Protocol-optimizing study of combining Tuina and horse-riding squat exercise for knee osteoarthritis
2022-04-18XINGHua邢华SHENJiayun沈佳韵GONGLi龚利LIJianhua李建华SHAOSheng邵盛CHUYuzhou储宇舟HEPengfei何鹏飞CHENHao陈浩KANGZhiran康知然DAIDacheng戴大城
XING Hua (邢华), SHEN Jiayun (沈佳韵), GONG Li (龚利), LI Jianhua (李建华), SHAO Sheng (邵盛),CHU Yuzhou (储宇舟), HE Pengfei (何鹏飞), CHEN Hao (陈浩), KANG Zhiran (康知然), DAI Dacheng (戴大城)
1 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
2 Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai 200071, China
Abstract
Keywords: Tuina; Massage; Manual Therapies; Physical and Breathing Exercises; Horse-riding Squat Exercise; Osteoarthritis,Knee; Factorial Design
Knee osteoarthritis (KOA) is a degenerative disease involving multiple risk factors with joint pain as the main symptom[1]. Its main characteristics include articular cartilage degeneration and destruction and hyperostosis. Most KOA patients suffer from knee pain.This pain will inhibit the lower-extremity muscle strength, resulting in joint dysfunction[2]. KOA is getting prevalent with the aging of society. As a chronic degenerative disease, it brings a great burden to both individuals and the social economy due to its recurrent and prolonging features[3]. Therefore, it has become a great deal to seek an effective treatment protocol that is also safe, easy to operate, and economical in treating KOA.
According to the guidance provided by the American Academy of Orthopedic Surgeons (AAOS) in 2013,evidence-based research recommends improving the KOA symptoms and function through training of lower-extremity muscle strength. One of the recommended exercises is half-squat exercise, which can help with the muscle strength around the knee joint(quadriceps femoris and hamstring muscles in particular), strengthen the stability of the joint, improve the knee joint flexion and extension, and reduce clinical symptoms[4]. This half-squat exercise is quite similar to the horse-riding squat exercise in traditional Tuina(Chinese therapeutic massage) Qigong exercise. Hence,we adopted this half-squat exercise in this trial as the training of horse-riding squat exercise. Training and without training were taken as the two levels in the factorial design.
Tuina consists of manipulations and Qigong exercise.But the two components have been rarely studied simultaneously in the treatment of KOA to explore the main effects and their interactions. Different manipulations have different emphases. The sitting knee-adjustment manipulation focuses on the correction of bones, while the Gun-Rolling manipulation stresses the treatment of tendons. As a form of Qigong exercise, the horse-riding squat exercise emphasizes the static pulling of tendons. Then there arise questions regarding Tuina treatment of KOA, including how to select and combine them in treating KOA and their relationships with knee pain and function evaluation.
This study observed the effects of Tuina manipulation and horse-riding squat exercise on the knee joint function and clinical efficacy for early- and middle-stage KOA, to find the optimal protocol to combine Tuina manipulation and horse-riding squat exercise in the treatment of this condition and offer clinical evidence.
1 Clinical Materials
1.1 Trial design and randomization
This study adopted a 2×2 factorial design. Factor A was Tuina manipulation whose two levels were Gun-Rolling manipulation (A1) and sitting knee-adjustment(A2), respectively. Factor B was horse-riding squat exercise whose two levels were training (B1) and without training (B2), respectively.
The participants were randomized at 1:1:1:1 into a manipulation group (group A1B2), a manipulation plus horse-riding squat exercise group (group A1B1), a sitting knee-adjustment group (group A2B2), and a sitting knee-adjustment plus horse-riding squat exercise group(group A2B1). The random assignments were hidden in opaque envelopes. The participants randomly chose and opened one envelope to determine the allocation.
This trial had been registered on the Chinese Trial Registry (No. ChiCTR-INR-17011916) and ethically approved by Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine (No. 2015034).
1.2 Participants
A total of 120 KOA patients were recruited between June 1, 2018 and January 20, 2020 at the Tuina Department of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine.
1.2.1 Diagnostic criteria
Conformed to the clinical and radiological diagnostic criteria for KOA stipulated by the American College of Rheumatology in 1995[5].
(1) Knee joint pain occurred most of the time in the recent months; (2) X-ray demonstrated osteophyte formation; (3) the synovial fluid analysis confirmed osteoarthritis (clear, sticky, white blood cell count<2×109/L); (4) age ≥40 years old; (5) morning stiffness≤30 min; (6) crepitus during joint movements.
KOA can be diagnosed when (1) and (2), or (1), (3), (5),and (6), or (1), (4), (5), and (6) were met.
1.2.2 Inclusion criteria
Conformed to the diagnostic criteria for KOA; aged 38 to 70 years old; voluntarily participated in this trial and signed the informed consent form; evaluated ≤grade III by Kellgren-Lawrence (K-L).
1.2.3 Exclusion criteria
With a history of knee joint trauma or surgery; knee joint tumor, tuberculosis, osteomyelitis, or other diseases involving the knee joint; psoriasis, syphilitic neuropathy, metabolic bone disease, or acute trauma;severe liver or kidney dysfunction, cardiovascular disease, or diabetes; mental disorders; participated in another clinical trial during the previous three months;took medications for KOA or chondroprotective agents during the previous six months; skin lesion on the knee joint; other improper conditions.
1.3 Main instruments
The Gait Watch three-dimensional gait analysis system (Zhanghe Electric Co., Ltd., China) was used for gait analysis. This system consists of seven highprecision real-time acquisition sensors and a computer to capture the movements of each joint of the patient and display the real-time three-dimensional walking model and curves. The contained gait collection and data analysis software, version 2.3.7, can provide and analyze gait data, including step length, stride, walking speed, joint flexion angle, and stance phase. The Biodex System 3 isokinetic muscle strength tester (Biodex, USA)was used to measure muscle strength before and after the intervention to obtain the flexor and extensor peak torques.
1.4 Statistical methods
SPSS version 23.0 software was adopted for data analyses. Measurement data in normal distribution and equal variance were expressed as mean ± standard deviation (±s) and tested using the pairedt-test for intra-group comparisons and theF-test and SNK-qpairwise multiple comparisons for between-group comparisons. Those not conforming to normal distribution were expressed as median (minimum,maximum) [M (min, max)] and tested using the Wilcoxon rank-sum test. The Kruskal-Wallis H rank-sum test and Nemenyi pairwise multiple comparisons were used when normal distribution or homogeneity of variance was not met. The 2×2 factorial analysis of variance was used for studying the main effect,individual effect, and interactions of factors A and B.The rank-transformation 2×2 factorial analysis of variance was used for between-group comparisons. The enumeration data were described using frequency,constituent ratio, or rate. The Chi-square test was used to process between-group comparisons of dichotomous or polytomous disordered data. The ordered ranked data were analyzed using the Kruskal-Wallis H rank-sum test and Nemenyi pairwise multiple comparisons.P<0.05 was considered statistically significant.
1.5 Quality control
The research staff rigorously followed the randomization principle and the inclusion and exclusion criteria. The manipulation and horse-riding squat training were conducted by professional physicians according to the treatment plan to ensure the treatment unity. The gait data and isokinetic muscle strength were collected, and the pertinent forms were filled under the guidance of professionals based on the research plan. Two individuals were assigned to enter the information to guarantee precision. During the research, the relevant medications and other exercises were restricted. Patients who were assigned to receive horse-riding squat training practiced under the guidance of professionals prior to the manipulation treatment to ensure training quality.
2 Interventions
This study referred to the Tuina treatment for KOA in theScience of Tuina[6]. The horse-riding squat exercise adopted in the current study is a novel training method referring to theScience of Tuina Qigong Exercise[7]and the half squat exercise recommended by the AAOS.
2.1 Manipulation group (group A1B2)
The patient took a supine position, while the physician was standing by the patient’s affected side performing the following manipulations for the affected limb: Gun-Rolling the quadriceps femoris (Figure 1) and Anrou-Pressing and Kneading Heding (EX-LE2), Xuehai(SP10), Futu (ST32), and Liangqiu (ST34). Then the patient lay on the belly, and the physician performed Gun-Rolling manipulation along the back of the leg and Na-Grasping manipulation at Weizhong (BL40) and Chengshan (BL57). Finally, the physician Ca-Rubbed around the knee joint till the hot sensation penetrated inside. The Gun-Rolling manipulation was done at a frequencyof 140 times/min for 20 min each session,three sessions each week, and for 4 weeks in total.

Figure 1. Gun-Rolling manipulation
2.2 Manipulation plus horse-riding squat exercise group (group A1B1)
The Tuina manipulations were performed as same as those in group A1B2. The horse-riding squat was trained as follows (Figure 2).
The left leg takes a step toward the left or the right foot takes a step toward the right with the feet shoulder-width apart. Raise both hands up horizontally.
If necessary, hold the back of a chair or a wall to maintain balance. Bend the knees and hips to squat within the tolerable range. Meanwhile, keep the back straight and stomach in. Hold this posture for 5 s and then stand tall slowly. Repeat this posture after a 2-second rest. The patients were asked to do this exercise 10 times as a set, 3 sets each session,3 sessions each week, and for 4 weeks.

Figure 2. Horse-riding squat exercise
2.3 Sitting knee-adjustment group (group A2B2)
The patient and the physician were seated face to face. The patient placed the feet steadily on the ground while the physician used his feet to fix the patient’s ankle of the affected side in an anatomic neutral position. Then the practitioner put the thumbs at the patient’s Neixiyan (EX-LE4) and Dubi (ST35) and the rest fingers around the patient’s knee. At this moment, the patient was asked to stand up, during which the foot of the affected side should not leave the ground. If necessary, some support can be provided. The patient needed to look straight ahead, with the head up and back straight. Extended the affected knee as much as possible within the normal range. During this process,the physician needed to fix the thumbs where they were and offered a rotating force internally and externally to relax the tibiofemoral and patellofemoral joints. After three times, the patient sat properly,looking straight forward. Finally, the physician stimulated the patient’s flexors and extensors around the knee with Tanbo-Plucking, An-Pressing, and Rou-Kneading manipulations, especially the quadriceps femoris, hamstring, and gastrocnemius (Figure 3). The treatment was conducted 3 times a week for a total of 4 weeks.
2.4 Sitting knee-adjustment plus horse-riding squat group (group A2B1)
The sitting knee-adjustment treatment was performed as same as in group A2B2, and the horseriding squat exercise was practiced as same as in group A1B1, three times a week for 4 weeks.

Figure 3. Sitting knee-adjustment
3 Outcome Observation
3.1 Outcome measures
3.1.1 Major efficacy measure
Before and after the 4-week intervention, the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) was used to evaluate the major efficacy of the four treatment protocols for KOA.WOMAC consists of 24 questions, and each question is scored in a range of 0-10 points using the visual analog scale (VAS).
3.1.2 Secondary efficacy measures
Before and after the 4-week intervention, gait analysis and isokinetic muscle strength test were conducted to measure the secondary efficacy of the four treatment protocols for KOA. We chose step length,stride, walking speed, and the maximum knee-joint flexion angle as the major items for gait analysis. In the isokinetic muscle strength test, we observed the extensor and flexor peak torques at 60 °/s and 180 °/s.
3.2 Results
3.2.1 Homogeneity test of the baseline data
There were no dropouts in the four groups. The age,gender, body mass index (BMI), disease duration, and K-L grading were statistically equal across the four groups before the intervention (P>0.05), suggesting the comparability (Table 1).
3.2.2 Comparison of the major efficacy measure WOMAC
The Cronbach's α was determined as 0.701-0.774 for WOMAC and its components, indicating that WOMAC has high credibility.
After the intervention, the WOMAC general score dropped significantly in the four groups (P<0.01), while the between-group differences in the WOMAC general score were statistically insignificant (P>0.05). The details are shown in Table 2.
The main effect of manipulation was significant in affecting the WOMAC general score (P<0.05). The main effect of horse-riding squat exercise was insignificant in affecting the WOMAC general score (P>0.05). The interaction of the two factors produced an insignificant effect on the WOMAC general score (P>0.05). The details are shown in Table 3.

Table 1. Comparison of the baseline data of the four groups

Table 2. Comparison of the WOMAC general score before and after treatment
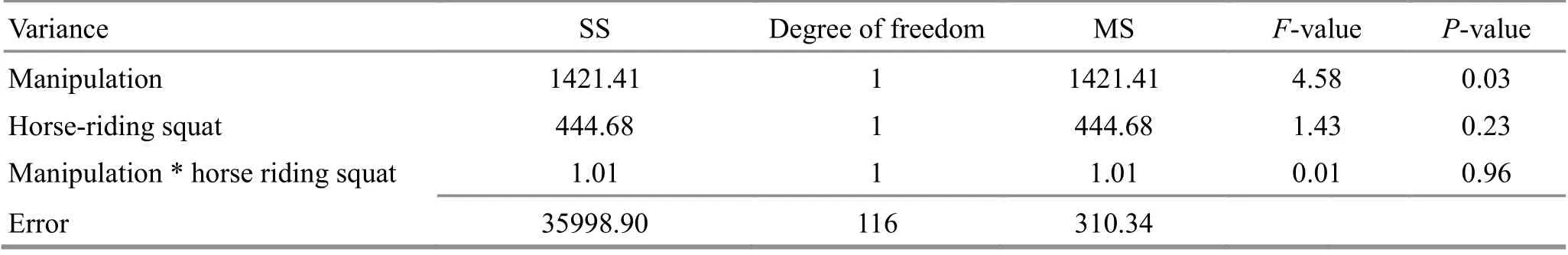
Table 3. Analysis of variance of the effects of manipulation and horse-riding squat on the WOMAC general score
After the intervention, the WOMAC pain score dropped significantly in the four groups (P<0.01), while the between-group differences were statistically insignificant among the four groups (P>0.05). The details are shown in Table 4.
The main effects of both manipulation and horseriding squat were significant in affecting the WOMAC pain score (P<0.01). However, the interaction of the two factors was insignificant in changing the WOMAC pain score (P>0.05). The details are shown in Table 5.
After treatment, the WOMAC stiffness score declined notably in the four groups (P<0.01), and theF-test revealed significant between-group differences in the WOMAC stiffness score among the four groups (P<0.05).Further, the SNK-q pairwise test showed that the WOMAC stiffness score was lower in the manipulation plus horse-riding squat group, sitting knee-adjustment group, and sitting knee-adjustment plus horse-riding squat group than in the manipulation group after the intervention, presenting statistical significance (P<0.05).Moreover, compared with the sitting knee-adjustment plus horse-riding squat group, the WOMAC stiffness score was significantly higher in the manipulation group,manipulation plus horse-riding squat group, and sitting knee-adjustment group (P<0.05). Please see details in Table 6.
The main effect of manipulation was insignificant in influencing the WOMAC stiffness score (P>0.05). The main effect of horse-riding squat was significant in affecting the WOMAC stiffness score (P<0.01). The interaction of the two factors was insignificant in changing the WOMAC stiffness score (P>0.05). The details are shown in Table 7.
After treatment, the WOMAC daily function score declined significantly in the four groups (P<0.01), but the inter-group differences in the WOMAC daily function score were statistically insignificant among the four groups (P>0.05). Please see details in Table 8.
Neither the main effect of manipulation nor that of horse-riding squat was significant in influencing the WOMAC daily function score (P>0.05). The interaction of the two factors did not notably affect the WOMAC daily function score (P>0.05). The details are shown in Table 9.

Table 4. Comparison of the WOMAC pain score before and after treatment

Table 5. Analysis of variance of the effects of manipulation and horse-riding squat on the WOMAC pain score

Table 6. Comparison of the WOMAC stiffness score before and after treatment

Table 7. Analysis of variance of the effects of manipulation and horse-riding squat on the WOMAC stiffness score

Table 8. Comparison of the WOMAC daily function score before and after treatment

Table 9. Analysis of variance of the effects of manipulation and horse-riding squat on the WOMAC daily function score
3.2.3 Comparison of the secondary efficacy measures
After the intervention, the step length changed significantly in the manipulation and manipulation plus horse-riding squat groups (P<0.05), while the change was statistically insignificant in the sitting kneeadjustment and sitting knee-adjustment plus horseriding squat groups (P>0.05). The inter-group differences in the step length were statistically insignificant among the four groups (P>0.05). The details are shown in Table 10.
The main effects of manipulation and horse-riding squat, and their interaction were insignificant in affecting the step length (P>0.05). Please see Table 11 for details.
After treatment, the stride changed markedly in the manipulation plus horse-riding squat group (P<0.05),while the changes in the other three groups were statistically insignificant (P>0.05). The inter-group differences in the stride were statistically significant among the four groups (P>0.05). The details are shown in Table 12.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in influencing the stride (P>0.05). The details are shown in Table 13.
After the intervention, the walking speed changed significantly in the manipulation plus horse-riding squat group (P<0.01), while the changes in the other three groups were statistically insignificant (P>0.05). The inter-group differences in the walking speed were statistically insignificant among the four groups (P>0.05).The details are shown in Table 14.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in influencing the walking speed (P>0.05). Please see details in Table 15.torque at 60 °/s (P>0.05), and the between-group differences were statistically insignificant among the four groups (P>0.05). The details are shown in Table 18.
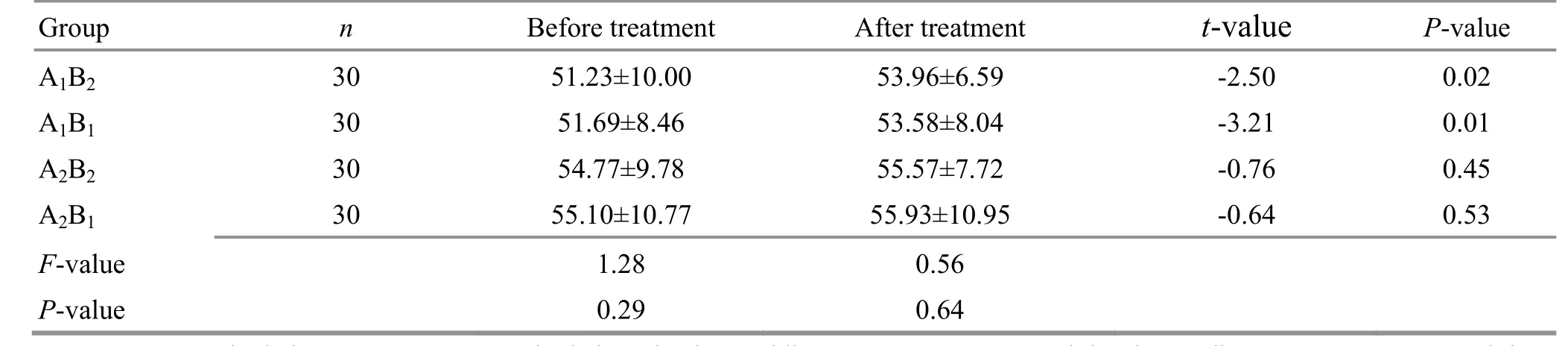
Table 10. Comparison of step length before and after treatment
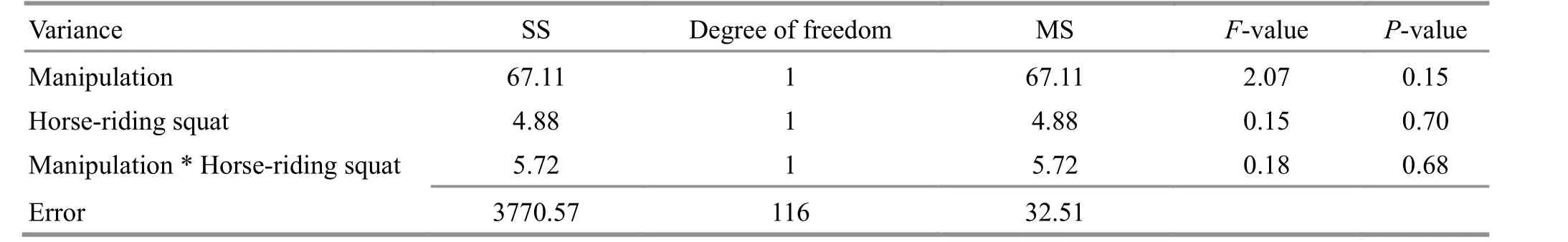
Table 11. Analysis of variance of the effects of manipulation and horse-riding squat on step length
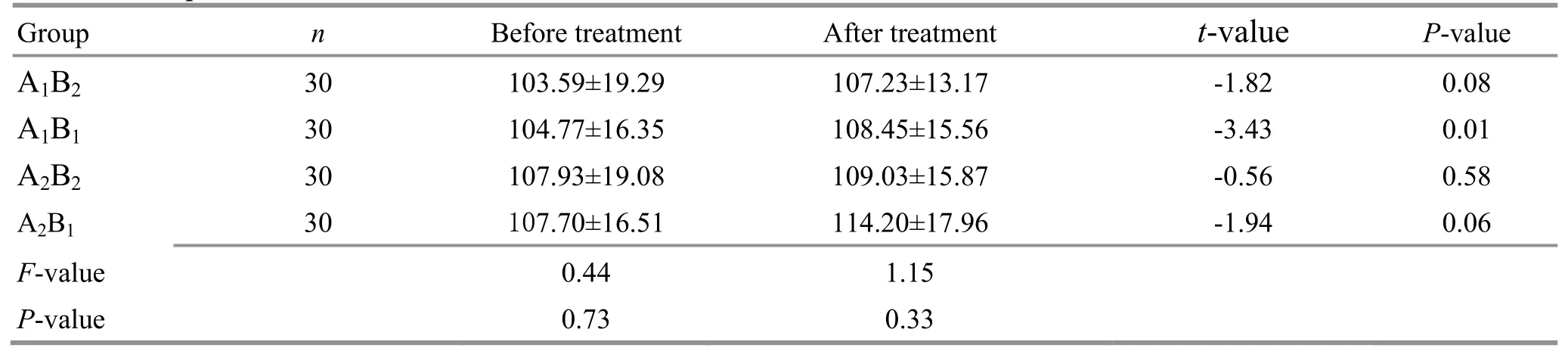
Table 12. Comparison of the stride before and after treatment

Table 13. Analysis of variance of the effects of manipulation and horse-riding squat on the stride
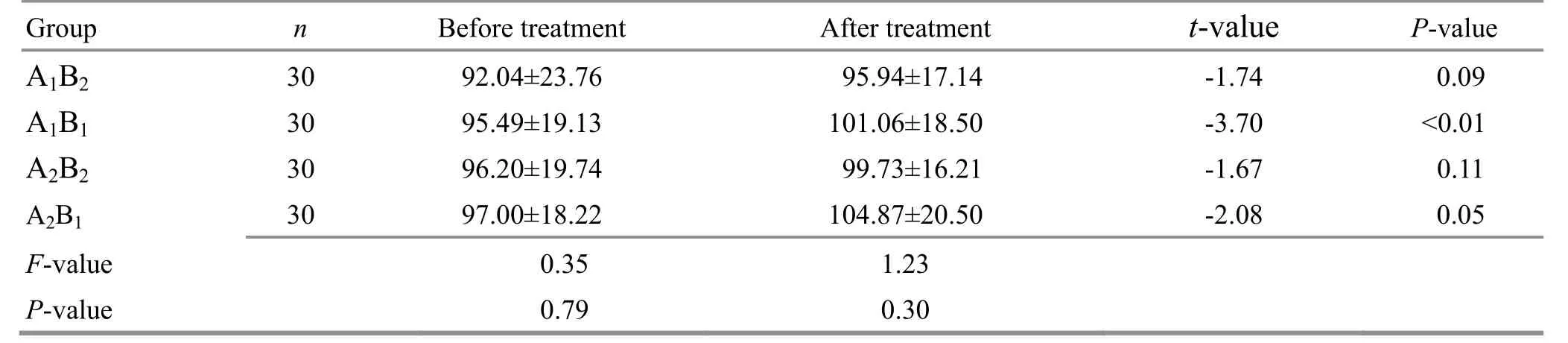
Table 14. Comparison of the walking speed before and after treatment

Table 15. Analysis of variance of the effects of manipulation and horse-riding squat on the walking speed
The main effects of manipulation and horse-riding squat and their interaction were insignificant in influencing the extensor peak torque at 60 °/s (P>0.05).Please see Table 19 for details.
After the intervention, none of the four groups showed a significant change in the flexor peak torque at 60 °/s (P>0.05), and the between-group differences were statistically insignificant among the four groups(P>0.05). The details are shown in Table 20.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in changing the flexor peak torque at 60 °/s (P>0.05).Please see Table 21 for details.
3.2.4 Comparison of flexion angle and extensor peak torque
After treatment, the maximum knee-joint flexion angle changed significantly in the manipulation plus horse-riding squat group (P<0.01), while the changes in the other three groups were statistically insignificant(P>0.05). There were no significant between-group differences in the maximum knee-joint flexion angle among the four groups (P>0.05). The details are displayed in Table 16.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in influencing the maximum knee-joint flexion angle(P>0.05). Please see Table 17 for details.
After the intervention, none of the four groups showed a significant change in the extensor peak

Table 16. Comparison of the maximum knee-joint flexion angle before and after treatment

Table 17. Analysis of variance of the effects of manipulation and horse-riding squat on the maximum knee-joint flexion angle
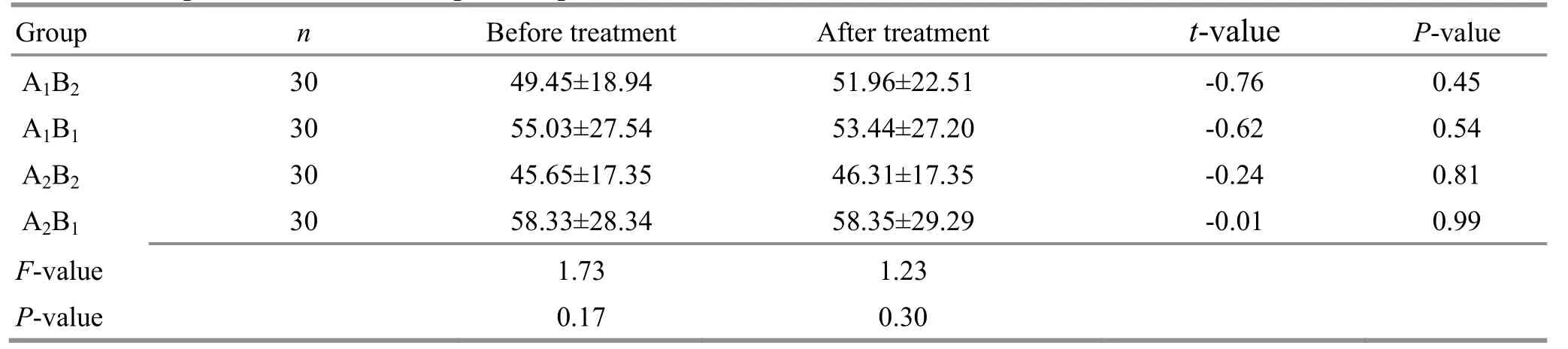
Table 18. Comparison of the extensor peak torque at 60 °/s
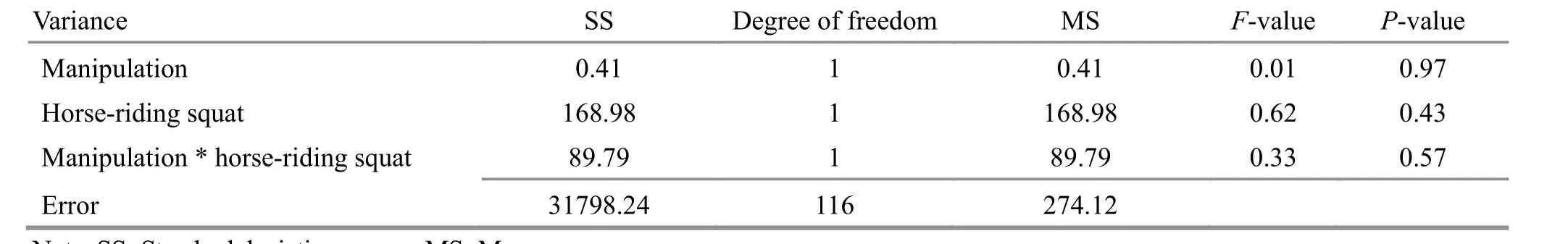
Table 19. Analysis of variance of the effects of manipulation and horse-riding squat on the extensor peak torque at 60 °/s

Table 20. Comparison of the flexor peak torque at 60 °/s

Table 21. Analysis of variance of the effects of manipulation and horse-riding squat on the flexor peak torque at 60 °/s
After treatment, the extensor peak torque at 180 °/s changed significantly in the manipulation group(P<0.05), while the changes in the other three groups were statistically insignificant (P>0.05). The betweengroup differences in the extensor peak torque at 180 °/s were statistically insignificant among the four groups(P>0.05). The details are shown in Table 22.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in changing the extensor peak torque at 180 °/s (P>0.05).Please see Table 23 for details.
After treatment, none of the four groups showed a significant change in the flexor peak torque at 180 °/s(P>0.05), and the between-group differences were statistically insignificant among the four groups (P>0.05).The details are shown in Table 24.
The main effects of manipulation and horse-riding squat and their interaction were insignificant in changing the flexor peak torque at 180 °/s (P>0.05).Please see Table 25 for details.

Table 22. Comparison of the extensor peak torque at 180 °/s
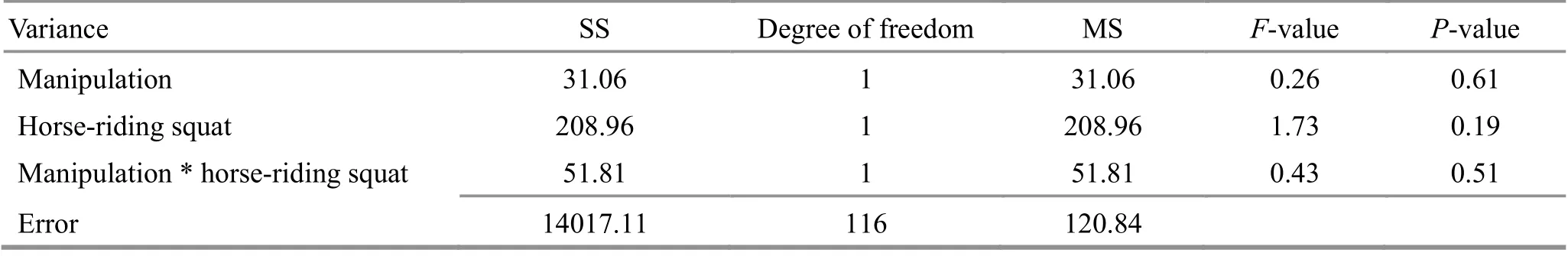
Table 23. Analysis of variance of the effects of manipulation and horse-riding squat on the extensor peak torque at 180 °/s
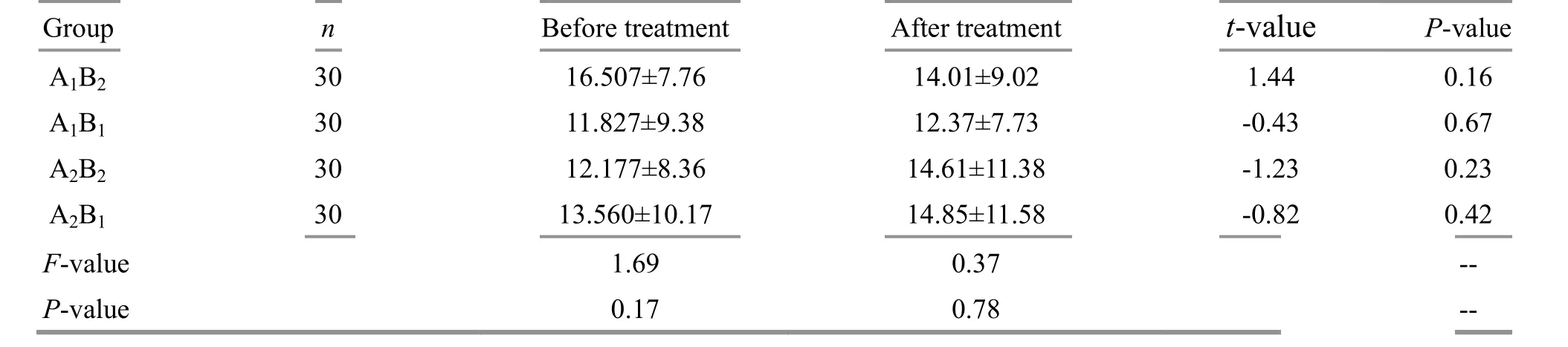
Table 24. Comparison of the flexor peak torque at 180 °/s

Table 25. Analysis of variance of the effects of manipulation and horse-riding squat on the flexor peak torque at 180 °/s
4 Discussion
This study adopted a 2×2 factorial design to observe the efficacy of Tuina and horse-riding squat in treating the early- and middle-stage KOA and the influence on the function of the knee joint. To find the optimal protocol to combine the two approaches and provide clinical evidence in treating this condition is another reason for us to conduct this research.
KOA can bring a great financial burden to the patients.According to LIU M,et al[8], the annual direct cost for osteoarthritis is 6 215.33 CNY for each person. It was reported that between January 2014 and May 2015, the annual medical cost in KOA patients was(7 184±4 890) CNY in Beijing, China, and the annual hospital visit frequency was (11.8±4.1) times[9].According to SHI F,et al[10], the economic burden for osteoarthritis patients was 0.361 billion RMB and the hospital visit was 4.97 times per person in 2007 in Shanghai, China.
Ladder treatment has been well-recognized in the treatment of KOA. In the Guideline on the Diagnosis and Treatment of Osteoarthritis stipulated by the Chinese Medical Association, patient education, exercise therapy,physical therapy, and support therapy are recommended as the first-tier treatments. For first-visit patients and mild cases, non-pharmaceutical treatment should be selected. As non-pharmaceutical treatment approaches, Tuina manipulation and horse-riding squat have been assessed as satisfactory in treating KOA by systematic reviews.
KOA belongs to the scope of knee Bi-Impediment in traditional Chinese medicine (TCM). The impediment begins from the knee and involves tendons and bones.Therefore, there is a dynamic evolution in the development of KOA from tendons to bones, yet which interact as both cause and effect, presenting as difficulty extending or flexing the joint and heaviness and weakness in the lower extremities. KOA Tendon Bi-Impediment usually manifests as cramps, flaccidity,or spasm of tendons and muscles[11]. Bone Bi-Impediment usually shows motor dysfunctions such as limited extension and flexion and blocking or catching sensations in the lower limbs. The twelve meridian muscle regions constrain bones and control joint movements to maintain the postures and motor functions within the normal range[12].
Pain is one of the major symptoms of KOA. Its pathogenesis involves both peripheral and central mechanisms. There distribute rich nerves around the attachments of capsules, tendons, and muscles.Damages to these regions will result in pain. FELSON D T,et al[13]found that bone marrow edema was closely associated with the pain in KOA, and when the edema score increased by two or move levels the pain was more likely to occur. Researchers also noticed that pain was linked to the damage to articular cartilage, and the smaller the joint space, the higher the incidence of pain[14]. The central mechanism of pain includes the sensitization of the spinal cord and dysregulation of the upper and lower pathways[15]. Tuina manipulation and Qigong exercise both can dredge and unblock meridians and collaterals, improve topical lymphatic and blood circulation of the knee joint, down-regulate the inflammatory transmitter levels [tumor necrosis factor(TNF)-α and interleukin (IL)-1β][16], inhibit heat-shock protein phosphorylation, and promote the repair of muscles[17-18]. Besides, Tuina can regulate the content of β-endorphin in the peripheral blood to cease pain[19].Our study again confirms that Tuina manipulation and horse-riding squat both can reduce pain in KOA.
QU Y J,et al[20]observed the effect of treating KOA by mainly intervening in the quadriceps femoris. The results showed that after a four-week intervention, the VAS and WOMAC scores dropped significantly,indicating that this approach can reduce pain and improve joint function. WANG K,et al[21]adopted the meridian muscle region Tuina manipulation to treat early- and middle-stage KOA. Four weeks later, the VAS and WOMAC total scores declined, suggesting that this method can help with pain, stiffness, and daily function in early- and middle-stage KOA. WANG C,et al[22]reported that after 12-week training of Tai Ji Quan, the WOMAC pain and stiffness scores declined noticeably in KOA patients, thus holding that Tai Ji Quan training can improve the lower-limb muscle strength and balance in KOA patients to mitigate the clinical symptoms.
The sitting knee-adjustment manipulation relaxes the tibiofemoral and patellar joints within the normal physiological range to push the apex of the patella and correct its route in flexion and extension. The purpose is to adjust the lower-limb line of force and distribution of mechanical load inside the knee joint, change the focus of topical stress, release knee pain, and enhance the quality of life. ZHANG H,et al[23]treated 1 000 cases of patellofemoral arthropathy with the sitting knee-adjustment approach based on the real world and found that the VAS score of the interior and exterior sides of the joint went down after the intervention,manifesting as significant relief of pain and improvement of joint range of motion.
Previously, we have found that Tuina can improve gait and isokinetic muscle strength. ZHU Q G,et al[24]also reported improvements in the walking speed, step length, and stance phase in KOA patients after Tuina treatment. GONG L,et al[25]compared the effects of Tuina manipulation on the function of knee-joint flexors and extensors with oral Fenbid. The results revealed significant improvements in the peak torques, total work, and power of flexors and extensors at 60 °/s and 180 °/s after Tuina treatment. Moreover, the ratio of flexors to extensions also exhibited a declining tendency.It is suggested that Tuina treatment is superior to oral Fenbid in ameliorating the function of both flexors and extensors. The gait analysis results in the current study are slightly different from the previous findings. There are three possible reasons. Firstly, we treated the patients with the same protocol regardless of the varus and valgus deformities. Hence, the treatment results may be affected. Secondly, the patient’s subjective improvement of walking function may result from the amelioration of the activation pattern of femoral muscles via physical stimulation, which improves the balance of coronal muscles. Nevertheless, the isokinetic muscle strength test can only target the flexors and extensors but cannot reflect the changes in medial and lateral muscles. Thirdly, the intervention period was rather short. However, gait and isokinetic muscle strength usually require a long-term intervention to show significant changes.
According to the current study, four-week manipulation plus horse-riding squat training can reduce joint pain, stiffness, and dysfunction in KOA patients. Sitting knee-adjustment plus horse-riding squat should be the optimal method for improving knee-joint stiffness. The main effects of manipulation and horse-riding squat both are significant in relieving pain. Meanwhile, the main effect of horse-riding squat training is meaningful in improving joint stiffness.
Using a factorial design, this study analyzed the efficacy of Tuina plus horse-riding squat exercise in treating KOA and the main effects and interplays to provide evidence for formulating a symptom-based treatment plan for KOA. Although we studied the main effects and interplays of manipulation and horse-riding squat training, the results need further evidence to testify. We need to read more literature to determine the frequency, duration, and intensity of horse-riding squat training in future studies. Further, we have to increase the observation times and conduct follow-ups to obtain more reliable results. Besides, a stratified randomized design based on the interferences like gender and age of the patients may also help with achieving stronger evidence.
Conflict of Interest
There is no potential conflict of interest in this article.
Acknowledgments
This work was supported by National Natural Science Foundation of China (国家自然科学基金项目, No.8197151584); Shanghai Sailing Program (上海市“科技创新行动计划”启明星培育杨帆专项, No. 22YF1444300);Three-year Development Project for Traditional Chinese Medicine of Shanghai [上海市进一步加快中医药事业发展三年行动计划, No. ZY(2018-2020)-ZWB-1001-FWB-08]; Project of Non-drug Therapy Clinical Research Center(非药物疗法临床研究中心项目); Project Within the Budget of Shanghai University of Traditional Chinese Medicine (上海中医药大学预算内项目, No. 2021LK091).
Statement of Informed Consent
The protocol and informed consent were approved by the Medical Ethics Committee of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine (Approval No.2015034). This trial was registered in Chinese Clinical Trial Registry (No. ChiCTR-INR-17011916). Informed consent was obtained from all individual participants.
Received: 3 September 2020/Accepted: 25 March 2021
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture on angiogenesis and cortical VEGF and BDNF expression in rats with focal cerebral ischemia
- Therapeutic efficacy observation of warm needling moxibustion plus Tuina for knee osteoarthritis
- Reduction of serum level of interleukin-2 and pruritus severity after acupuncture at Quchi (LI11) in hemodialysis patients: a placebo-controlled randomized clinical trial
- Acupuncture plus naloxone hydrochloride in the treatment of coma after surgery for cerebral hemorrhage: a randomized controlled trial
- Clinical observation of pediatric Tuina plus oral Chinese medication for pediatric anorexia due to spleen failing in transportation
- Therapeutic efficacy of acupuncture plus Tuina for spastic cerebral palsy and discussion of its mechanism