Therapeutic efficacy of acupuncture plus Tuina for spastic cerebral palsy and discussion of its mechanism
2022-04-18XUYan徐艳SHAOZheng邵铮YUYunyang余韵扬XIAOYao肖尧LUOYujun罗昱君YANGJin杨锦
XU Yan (徐艳), SHAO Zheng (邵铮), YU Yunyang (余韵扬), XIAO Yao (肖尧), LUO Yujun (罗昱君), YANG Jin (杨锦)
1 Department of Rehabilitation, Hubei Provincial Hospital of Traditional Chinese Medicine, Wuhan 430061, China
2 Department of Children Rehabilitation, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Edong Healthcare Group, Huangshi 435000, China
Abstract
Keywords: Acupuncture Therapy; Tuina; Massage; Cerebral Palsy; Motor Disorders; Cerebrovascular Circulation;Hemodynamics
Cerebral palsy (CP) is non-progressive brain damage due to congenital defects or acquired factors in infants.Injuries during pregnancy or delivery, premature birth,and maternal diseases are all listed as risk factors for CP[1]. Its manifestations include developmental disorders, abnormal postures, and a series of daily dysfunctions involving sensations, cognition, and communication. Some patients may even develop epilepsy or musculoskeletal diseases[2]. Spastic CP is the most common type, featured by high muscle tension,limited joint range of motion (ROM), and severe gross and fine motor dysfunctions[3-4]. To date, CP is mainly managed by combined treatments since there is no specific cure for it yet. The search for an optimal treatment protocol is still underway. This study conducted a retrospective analysis of 87 spastic CP kids to evaluate the efficacy of different treatment protocols and the effects on kids’ mental development, motor function, cerebral hemodynamics, and muscle tone.The report is summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
By referring to the diagnostic criteria for spastic CP in
ZHU Futang Practice of Pediatrics[5], we diagnosed CP following two points. The presence of motor retardation or motor dysfunction in early childhood; central paralysis caused by metabolic or degenerative diseases,and transient motor retardation in healthy kids should be excluded.
Here introduce the key points in diagnosing spastic CP.The pyramidal system was affected, and the kids showed increased muscle tension, notable spastic symptoms, and limited daily functions; increased muscle tension of the upper-limb flexors, manifesting as flexed fingers and wrists, thumbs wrapped by the contracted fists, adducted shoulders, etc.; flexed knees and hips in a lying position and difficulty raising the head in a prone position; walked in a scissor gait;tendon hyperreflexia, positive for ankle clonus test, and positive Babinski sign after 2 years old.
1.1.2 Diagnostic criteria in traditional Chinese medicine (TCM)
Referred to the syndrome differentiation criteria for CP in theGuidelines for Diagnosis and Treatment of Common Diseases of Pediatrics in Traditional Chinese Medicine[6].
1.2 Inclusion criteria
Conformed to the diagnostic criteria in Western medicine and TCM syndrome differentiation criteria mentioned above; aged between 6 months and 3 years old; with good compliance and complete medical records.
1.3 Exclusion criteria
Coupled with severe organic diseases such as congenital heart diseases, intracranial hypertension,and brain edema; motor dysfunction caused by a brain tumor or encephalitis, and genetic diseases; those with frequent epilepsies that may affect the treatment results; those with a spontaneous bleeding tendency.
1.4 Statistical methods
We adopted SPSS version 23.0 software for statistical analysis in this study. Measurement data that conformed to normal distribution and homogeneity of variance were expressed as mean ± standard deviation(±s), with the independent samplest-test used for between-group comparisons and pairedt-test for intra-group comparisons. Those not conforming to normal distribution or homogeneity of variance were processed using the non-parametric test. Enumeration data were processed by the Chi-square test. The rank-sum test was employed for the ranked data.P<0.05 was accepted as statistically significant.
1.5 General data
Eighty-seven kids with spastic CP were recruited from Hubei Provincial Hospital of Traditional Chinese Medicine between February 2019 and January 2020 for retrospective analysis. They were divided into a control group and an observation group according to their original treatment plan after the diagnosis. There were no significant differences in the general data, including gender and age, between the two groups (P>0.05),suggesting the comparability (Table 1).
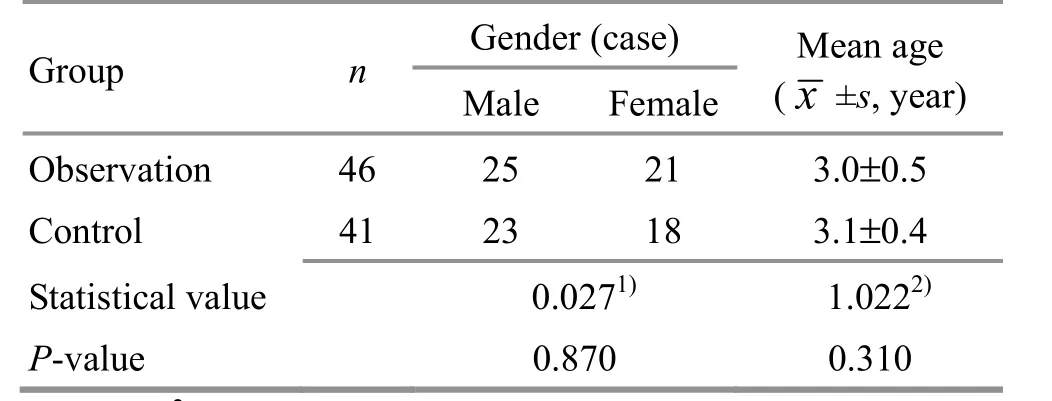
Table 1. Comparison of the general data between the two groups
2 Treatment Methods
The symptomatic treatment, motor development therapy (mainly Bobath therapy), and Tuina (Chinese therapeutic massage) treatment were offered to both groups.
2.1 Control group
2.1.1 Bobath therapy
Bobath therapy consists of two parts: constraint and facilitation. The constraint technique is mainly applied to correct abnormal postures and movement patterns.The facilitation technique is mainly used to help with keeping balance in movements or a static state and also uprightness in standing or sitting positions.
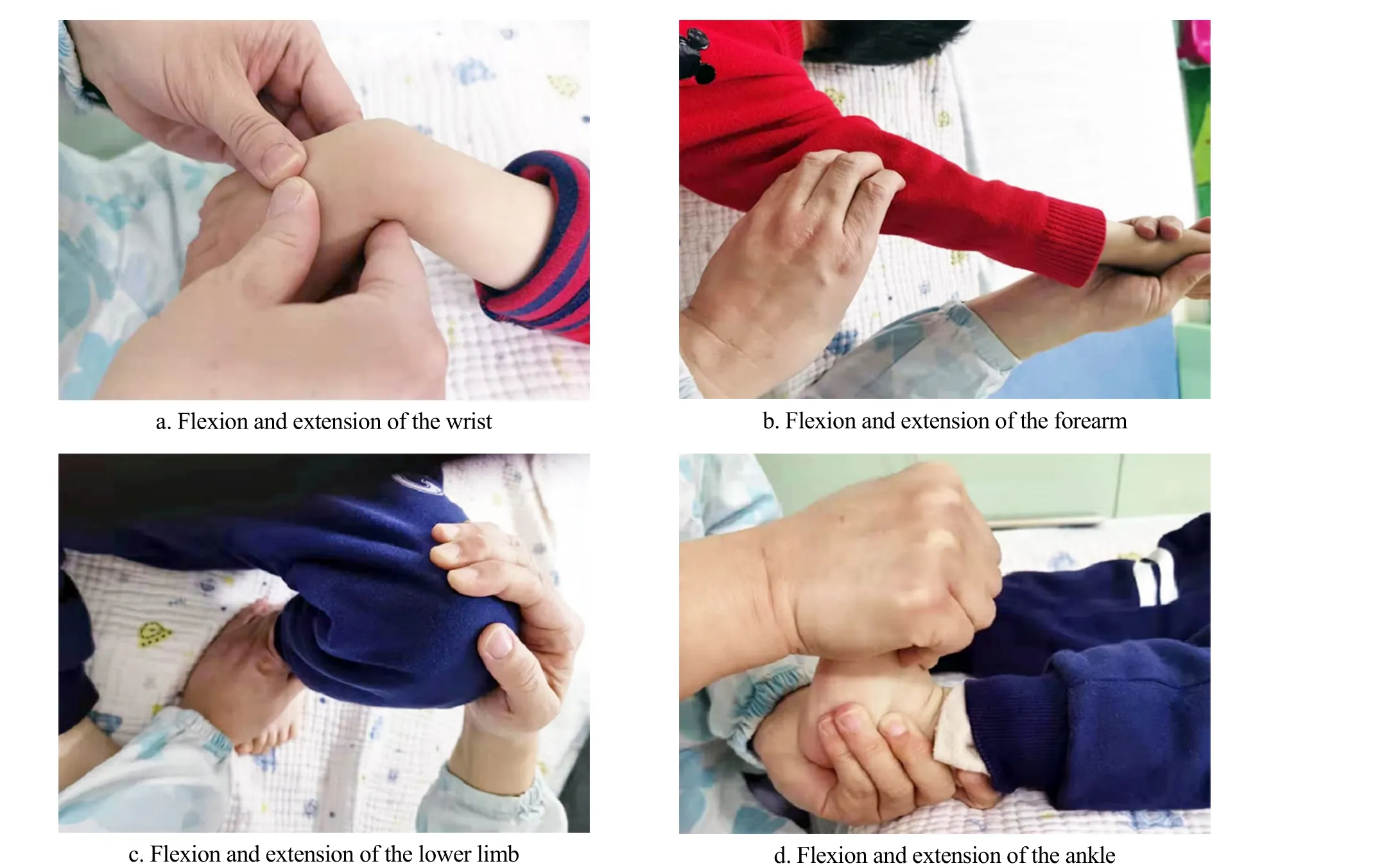
Figure 1. Bobath therapy
The kid took a supine position. The physician placed the thumbs on the kid’s dorsal wrist with the palms and the other four fingers holding the kid’s hand to help with the flexion and extension of the wrist (Figure 1a).Then the physician held and fixed the kid’s affected forearm with the left hand and lifted the affected arm with the right hand and gently tapped the biceps brachii muscle for relaxation, which was repeated 4-5 times(Figure 1b). Afterward, the physician gently tapped the abnormal lower limb to reduce muscle tension and pressed toward the tibiopatellar joint for 2-3 min(Figure 1c). Finally, the physician extended the kid’s lower limb and held the front part of the kid’s foot to fully flex the ankle joint. Strephenopodia can be treated with an opposite force for correction (Figure 1d). The treatment was performed once each day, 30 min each session.
2.1.2 Tuina treatment
The kid took a prone position. The physician Ti-Lifted and Nian-Twisted the kid’s back along the spine and applied acupressure at Ganshu (BL18), Pishu (BL20), and Shenshu (BL23), (Figure 2a). The kid then sat up to receive Dian-Digital pressing, An-Pressing, and Rou-Kneading manipulations at Fengchi (GB20), Baihui(GV20), Naohu (GV17), and Tianzhu (BL10) (Figure 2b),followed by Na-Grasping applied to the lateral lowerlimb muscle group, acupressure at Weizhong (BL40),Na-Grasping and Rou-Kneading to the upper-limb muscle groups, and acupressure at Quchi (LI11). The treatment lasted for about 15 min.
2.2 Observation group
The observation group received the same basic treatment as the control group together with acupuncture treatment.
Acupoints: Baihui (GV20), Sishencong (EX-HN1), and Shenting (GV24) for awakening orifices; Shenshu (BL23),Taixi (KI3), Yanglingquan (GB34), Zusanli (ST36), and Sanyinjiao (SP6) for unblocking the Governor Vessel.
Methods:The Hwato brand acupuncture needles(0.30 mm in diameter and 25 mm in length, Suzhou Medical Appliance Co., Ltd., China) were used. The kid took a supine position. After standard sterilization,the orifice-awakening acupoints were inserted subcutaneously backward by 0.5 Cun. The needles were retained for 30 min, during which the needles were swiftly twirled 3 times. The acupoints for unblocking the Governor Vessel were inserted perpendicularly by 0.5-0.8 Cun with even reinforcing-reducing manipulation applied after needling Qi was obtained(Deqi). The needles were removed 10 min later. The acupuncture treatment was performed once every other day, 3 times each week.
Regarding the treatments mentioned above, one month was taken as a course. The efficacy was evaluated after 6 treatment courses.
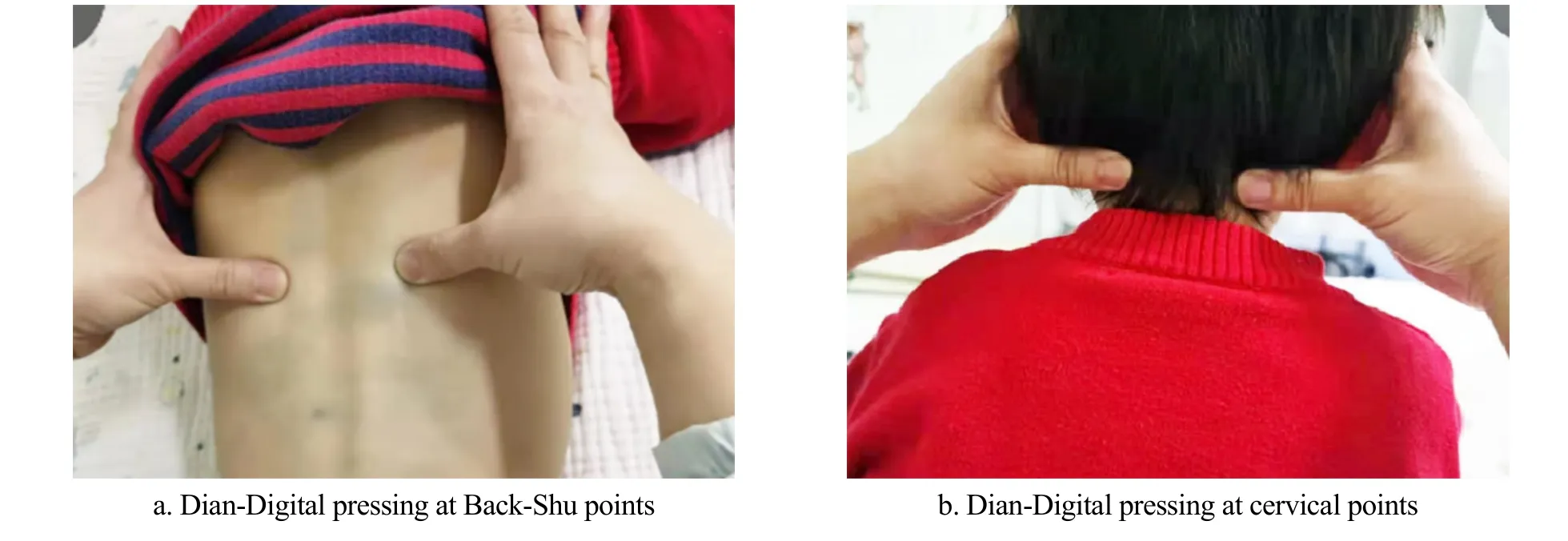
Figure 2. Tuina therapy
3 Efficacy Observation
3.1 Parameters
3.1.1 Muscle tone scoring
We used the modified Ashworth scale (MAS)[7]to assess the patients’ muscle tone before and after the intervention. MAS measures the resistance and angle of joints during passive movements, involving the joints of nine body regions: head, shoulders, elbows, wrists,fingers, thumbs, hips, knees, and ankles. The evaluation is described in a range of 0-5 points. A score of 0 point means no increase in muscle tone (no resistance during passive movements); 1 point suggests a slight increase in muscle tone (minimal resistance at the end of passive movements); 2 points suggest a mild increase in muscle tone [a catch during the first half range of motion (ROM)and slight resistance throughout the remainder of the ROM]; 3 points suggest more marked increased in muscle tone (notable resistance through most of the ROM, but movements are still available); 4 points indicate a considerable increase in muscle tone(resistance though the whole ROM and passive movements are difficult); 5 points suggest a significant increase in muscle tone (the affected parts are rigid and passive movements are rather difficult)[8].
3.1.2 Mental development
The kids’ mental development status was assessed using the scale of the Children’s Developmental Center of China (CDCC)[9]before and after the intervention. The CDCC scale consists of the mental development index(MDI) and psychomotor development index (PDI). The score is graded as follows: ≤69 points, mental retardation; 70-79 points, borderline retardation;80-89 points, below average; 90-109 points, average;110-119 points, above average; 120-129 points,eminent; ≥130 points, extremely eminent.
3.1.3 Motor function
Motor function was assessed using the Gross motor function measure (GMFM)[10]and the fine motor function measure (FMFM)[11]before and after treatment. The GMFM estimates five dimensions,including lying and rolling, sitting, crawling and kneeling,standing, and walking, running and jumping. The FMFM also estimates five dimensions, including visual movement, upper-limb joint motor function, grasping,operation, and hand-eye coordination. Each dimension is scored in a range of 0-4 points, and the final scores of GMFM and FMFM are obtained by adding the dimension scored and dividing the sum by 5. The higher the score, the better the recovery of gross and fine motor functions.
3.1.4 Cerebral hemodynamics
Before and after the intervention, the two groups of kids received transcranial Doppler test to measure the systolic velocity (Vs), mean velocity (Vm), and pulsatility index (PI) of the anterior cerebral artery (ACA), middle cerebral artery (MCA), and posterior cerebral artery(PCA).
3.1.5 Efficacy evaluation
Efficacy was evaluated based on the change in the MAS score before and after treatment.
Markedly effective: The MAS score dropped by two or more levels.Effective: The MAS score dropped by one level.Invalid: The MAS did not show significant change.
3.2 Results
3.2.1 Comparison of the muscle tone
Before treatment, there was no significant difference in the muscle tone score between the two groups(P>0.05). After treatment, the muscle tone score dropped in both groups (P<0.05) and was significantly lower in the observation group than in the control group (P<0.05), (Table 2).
3.2.2 Comparison of efficacy
The observation group obtained more significant efficacy than the control group (P<0.05), (Table 3).
3.2.3 Comparison of mental development
Before treatment, there were no significant differences in the MDI or PDI scores between the two groups (P>0.05). After treatment, the MDI and PDI scores increased in both groups (P<0.05) and were notably higher in the observation group than in the control group (P<0.05), (Table 4).
3.2.4 Comparison of motor function
Before intervention, there were no significant differences in the GMFM or FMFM scores between the two groups (P>0.05). After treatment, the GMFM and FMFM scores went up in both groups (P<0.05) and were significantly higher in the observation group than in the control group (P<0.05), (Table 5).
3.2.5 Comparison of cerebral hemodynamics
Before treatment, there were no significant differences in the Vs, Vm, or PI of the ACA, MCA, and PCA between the two groups (P>0.05). After treatment,the Vs and Vm of the ACA, MCA, and PCA increased and the PI decreased in both groups (P<0.05). Moreover, the Vs and Vm of the ACA, MCA, and PCA were markedly higher and the PI was markedly lower in the observation group than in the control group (P<0.05),(Table 6-Table 8).
Table 2. Comparison of the muscle tone score between the two groups (±s point)

Table 2. Comparison of the muscle tone score between the two groups (±s point)
Group n Before treatment After treatment t-value P-value Observation 46 3.07±0.43 1.57±0.48 15.787 <0.001 Control 41 3.15±0.39 2.16±0.40 11.347 <0.001 t-value 0.905 6.185 P-value 0.368 <0.001
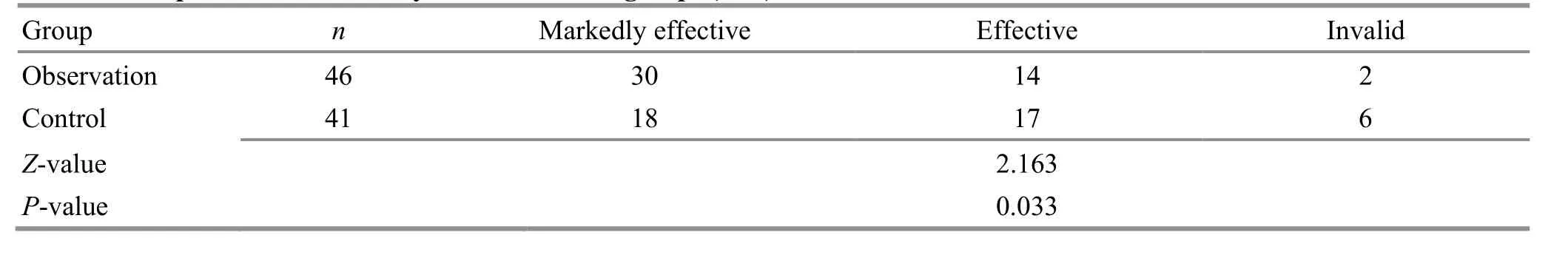
Table 3. Comparison of the efficacy between the two groups (case)
Table 4. Comparison of the mental development between the two groups (±s point)
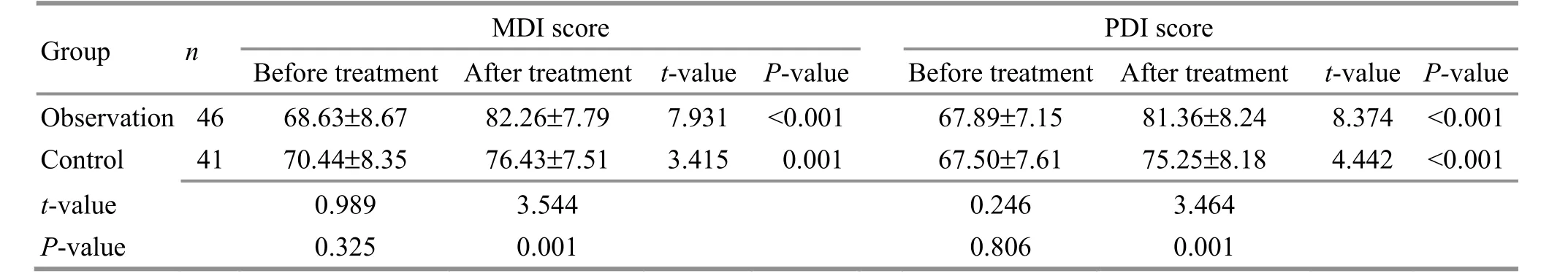
Table 4. Comparison of the mental development between the two groups (±s point)
Note: MDI=Mental development index; PDI=Psychomotor development index
Group n MDI score PDI score Before treatment After treatment t-value P-valueBefore treatment After treatment t-value P-value Observation 46 68.63±8.67 82.26±7.79 7.931 <0.00167.89±7.15 81.36±8.24 8.374 <0.001 Control 41 70.44±8.35 76.43±7.51 3.415 0.00167.50±7.61 75.25±8.18 4.442 <0.001 t-value 0.989 3.544 0.246 3.464 P-value 0.325 0.001 0.806 0.001
Table 5. Comparison of the motor function between the two groups (±s point)

Table 5. Comparison of the motor function between the two groups (±s point)
Note: GMFM=Gross motor function measure; FMFM=Fine motor function measure
Group n GMFM score FMFM score Before treatment After treatment t-value P-valueBefore treatment After treatment t-value P-value Observation 46 51.13±6.29 71.35±6.54 15.114 <0.00170.16±7.53 85.91±8.73 9.266<0.001 Control 41 49.76±6.58 60.63±6.88 7.311 <0.00169.82±7.42 77.39±8.66 4.250<0.001 t-value 0.992 7.447 0.212 4.561 P-value 0.324 <0.001 0.833 <0.001
Table 6. Comparison of the hemodynamics of the ACA (±s)
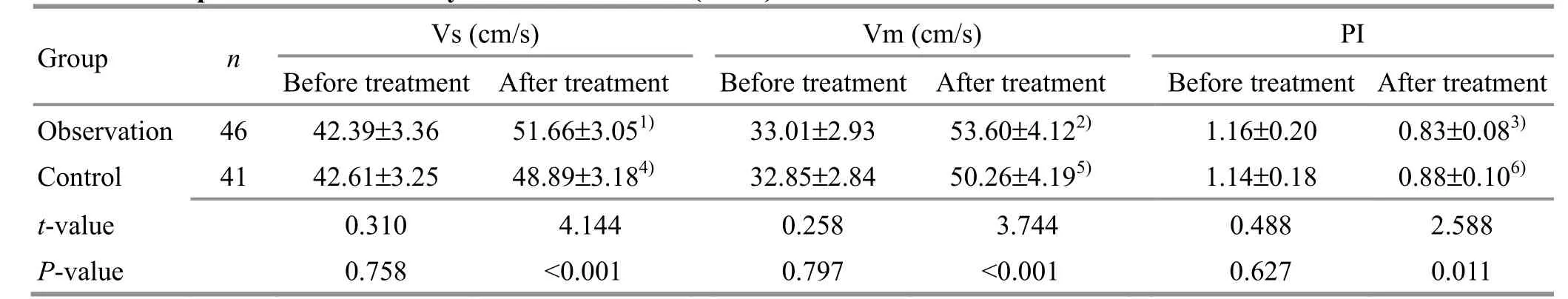
Table 6. Comparison of the hemodynamics of the ACA (±s)
Note: ACA=Anterior cerebral artery; Vs=Systolic velocity; Vm=Mean velocity; PI=Pulsatility index; compared with the same group before treatment, 1) t=13.855, P<0.001; 2) t=27.622, P<0.001; 3) t=10.674, P<0.001; 4) t=8.844, P<0.001; 5) t=22.024, P<0.001;6) t=8.018, P<0.001
Group n Vs (cm/s) Vm (cm/s) PI Before treatment After treatmentBefore treatment After treatmentBefore treatment After treatment Observation 46 42.39±3.36 51.66±3.051) 33.01±2.93 53.60±4.122) 1.16±0.20 0.83±0.083)Control 41 42.61±3.25 48.89±3.184) 32.85±2.84 50.26±4.195) 1.14±0.18 0.88±0.106)t-value 0.310 4.144 0.258 3.744 0.488 2.588 P-value 0.758 <0.001 0.797 <0.001 0.627 0.011
Table 7. Comparison of the hemodynamics of the MCA (±s)
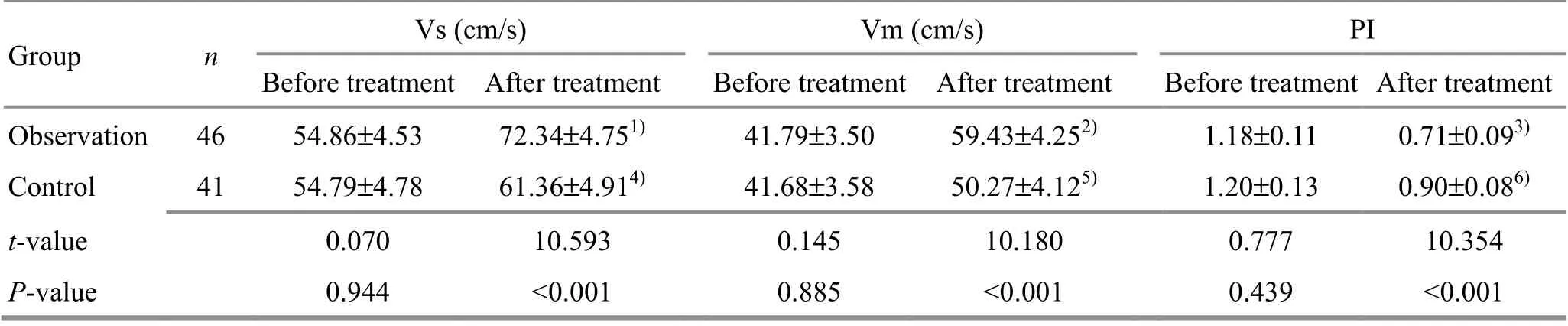
Table 7. Comparison of the hemodynamics of the MCA (±s)
Note: MCA=Middle cerebral artery; Vs=Systolic velocity; Vm=Mean velocity; PI=Pulsatility index; compared with the same group before treatment, 1) t=18.062, P<0.001; 2) t=21.730, P<0.001; 3) t=22.429, P<0.001; 4) t=6.139, P<0.001; 5) t=10.077, P<0.001;6) t=12.584, P<0.001
Group n Vs (cm/s) Vm (cm/s) PI Before treatment After treatmentBefore treatment After treatmentBefore treatment After treatment Observation 46 54.86±4.53 72.34±4.751) 41.79±3.50 59.43±4.252) 1.18±0.11 0.71±0.093)Control 41 54.79±4.78 61.36±4.914) 41.68±3.58 50.27±4.125) 1.20±0.13 0.90±0.086)t-value 0.070 10.593 0.145 10.180 0.777 10.354 P-value 0.944 <0.001 0.885 <0.001 0.439 <0.001
Table 8. Comparison of the hemodynamics of the PCA (±s)
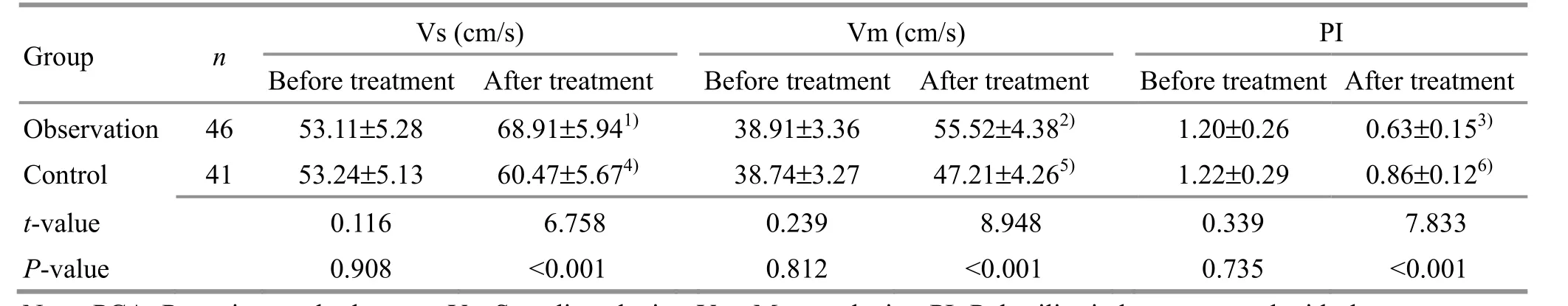
Table 8. Comparison of the hemodynamics of the PCA (±s)
Note: PCA=Posterior cerebral artery; Vs=Systolic velocity; Vm=Mean velocity; PI=Pulsatility index; compared with the same group before treatment, 1) t=13.484, P<0.001; 2) t=20.407, P<0.001; 3) t=12.879, P<0.001; 4) t=6.055, P<0.001; 5) t=10.099, P<0.001;6) t=7.345, P<0.001
Group n Vs (cm/s) Vm (cm/s) PI Before treatment After treatmentBefore treatment After treatmentBefore treatment After treatment Observation 46 53.11±5.28 68.91±5.941) 38.91±3.36 55.52±4.382) 1.20±0.26 0.63±0.153)Control 41 53.24±5.13 60.47±5.674) 38.74±3.27 47.21±4.265) 1.22±0.29 0.86±0.126)t-value 0.116 6.758 0.239 8.948 0.339 7.833 P-value 0.908 <0.001 0.812 <0.001 0.735 <0.001
4 Discussion
Spastic CP is the most common type of CP in infants,counting for 60%-70% according to the epidemiological data[12]. The pyramidal system is mainly affected in this condition. Its features include increased muscle tone,spastic limbs, limited ROM, etc. To be specific, the upper limbs usually present adducted elbows and wrists and clenched fists, and the lower limbs often show flexed knees and ankles, adducted thighs, strephenopodia or strephexopodia, and scissor gait[13]. According to modern medical research, spastic CP has complex pathogenesis, and among many factors like genetic,maternal, and neonatal factors that may cause CP,cerebral hypoxia should be the key[14]. Reperfusion in ischemic brain tissue will produce a large number of oxygen free radicals, damage the blood-brain barrier,and aggravate brain edema. Consequently, the dysplasia of brain myelin sheath, malformed central nervous system, and periventricular leukomalacia will finally cause CP[15]. A combined treatment protocol is often adopted to treat this disease, by combining exercise therapies such as Bobath and neurotrophic medications.The effectiveness of Tuina therapy has also been proved by numerous clinical trials. FANG X,et al[16]treated spastic CP with acupressure at lumbar Jiaji (EX-B2)points plus gravity posture maintenance and exercise training. They found a significant decrease in the kids’muscle tone and a notable improvement in the gross motor function after the intervention. HONG W Y,et al[17]applied Rou-Kneading, Tui-Pushing, and An-Pressing manipulations to Sishencong (EX-HN1),Weizhong (BL40), Kunlun (BL60), Taichong (LR3), Quchi(LI11), and Hegu (LI4) in treating spastic CP kids. After treatment, the kids’ mobilities of femoral angle,dorsiflexion angle, and popliteal angle increased significantly, and their muscle tone dropped. Besides Tuina therapy, acupuncture treatment can also produce satisfactory efficacy in improving mental development and motor function in CP kids.
In TCM, spastic CP can be classified into the “five retardations” or “five stiffness”. According toYi Zong Jin Jian(Golden Mirror of the Medical Tradition), “five retardations result from insufficient Qi and blood of the parents and the congenital defects, and the diseased kid is born with weak tendons and bones, difficulty walking and sitting, and slow growth of teeth, for which kidney Qi deficiency should be to blame”. The description is in line with the manifestations discovered in modern times about this disease, growth retardation, spastic limbs, and limited ROM. TCM holds that the etiology and pathogenesis involve multiple congenital and postnatal factors. The insufficiency of patients’ essence blood or maternal Qi-blood deficiency can cause congenital defects, and when tendons and bones lack nourishment palsy will occur. Improper feeding and nursing behaviors may damage the spleen and stomach or cause falls and traumatic injuries, where the interrupted production of Qi-blood and accumulated phlegm and stasis will impair the functions of Zang-Fu organs and cause malnourishment of limbs,consequently causing CP. Therefore, the treatment of CP should focus on unblocking Governor Vessel,tonifying the kidney, opening the orifices, and resolving the stasis[18-19]. In this study, a specific acupuncture method was adopted. It is based on the TCM acupoint theory and the pathogenesis of spastic CP. In this acupuncture protocol, two groups of acupoints were selected, i.e., points for awakening orifices and points for unblocking Governor Vessel. Awakening orifices is to awaken the brain, open orifices, unblock meridians and collaterals, and regulate Qi-blood, for which Baihui(GV20), Sishencong (EX-HN1), and Shenting (GV24)were selected. Baihui (GV20) is the joint of multiple meridians. Acupuncture at this point can balance Yin-Yang, supplement marrow, and benefit the brain.Sishencong (EX-HN1) can regulate the mind and benefit intelligence. Shenting (GV24) belongs to Governor Vessel and can modulate the mind and improve intelligence[20-21]. According to modern anatomy, speech areas 1, 2, and 3 are located in the speech center of the frontal lobe, parietal lobe, and temporal lobe,respectively[22]. Acupuncture stimulation to these speech areas can modulate the secretion of neurobiochemical factors and promote the growth of nerve fibers to improve neurological function and enhance mental development. TCM believes that the Governor Vessel is the joint of Yang meridians and can govern the Yang energy of the whole body. Normal running of meridian Qi and blood can boost essence blood to go up and nourish the brain. Puncturing the Governor Vessel can regulate the Yang energy of the whole body and maintain the normal flow of meridian Qi to nourish the brain and tendons to ease the symptoms. In addition, Shenshu (BL23), Taixi (KI3),Yanglingquan (GB34), Zusanli (ST36), and Sanyinjiao(SP6) are combined to tonify the spleen and kidney and activate the flow of Qi and blood. Acupuncture at Taixi(KI3) can clear heat and tonify Qi; Yanglingquan (GB34)can unblock and regulate meridians, sedate and release spasms; Zusanli (ST36) and Sanyinjiao (SP6) are essential to health care and can regulate the transportation and distribution of essence, Qi, and fluids in the body to reinforce the spleen and kidney and boost the production of Qi and blood[23].
The results of this study showed that the muscle tone score dropped in both groups after the intervention and was significantly lower in the observation group than in the control group. It is suggested that acupuncture plus motor development Tuina can produce satisfactory efficacy in reducing muscle tone, and the mechanism may be associated with acupuncture’s effects in activating the brain neural circuits, regulating nerve cell excitability, and boosting the recovery of nerve cells and brain tissue. After treatment, the GMFM and FMFM scores increased in both groups and were notably higher in the observation group than in the control group, indicating that acupuncture plus motor development Tuina can produce significant efficacy in improving gross and fine motor functions. The credit should go to Governor Vessel as it runs through the spine and enters the brain. When stimulated by acupuncture, it can unblock the pertinent three Yang meridians and activate the flow of meridian Qi to nourish the bran and promote the neurological function to coordinate motor function. In this study, the MDI and PDI scores also increased after treatment and were higher in the observation group than in the control group. It is indicated that acupuncture can produce satisfactory efficacy in improving mental development in CP kids. After the intervention, the Vs and Vm of the ACA, MCA, and PCA were notably higher and the PI was lower in the observation group than in the control group, suggesting that the effect of acupuncture in promoting mental development may be associated with the improvements of cerebral hemodynamics.
To conclude, acupuncture plus motor development Tuina can produce significant efficacy in treating infants with spastic CP. It can effectively lower muscle tone and improve mental development, motor function, and cerebral hemodynamics.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Key Innovation Plan of Science and Technology of Hubei Province (湖北省重大科技创新计划, No. 2020SY10126).
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.Received: 10 November 2020/Accepted: 29 June 2021
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture on angiogenesis and cortical VEGF and BDNF expression in rats with focal cerebral ischemia
- Therapeutic efficacy observation of warm needling moxibustion plus Tuina for knee osteoarthritis
- Reduction of serum level of interleukin-2 and pruritus severity after acupuncture at Quchi (LI11) in hemodialysis patients: a placebo-controlled randomized clinical trial
- Acupuncture plus naloxone hydrochloride in the treatment of coma after surgery for cerebral hemorrhage: a randomized controlled trial
- Clinical observation of pediatric Tuina plus oral Chinese medication for pediatric anorexia due to spleen failing in transportation
- Protocol-optimizing study of combining Tuina and horse-riding squat exercise for knee osteoarthritis
