Acupuncture plus naloxone hydrochloride in the treatment of coma after surgery for cerebral hemorrhage: a randomized controlled trial
2022-04-18CHENMin陈敏WUShuangshuang吴双双TANGPeiying汤佩英
CHEN Min (陈敏), WU Shuangshuang (吴双双), TANG Peiying (汤佩英)
The First People’s Hospital of Huzhou, Zhejiang Province, Huzhou 313000, China
Abstract
Keywords: Acupuncture Therapy; Acupuncture Medication Combined; Naloxone; Cerebral Hemorrhage; Brain Edema;Coma; Randomized Controlled Trial
Cerebral hemorrhage is a non-trauma-induced spontaneous brain parenchymal hemorrhage with high mortality and disability rates, and is a common critical illness in neurosurgery[1]. Minimally invasive hematoma removal can promptly remove the majority of intracranial hematomas and reduce intracranial pressure in patients with short operative time and minimal trauma[2]. Although the incidence of postoperative complications is low, postoperative cerebral edema and secondary damage still cannot be completely avoided, so coma after surgery for cerebral hemorrhage is still common[3]. Naloxone hydrochloride is an opioid receptor antagonist, which is administered intravenously to rapidly cross the blood-brain barrier,reduce endorphin release and brain tissue damage,improve cerebral circulation, and improve cerebral metabolism by regulating the balance of prostacyclin and thromboxane, so it is commonly used to promote resuscitation in comatose patients with cerebral hemorrhage[4-5]. Acupuncture, with its effects of dispelling blood stasis and opening the body and awakening the mind, is a common treatment for cerebral hemorrhage and cerebral infarction. It can upregulate the expression of neurotrophic factors,inhibit inflammatory responses, improve cerebral hemodynamics, and promote the repair of neurological damage[6]. In this study, acupuncture combined with naloxone hydrochloride was used to treat coma after surgery for cerebral hemorrhage and compared with naloxone hydrochloride treatment alone to observe its efficacy and explore its possible mechanism of action.
1 Clinical Materials
1.1 Diagnostic criteria
The Diagnosis was made according to the diagnostic criteria for cerebral hemorrhage in theKey Diagnostic Points for Cerebrovascular Diseases[7]. The onset of the disease is rapid and progresses rapidly, with impaired consciousness, limb hemiparesis, headache, nausea and vomiting as the main symptoms; CT examination can clarify the site of bleeding.
1.2 Inclusion criteria
Met the diagnostic criteria for cerebral hemorrhage;75 years old or younger; had undergone minimally invasive hematoma removal, remained comatose 3-7 d after surgery, and had a Glasgow coma scale (GCS) score of 5-8 points; obtained informed consent from the patient’s family.
1.3 Exclusion criteria
Patients with cerebral hemorrhage caused by other reasons such as trauma or tumor; those who were already in a deep coma with unstable vital signs,advanced brain herniation, or bilateral dilated pupils at the time of admission; those with unstable postoperative vital signs; and those with combined serious underlying diseases.
1.4 Criteria for elimination and dropout
Those whose condition deteriorated during the trial;those whose family members requested to withdraw from the trial on their own initiative; those who did not follow medical advice and used other drugs or therapies;those with incomplete information.
1.5 Statistical analysis
SPSS version 22.0 statistical software was used for data analysis. Count data were tested by Chi-square test.The measurement data conforming to normal distribution and homogeneity of variance were expressed as mean ± standard deviation (±s) and processed byt-test; the measurement data not conforming to normal distribution or homogeneity of variance were tested by nonparametric test.P<0.05 was considered a statistically significant difference.
1.6 General data
Seventy-two patients admitted to our hospital between August 2018 and September 2019 who were in a coma after surgery for cerebral hemorrhage were selected as study subjects. They were divided into a control group and an observation group according to the random number table method, with 36 cases in each group. During the study, due to deterioration, two cases dropped out in the control group and the remaining 34 cases completed the trial, with a dropout rate of 5.6%; one case dropped out in the observation group and the remaining 35 cases completed the trial,with a shedding rate of 2.8%. There was no statistical difference between the two groups in terms of gender,age, bleeding volume and site (P>0.05), indicating that the two groups were comparable (Table 1).
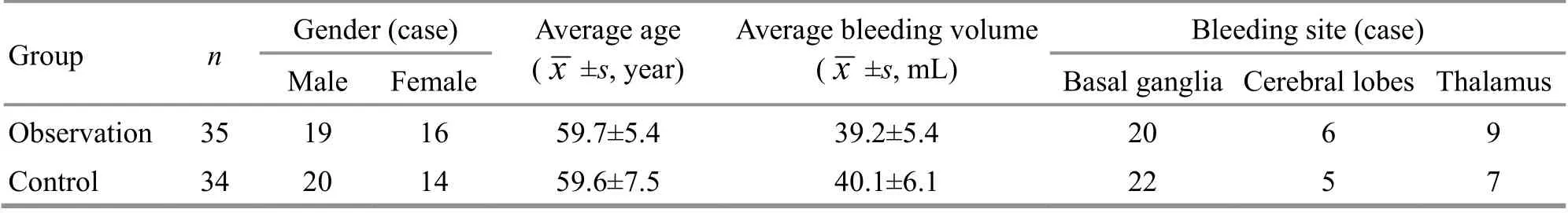
Table 1. Baseline characteristics of the two groups
2 Treatment Methods
Both groups were given monitoring of vital signs,oxygenation, dehydration to lower intracranial pressure,blood pressure control, cerebral nerve protection,nutritional support, maintenance of water, electrolyte,acid-base balance, and other symptomatic treatments.
2.1 Control group
After minimally invasive hematoma removal, 4 mg of naloxone hydrochloride (State Food and Drug Administration Approval No. H20054907, Shandong Xinhua Pharmaceutical Co., Ltd., China) was added to 250 mL of 5% glucose solution, and was administered intravenously once per day for 1 month.
2.2 Observation group
Acupuncture was used additionally besides the drug treatment used in the control group.
Acupoints: Shuigou (GV26), Baihui (GV20), and bilateral Neiguan (PC6) and Taichong (LR3).
Methods:The acupoints were positioned with reference to theScience of Meridians and Acupoints[8].After routine sterilization, sterile acupuncture needles of 0.25 mm in diameter and 25 mm in length were used.The acupuncture needle was inserted obliquely upward by about 10 mm into Shuigou (GV26) with the sparrow-pecking manipulation; the acupuncture needle was inserted subcutaneously forward about 8 mm into Baihui (GV20) with the reducing manipulation of twisting-rotating; Neiguan (PC6) and Taichong (LR3)were punctured perpendicularly by about 10 mm. The needles were retained for 30 min. The acupuncture treatment was done once a day, and rested for 2 d after 5 d of consecutive treatment, for a total of one month.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 Awakening rate
The awakening rate was compared between the two groups after treatment. The criterion for awakening was GCS score ≥9 points[9].
3.1.2 GCS score
The GCS score was compared between the two groups before and after treatment. A lower GCS score indicates a severer impairment of consciousness[10].
3.1.3 Cerebral edema volume
Cranial CT examinations were performed on the patients before and after treatment, and the volume of cerebral edema was calculated according to the Coniglobus formula[11].
3.1.4 Mean velocity (Vm) of middle cerebral artery
The middle cerebral artery Vm was compared between the two groups before and after treatment.
3.1.5 Cerebrospinal fluid Caspase-3 and macrophage migration inhibitory factor (MIF) levels
Before and after treatment, 5 mL of cerebrospinal fluid was extracted by lumbar puncture. The Caspase-3 level was measured by enzyme-linked immunosorbent assay, and the MIF level was measured by immunoradiometric assay.
3.2 Results
3.2.1 Comparison of the awakening rate
The awakening rate in the observation group was 62.9%, which was significantly higher than that in the control group, which was 26.5% (P<0.05), (Table 2).
3.2.2 Comparison of the GCS score
There was no statistical difference in the GCS score between the two groups before treatment (P>0.05).After treatment, the GCS score improved in both groups(P<0.05), and was higher in the observation group than in the control group (P<0.05). For details, see Table 3.
3.2.3 Comparison of the cerebral edema volume
There was no statistical difference in the volume of brain edema between the two groups before treatment(P>0.05). After treatment, the brain edema volume decreased in both groups (P<0.05), and was lower in the observation group than in the control group (P<0.05).For details, see Table 4.

Table 2. Comparison of the awakening rate between the two groups
Table 3. Comparison of the GCS score between the two groups(±s point)
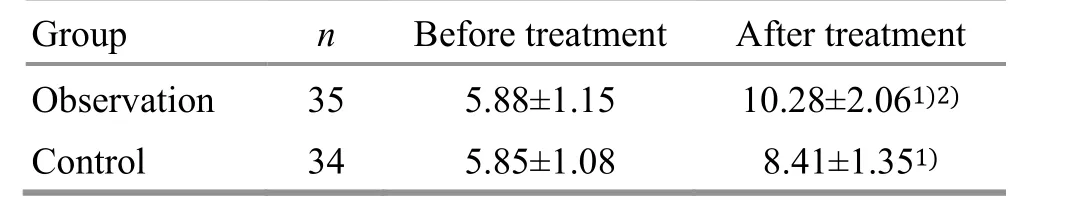
Table 3. Comparison of the GCS score between the two groups(±s point)
Note: GCS=Glasgow coma scale; compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Observation 35 5.88±1.15 10.28±2.061)2)34 5.85±1.08 8.41±1.351)Control
Table 4. Comparison of the cerebral edema volume between the two groups (±s mL)

Table 4. Comparison of the cerebral edema volume between the two groups (±s mL)
Note: Compared with the same group before treatment, 1) P<0.05;compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Observation 35 24.97±4.15 9.49±3.331)2)34 24.62±4.07 14.65±2.821)Control
3.2.4 Comparison of the middle cerebral artery Vm
There was no statistical difference in the middle cerebral artery Vm between the two groups before treatment (P>0.05). After treatment, the middle cerebral artery Vm increased in both groups (P<0.05),and was higher in the observation group than in the control group (P<0.05). For details, see Table 5.
3.2.5 Comparison of the cerebrospinal fluid Caspase-3 and MIF levels
There was no statistical difference in the levels of cerebrospinal fluid Caspase-3 and MIF between the two groups before treatment (P>0.05). After treatment, the cerebrospinal fluid Caspase-3 and MIF levels were significantly lower in both groups (P<0.05), and were lower in the observation group than in the control group (P<0.05). For details, see Table 6.
Table 5. Comparison of the middle cerebral artery Vm between the two groups (±s cm/s)

Table 5. Comparison of the middle cerebral artery Vm between the two groups (±s cm/s)
Note: Vm=Mean velocity; compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Observation 35 67.77±4.09 90.64±7.681)2)Control 34 67.62±4.29 80.15±6.431)
Table 6. Comparison of the cerebrospinal fluid Caspase-3 and MIF levels between the two groups (±s)
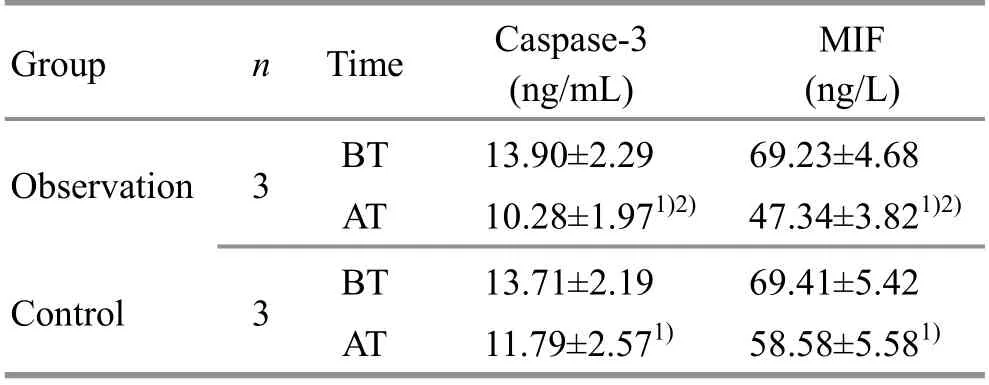
Table 6. Comparison of the cerebrospinal fluid Caspase-3 and MIF levels between the two groups (±s)
Note: BT=Before treatment; AT=After treatment; MIF=Macrophage migration inhibitory factor; compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Caspase-3(ng/mL)MIF(ng/L)Observation 3 BT 13.90±2.29 69.23±4.68 AT 10.28±1.971)2) 47.34±3.821)2)Control 3 BT 13.71±2.19 69.41±5.42 AT 11.79±2.571) 58.58±5.581)
4 Discussion
Intracranial hypertension formed by cerebral hemorrhage causes displacement and deformation of the brain tissue and downward compression of the brainstem, which in severe cases can lead to brain herniation and diffuse damage to the cerebral cortex or brainstem reticular formation, which in turn leads to coma[12-13]. Coma can induce complications in all systems, especially in the respiratory system. The duration and degree of coma largely affect the prognosis of patients; the inability to take care of oneself during coma poses a great economic and mental burden to the family[14-15]. Therefore, the search for effective wake-up promotion methods to accelerate the awakening of patients in coma after cerebral hemorrhage and improve their neurological function and prognosis is an important topic of current neuroscience concern.
Coma after surgery for cerebral hemorrhage belongs to the category of “wind stroke” and “mental fainting”in traditional Chinese medicine, with unconsciousness,hemiparesis of limbs, and distorted eyes and mouth as the main manifestations[16]. Stagnation of Qi, deficiency of Qi and blood, or phlegm blocking the ligaments, or heat forcing blood to move in chaos can lead to the formation of blood stasis; under certain circumstances,Qi and blood reverse and offend the brain, resulting in blood overflowing outside the veins and loss of the use of the brain and coma[17]. It can be seen that blood stasis is always present in the disease and affects its prognosis, so the treatment should be based on invigorating blood and dissolving blood stasis, opening the orifices and awakening the mind[18].
Shuigou (GV26) and Baihui (GV20), Neiguan (PC6),and Taichong (LR3) are commonly used acupoints for the treatment of “stroke” and “fainting”. Shuigou (GV26)is the crossing point of the Governor Vessel and Yangming Meridians of Hand and Foot. It can open the orifices and awaken the brain and unblock the meridians. Baihui (GV20) is located on the top of the head, and can extinguish the wind and wake up the brain, and raise the Yang to solidify the weakness. These two acupoints are both important for first aid. Neiguan(PC6) is one of the Confluent Points of the Eight Extraordinary Vessels. It is connected to the Yin link Vessel and can nourish the heart and calm the mind and dredge Qi and blood. Taichong (LR3) is the Yuan-Primary point of the Liver Meridian of Foot Jueyin. It regulates Qi and blood, calms the liver, and extinguishes the wind.Together, these acupoints work to open the orifices and awaken the mind, regulate Qi and blood, and unblock the meridians to repair the damaged reticular system of the brainstem and promote the awakening of patients in a coma after surgery for cerebral hemorrhage.
The results of the study showed that the awakening rate of the observation group was higher than that of the control group after treatment, and the volume of cerebral edema was smaller than that of the control group, showing that acupuncture has an important role in improving the awakening rate of patients, reducing the degree of coma and the volume of cerebral edema,and enhancing the cerebral blood flow rate.
Caspase-3 is the main executor of apoptosis, and its expression level is used to assess the level of apoptosis[19]. One study showed that Caspase-3 expression was significantly increased in brain tissue of rats in a cerebral hemorrhage model and peaked at 24-75 h, indicating that elevated Caspase-3 expression can occur after cerebral hemorrhage, causing apoptosis of neural cells and aggravating brain injury[20]. MIF can inhibit macrophage wandering mobile function,promote the secretion of multiple cytokines by macrophages, and indirectly exert inflammatory regulatory functions. It is closely related to cardiovascular diseases such as atherosclerosis,coronary heart disease, and hypertension[21]. MIF can promote the secretion of inflammatory factors such as high-sensitivity C-reactive protein and tumor necrosis factor-α, aggravate the inflammatory response of the body, and is positively correlated with the degree of neurological injury in cerebral hemorrhage[22]. The results of this study showed that the levels of cerebrospinal fluid Caspase-3 and MIF were reduced in both groups after treatment, and were lower in the observation group than in the control group (P<0.05).This indicates that acupuncture can reduce the levels of cerebrospinal fluid Caspase-3 and MIF in the patients.
Acupuncture combined with naloxone hydrochloride for the treatment of coma after surgery for cerebral hemorrhage can promote the patients' awakening,improve the degree of coma, reduce the volume of cerebral edema, and enhance cerebral blood flow velocity, producing a better effect than naloxone hydrochloride used alone; this may be related to its reduction of cerebrospinal fluid Caspase-3 and MIF levels.
Conflict of Interest
There is no potential conflict of interest in this article.
Acknowledgments
There was no project fund support for this study.
Statement of Informed Consent
Informed consent was obtained from guardians of all individual participants.
Received: 16 November 2020/Accepted: 27 April 2021
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture on angiogenesis and cortical VEGF and BDNF expression in rats with focal cerebral ischemia
- Therapeutic efficacy observation of warm needling moxibustion plus Tuina for knee osteoarthritis
- Reduction of serum level of interleukin-2 and pruritus severity after acupuncture at Quchi (LI11) in hemodialysis patients: a placebo-controlled randomized clinical trial
- Clinical observation of pediatric Tuina plus oral Chinese medication for pediatric anorexia due to spleen failing in transportation
- Protocol-optimizing study of combining Tuina and horse-riding squat exercise for knee osteoarthritis
- Therapeutic efficacy of acupuncture plus Tuina for spastic cerebral palsy and discussion of its mechanism