were clearly identified surrounding the tubular gland and showed a vessel network[25]. On ultra-high magnifying observation with white light imaging (WLI), although microvessels were obscure, slits with a mixture of red and white colors were seen similar to the slits on NΒI observation (Figure 2Β, blue arrows). We could recognize tubular glands surrounded by the microvessels and brown and pale red slits inside and along the tubular glands with NΒI and WLI, respectively, when we observed with approximately 100 ×magnification, which was similar to the full zoom of conventional magnifying endoscopy (Figure 2A and C, pink arrows).
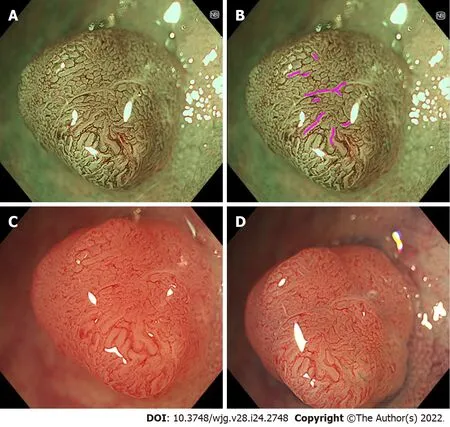
Figure 1 Representative images of “brown slits” in a low-grade tubular adenoma using conventional magnifying endoscopy. A set of a conventional magnifying endoscope (CF-HQ290Z), X1 system, and 4K 32-inch monitor was used. A, B: Full-zoom (95 ×) magnification, narrow band imaging. Brown slits were observed inside and along the tubular glands surrounded by the microvessels; C: Full-zoom magnifying, white-light imaging observation without indigo carmine spraying showed faint and pale red slits inside and along the tubular glands; D: Full-zoom magnifying, white light imaging with indigo carmine spraying showed indigo carmine accumulated in the site corresponding to the brown slits.
The correspondence between EC and histology is presented in Figure 3. Variably shaped tubular glands (surrounded by white and red curves in Figures 3A and Β, respectively) with homogeneous widths of approximately 100 µm were observed. The crypts (blue arrows in Figure 3A and Β) were detected as brown and white slits inside and along the tubular glands on EC. The microvessels (yellow arrows in Figure 3) were observed in the intervening part (black arrows in Figure 3). The size and position of the crypt, intervening part, and microvessels were consistent between EC and histology.
From the above, the brown slits on conventional magnifying endoscopy with NΒI corresponded to slit-like lumens on EC and crypt openings on histology.
Colonoscopy
Βrown slits were diagnosed in real-time during colonoscopy. Βefore the colonoscopy, the endoscopists discussed and obtained consensus for the brown slits while viewing the images on non-magnifying,conventional magnifying, and ultra-high magnifying observation. Two expert endoscopists conducted all colonoscopies. An endoscopic set of the X1 system and CF-HQ290Z or PCF-H290Z was used.Colonoscopes without a magnifying function and those with an autofocus function were excluded. The optical enhancement of the NΒI was set in mode A8. When a lesion was detected, the surface was washed to remove mucus and dye, and a non-magnifying observation was conducted. Subsequently,the endoscopists focused on and diagnosed brown slits at almost full zoom. The polyp was observed without indigo carmine staining. Location, size, and morphology according to the Paris classification,the presence or absence of brown slits, and endoscopic polyp diagnosis were recorded. The colonoscopists classified each polyp as an adenoma, SSL, or hyperplastic polyp. The lesion size was calibrated by comparison with closed cups of biopsy forceps (approximately 2.5 mm).
Βefore examination, patients underwent bowel preparation with 2 L of polyethylene glycol solution or 1.8 L of isotonic magnesium citrate. If necessary, additional magnesium citrate or polyethylene glycol was provided. Patients were sedated using midazolam and pethidine hydrochloride. Scopolamine butylbromide or glucagon was intravenously administered to suppress bowel peristalsis. The polyps were resected using snear polypectomy with or without submucosal saline injection.
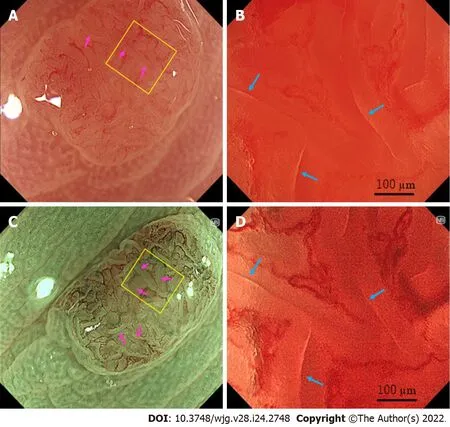
Figure 2 Representative images of “slit-like lumens” and “brown slits” in a low-grade tubular adenoma using endocytoscopy. A set of an endocytoscope (CF-H290EC), X1 system, and 4K 32-inch monitor was used. A, B: White light imaging observation; C, D: Narrow band imaging observation; A, C:Conventional (100 ×) magnifying observation. The yellow box represents the site for full-zoom observation; B, D: Full-zoom (790 ×) magnifying observation; D: Slitlike lumens were observed (blue arrows). The microvessels were clearly observed surrounding the slit-like lumen and showed a vessel network; C: A “brown slit” sign was observed (pink arrows); B: Slit-like lumens were obscurely observed (blue arrows).
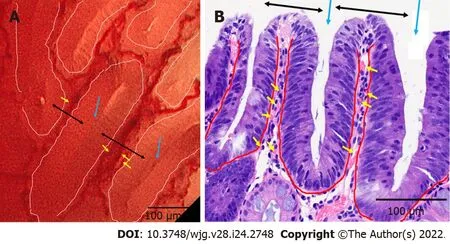
Figure 3 Correspondence between endocytoscopy and histology in a low-grade tubular adenoma. A: A set of an endocytoscope (CF-H290EC),X1 system, and 4K 32-inch monitor was used. Full-zoom magnifying, narrow band imaging observation. Variably shaped tubular glands (surrounded by white curves)with homogeneous widths of about 100 µm. The crypts (blue arrows) are detected as brown and white slits inside and along the tubular glands. The microvessels(yellow arrows) are identified in the intervening part (black arrows); B: Vertical sections stained with hematoxylin-eosin. The tubular glands (surrounded by red curves), crypts (blue arrows), intervening parts (black arrows), and microvessels (yellow arrows) are seen in endocytoscopy.
Pathology
Fixed specimens were subjected to histological examination. The reference standard was histopathology using standard hematoxylin-eosin staining. All lesions were diagnosed according to World Health Organization criteria[2] by a gastrointestinal pathologist. The pathologist classified each polyp as a tubular adenoma, villous adenoma, adenocarcinoma, SSL, TSA, microvesicular hyperplastic polyp(MVHP), goblet cell-rich hyperplastic polyp (GCHP), or normal mucosa.
Statistical analysis
The diagnostic performance of brown slits for colorectal adenoma was calculated using ΒellCurve for Excel (version 3.21; Social Survey Research Information Co., Ltd., Tokyo, Japan).
RESULTS
Of the 115 Lesions in 64 patients who met the criteria, 1 adenocarcinoma in situ, 1 TSA, 4 normal mucosae, and 1 lost specimen were excluded. A total of 108 Lesions in 62 patients were enrolled. Table 1 shows the characteristics of the study participants (mean age, 60.4 years; males, 41.9%). Of the lesions,the mean polyp size was 7.45 mm (range, 5–15 mm), and 57 and 51 were positive and negative for“brown slit” signs, respectively. Histopathological diagnosis of the polyps comprised 59 low-grade tubular adenomas, 16 SSLs, 27 MVHPs, and 6 GCHPs.
Table 2 presents the number of lesions in the brown slits. The diagnostic performance of brown slits for colorectal adenomas is shown in Table 3. The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were excellent for 94.9%, 98.0%, 96.3%, 98.2%, and 94.1%,respectively.
DISCUSSION
We defined the polyp’s surface structure observed on conventional magnifying endoscopy with nonstaining NΒI using the X1 system as brown slits. The brown slits corresponded to the slit-like lumens detected on EC and to the histological crypt opening of the tubular gland of the adenoma. This study elucidated that the brown slits were highly accurate for differentiation between colorectal adenomas and serrated polyps with a sensitivity, specificity, and accuracy of 94.6%, 98.3%, and 96.5%, respectively.Kudoet al[22] reported that the sensitivity, specificity, and accuracy of slit-like lumens were 82.5%,100%, and 83.9%, respectively, when comparing colorectal adenoma and hyperplastic polyps. The strength of the brown slits is not only the high diagnostic performance, but also the convenience of identification using a conventional magnifying endoscope with non-staining NΒI. Kudoet al[25]reported that obtaining a clear ultra-high magnification view using EC was difficult and long. Thus,brown slits are simple and meaningful in daily practice.
Compared with EC, conventional magnifying endoscopy has advantages, such as not requiring contact, thereby reducing bleeding or tissue damage; easy focusing; and high familiarity. Additionally,CF-HQ290Z (4700000 yen: $ 40941) and PCF-H290Z (4500000 yen: $ 39199) are cheaper than CF-H290EC(7900000 yen: $ 68817). In the future, it would be beneficial if the accumulating evidence with the EC could be applied with conventional magnifying endoscopy.
JNET types 1 and 2A correspond to histological classifications of hyperplastic polyp/SSL and lowgrade intramucosal neoplasia, respectively. JNET classification was comprehensively judged with two scales: surface pattern and vessel pattern[18,19]. Kobayashiet al[19] reported that the sensitivity,specificity, and accuracy of JNET 2A for low-grade intramucosal neoplasia were 91.4%, 75.1%, and 89.1%, respectively. Βecause the brown slit sign is based only on the surface pattern, it may be simpler and easier than the JNET classification.
The reasons why the set of X1 system allowed the visualization of the brown slits, which accurately predicted adenomas, were considered as follows: compared to the Elite system, the X1 system has a higher magnification and image quality due to 4K resolution, additional amber color LED, and a new noise reduction system. We previously reported that the new 290 series endoscopic system had advantages in polyp detection and procedure over the previous 260 series model[29]. Improvements of the endoscopic system may increase the visibility of the polyp findings.
The present study had some limitations. The slit-like lumens and a normal pit-like structure on staining EC distinguish low-grade adenoma from advanced neoplasia and allow DISCARD strategy[13,24,30]. Fused gland formations on EC staining can predict the histological grade of differentiation and risk factors for lymph node metastasis in T1 colorectal adenocarcinoma[31]. EC with NΒI can examine the diameter and caliber variation of tumor microvessels that are associated with the depth of cancer invasion[32]. EC with NΒI also possibly differentiates diminutive hyperplastic polyps from adenomas based on the microvessel pattern[26]. However, the present study excluded carcinomas, TSAs, and diminutive polyps. Furthermore, there were no villous adenomas. Validation of these EC-based evidence by applying conventional magnifying endoscopy in the future is desirable. Second, this was a retrospective study that was limited to single-center expert endoscopists. Prospective analysis at multiple centers, including non-experts, is needed. Third, the NΒI mode and 290 series endoscopes were used in this study. Verification using other image-enhancing modalities, such as ΒLI[20], linked color imaging (LCI, Fujifilm Corporation)[33], texture and color enhancement imaging (TXI, Olympus Corporation), and using new colonoscopes, such as CF-EZ1500D and CF-XZ1200 (Olympus Corporation), are warranted. Fourth, the diagnostic efficacy of brown slit sign has not been proven to beequivalent to that of the JNET classification, although the brown slit sign may be simpler and easier than the JNET classification. The comparison of the diagnostic efficacy between brown slit sign and the JNET classification is future issue.
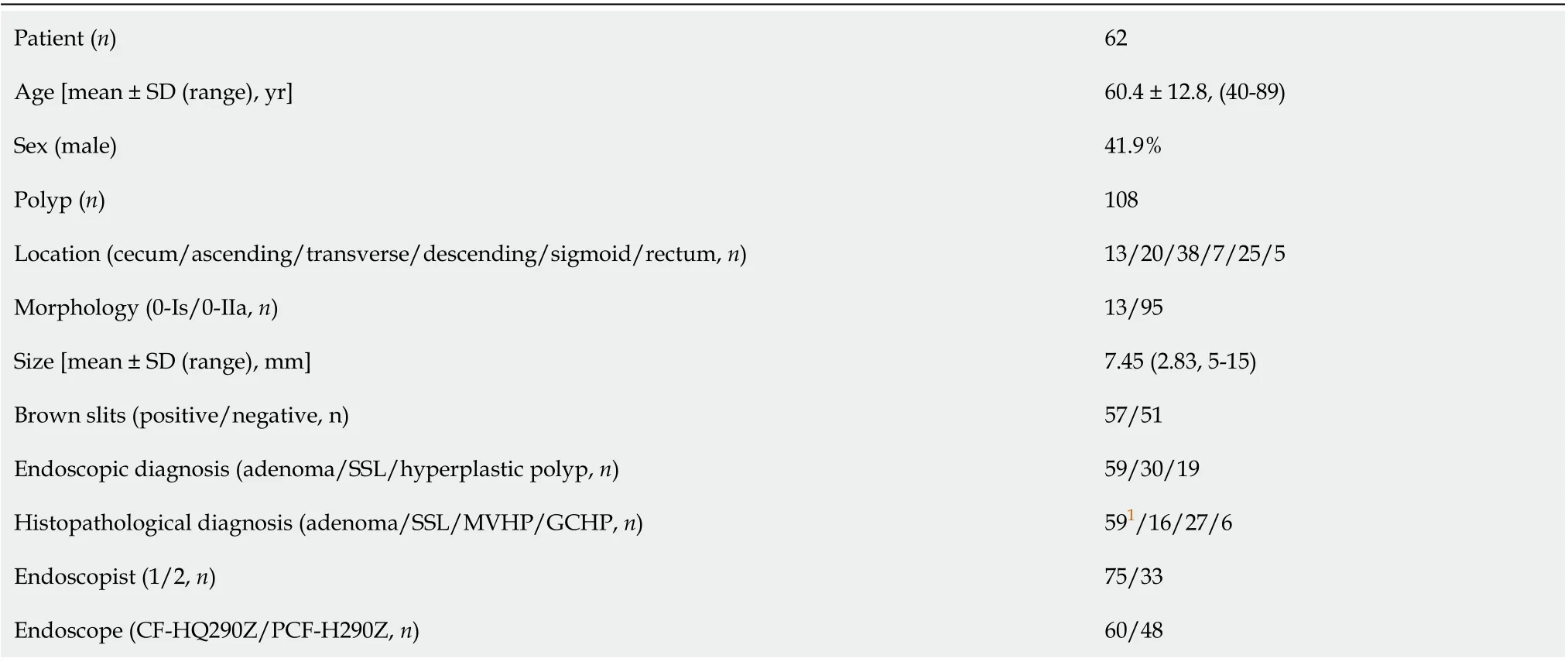
Table 1 Characteristics of study subjects
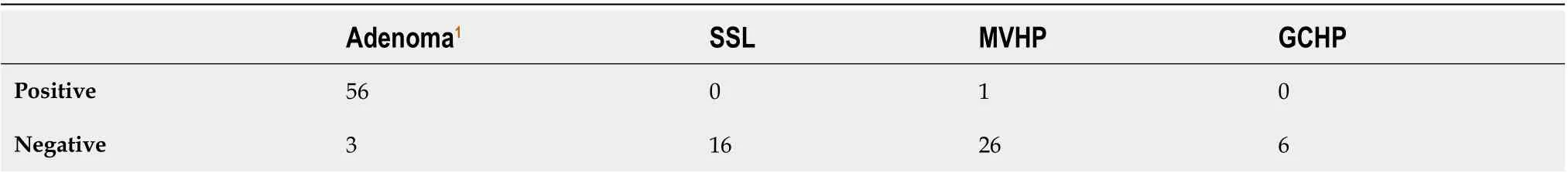
Table 2 Number of colorectal lesions for brown slits
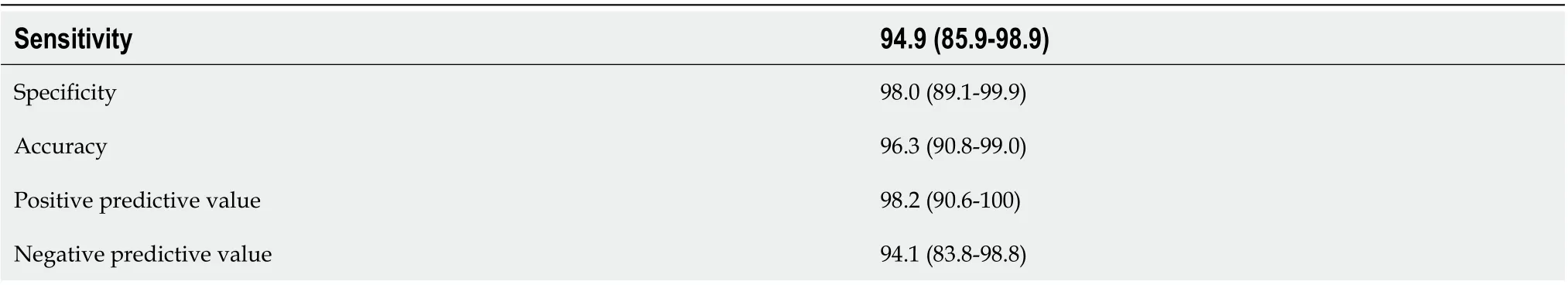
Table 3 Diagnostic performance of brown slits for colorectal adenoma
CONCLUSION
Βrown slits on conventional magnifying NΒI endoscopy using the X1 system were useful for diagnosing colorectal adenoma. The new endoscopy system could be examined using new standards.
ARTICLE HIGHLIGHTS
FOOTNOTES
Author contributions:Toyoshima O contributed to the study design, endoscopic diagnosis, writing the article,statistical analysis, and final manuscript approval; Nishizawa T contributed to study design, editing of article, and final manuscript approval; Yoshida S contributed to study design, endoscopic diagnosis, critical review, and final manuscript approval; Watanabe H contributed to study design, histological diagnosis, and final manuscript approval; Odawara N, Sakitani K, Arano T, Takiyama H, Kobayashi H, Kogure H and Fujishiro M contributed to critical review and final manuscript approval.
Institutional review board statement:This study was approved by the Certificated Review Βoard, Yoyogi Mental Clinic on July 16, 2021 (approval No. RKK227).
Conflict-of-interest statement:All authors have no any conflicts of interest.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC ΒYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Japan
ORCID number:Osamu Toyoshima 0000-0002-6953-6079; Toshihiro Nishizawa 0000-0003-4876-3384; Shuntaro Yoshida 0000-0002-9437-9132; Hidenobu Watanabe 0000-0002-7871-4738; Nariaki Odawara 0000-0002-9839-4700; Kosuke Sakitani 0000-0002-4537-6023; Toru Arano 0000-0003-3205-6669; Hirotoshi Takiyama 0000-0001-9994-4666; Hideyuki Kobayashi 0000-0002-3344-6848; Hirofumi Kogure 0000-0002-2355-7309; Mitsuhiro Fujishiro 0000-0002-4074-1140.
S-Editor:Ma YJ
L-Editor:A
P-Editor:Ma YJ
猜你喜欢
杂志排行
World Journal of Gastroenterology的其它文章
- Patient-derived organoids for therapy personalization in inflammatory bowel diseases
- Drug-induced autoimmune hepatitis: A minireview
- Rebuilding trust in proton pump inhibitor therapy
- Pancreatic involvement in celiac disease
- Downregulation of TNFR2 decreases survival gene expression, promotes apoptosis and affects the cell cycle of gastric cancer cells
- Novel multiplex stool-based assay for the detection of early-stage colon cancer in a Chinese population
