小儿咳嗽变异性哮喘的临床特征及预后影响因素分析
2022-03-24许秀庭
许秀庭


【摘要】 目的:分析小兒咳嗽变异性哮喘(cough variant asthma,CVA)的临床特征及预后影响因素。方法:整理2015年3月-2016年3月阳江市阳东区妇幼保健院收治的117例CVA患儿的临床资料,就其临床特征、随访结果进行回顾性分析。按照患儿5年随访结果,将5年内需再次接受治疗的患儿纳入预后不良组,其余患儿纳入预后良好组,使用logistic多因素回归分析总结影响患儿预后的相关因素。结果:患儿年龄以3~6岁为主,发病季节常见于换季时、冬季,发病时间以睡前为主,常见发病诱因包括呼吸道感染、气候变化,发病先兆包括打喷嚏、流鼻涕、鼻塞,患儿饮食特点以甜食为主,69.23%的患儿有过敏史。随访期间117例患儿中,56例(47.86%)患儿再次接受以糖皮质激素为核心的针对性治疗,纳入预后不良组,其余61例(52.14%)患儿纳入预后良好组。logistic多因素回归分析示,PD20<0.5、病程≥2个月、咽后壁充血、咽后壁淋巴滤泡增生、特应性体质、家族哮喘史、随访期间呼吸道感染≥5次均为影响小儿CVA预后的独立危险因素(P<0.05)。结论:小儿CVA好发于学龄前儿童,发病季节以换季、冬季为主,症状好发于睡前,呼吸道感染、气候变化是常见诱因,发病前常有打喷嚏、流鼻涕、鼻塞等症状,好食甜食、有过敏史者更易发生CVA;PD20、病程、咽部症状、特应性体质、家族史、呼吸道感染情况与患儿预后有关。
【关键词】 咳嗽变异性哮喘 临床特征 预后 影响因素
[Abstract] Objective: To analyze the clinical characteristics and prognostic influence factors of cough variant asthma (CVA) in children. Method: The clinical data of 117 cases of children with CVA who admitted to Yangjiang Yangdong Maternal and Child Health Hospital from March 2015 to March 2016 were retrospectively analyzed on their clinical characteristics and follow-up results. According to the five-year follow-up results of children, the children who needed to be treated again within five years were included in poor prognosis group, while the others were included in good prognosis group, logistic multi-factor regression analysis was used to summarize the relevant factors affecting the prognosis of children. Result: Children were mainly aged from 3 to 6 years old, the onset season was usually in the changing season and winter, the onset time was mainly before bedtime, the common precipitating factors included respiratory tract infection and climate change, the precursors of onset included sneezing, runny nose and stuffy nose, the dietary characteristics of children were mainly sweet foods, 69.23% of children had allergic history. During the follow-up period, 56 cases (47.86%) of 117 children who received targeted therapy with glucocorticoid as the core again were included in the poor prognosis group, and the remaining 61 cases (52.14%) were included in the good prognosis group. logistic multivariate regression analysis showed that PD20<0.5, disease course ≥2 months, posterior pharyngeal congestion, proliferation of posterior pharyngeal lymphoid follicles, atopic constitution, family history of asthma and respiratory tract infection ≥5 times during follow-up were all the independent risk factors for the prognosis of CVA in children (P<0.05). Conclusion: CVA in children mostly occurs in preschool children, and the onset season is changed from season to season and in winter, the symptoms of CVA in children often occur before bedtime, respiratory tract infection and climate change are the common causes, before CVA onset, children often have symptoms such as sneezing, runny nose and stuffy nose, patients who like sweet food and have allergic history are more likely to suffer from CVA; PD20, disease course, pharyngeal symptoms, atopic constitution, family history, and respiratory tract infection are related to the prognosis of children.
[Key words] Cough variant asthma Clinical characteristics Prognosis Influence factor
First-author’s address: Yangdong Maternal and Child Health Hospital, Guangdong Province, Yangjiang 529500, China
doi:10.3969/j.issn.1674-4985.2022.03.039
咳嗽变异性哮喘(cough variant asthma,CVA)亦称过敏性咳嗽、变应性哮喘,其发病机制与典型哮喘类似,均与呼吸道慢性炎症、气道重塑及气道反应性增高有关[1]。儿童是CVA的好发群体,且近年来小儿CVA发病率呈上升趋势,加之小儿CVA临床症状不典型、易误诊或漏诊,极易因贻误治疗导致病情进展,严重时患儿可发生典型哮喘,生长发育质量面临严重威胁[2]。既往已有大量研究就小儿CVA的致病因素进行了调查,但关于CVA患儿预后影响因素的研究则较为缺乏,故此次研究就小儿CVA的临床特征、预后影响因素进行了分析,旨在提高临床对小儿CVA的认知,并指导患儿预后的预测与评估。现报道如下。
1 资料与方法
1.1 一般资料 以2015年3月-2016年3月阳江市阳东区妇幼保健院收治的117例CVA患儿为研究对象,开展回顾性分析。纳入标准:(1)年龄3~12岁。(2)明确CVA诊断,①咳嗽持续时间>4周,多于半夜和清早发生或加重,以刺激性干咳为主,无痰或仅有少量痰;②临床未见感染理化指標阳性证据;③抗哮喘药物诊断性治疗有效;④排除其他原因引发的慢性咳嗽;⑤支气管激发试验阳性和/或呼气峰值流速每日变异率≥20%(连续监测1~2周);⑥个人或一级、二级亲属有特应性疾病史,或变应原测试阳性;符合①~④即可明确诊断[3]。(3)临床资料保存完整。(4)随访时间≥5年且随访资料完成。排除标准:(1)因其他原因(上气道咳嗽综合征、支气管异物等)引发的亚急性或慢性咳嗽。(2)合并心血管、肝、肾等脏器严重病变。(3)治疗后效果判定未达痊愈,仍存在CVA症状。117例患儿中,男64例,女53例;年龄3~12岁,平均(5.57±2.23)岁。本研究已征得医院医学伦理委员会批准,并在随访时征得患儿监护人知情同意。
1.2 方法
1.2.1 临床特征研究 整理患儿基线临床资料,就其临床特征进行回顾性分析,分析内容包括年龄、发病季节、发病时间、发病诱因、发病先兆、饮食特点及过敏史。
1.2.2 预后影响因素研究 按照患儿5年随访结果,将随访期间因慢性咳嗽再次接受以糖皮质激素为核心的针对性治疗患儿纳入预后不良组,将其他患儿纳入预后良好组。对比两组基线资料,包括病程、乙酰甲胆碱累积量(PD20)、日间咳嗽积分、夜间咳嗽积分、咽后壁充血情况、咽后壁淋巴滤泡增生情况、特应性体质(合并过敏性鼻炎、过敏性咽炎、湿疹、荨麻疹、异位性皮炎等)、家族哮喘史、随访期间呼吸道感染发生情况等,将组间比较差异有统计学意义的因素纳入logistic多因素回归分析,总结影响小儿CVA预后的相关因素。
1.3 统计学处理 采用SPSS 22.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用独立样本t检验;计数资料以率(%)表示,比较采用字2检验;多因素分析采用logistic回归模型。以P<0.05为差异有统计学意义。
2 结果
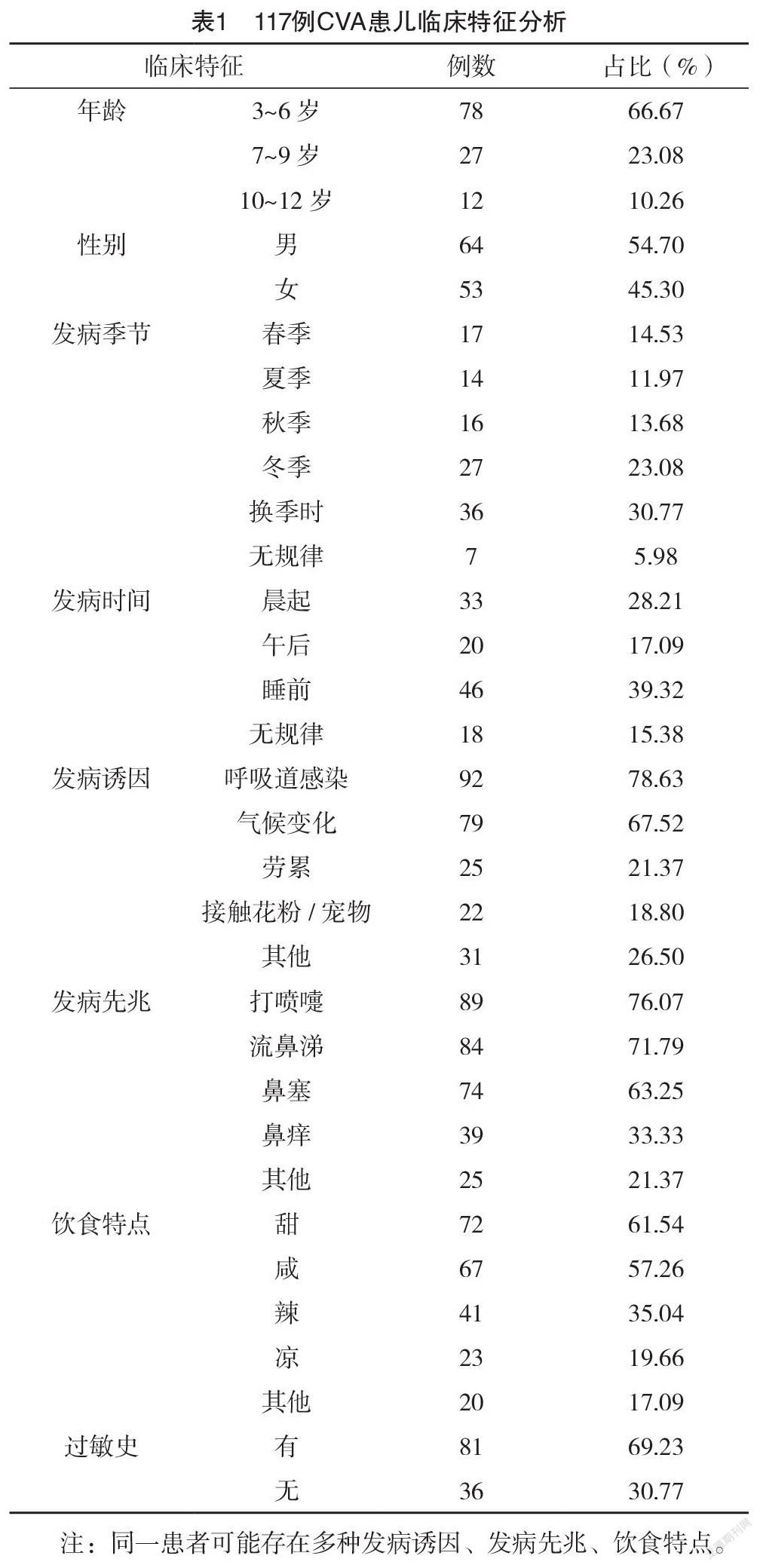
2.1 临床特征 患儿年龄以3~6岁为主,发病季节常见于换季时、冬季,发病时间以睡前为主,常见发病诱因包括呼吸道感染、气候变化,发病先兆包括打喷嚏、流鼻涕、鼻塞,患儿饮食特点以甜食为主,69.23%的患儿有过敏史,见表1。
2.2 随访结果 随访期间117例患儿中,56例(47.86%)患儿再次接受以糖皮质激素为核心的针对性治疗,纳入预后不良组,其余61例(52.14%)患儿纳入预后良好组。
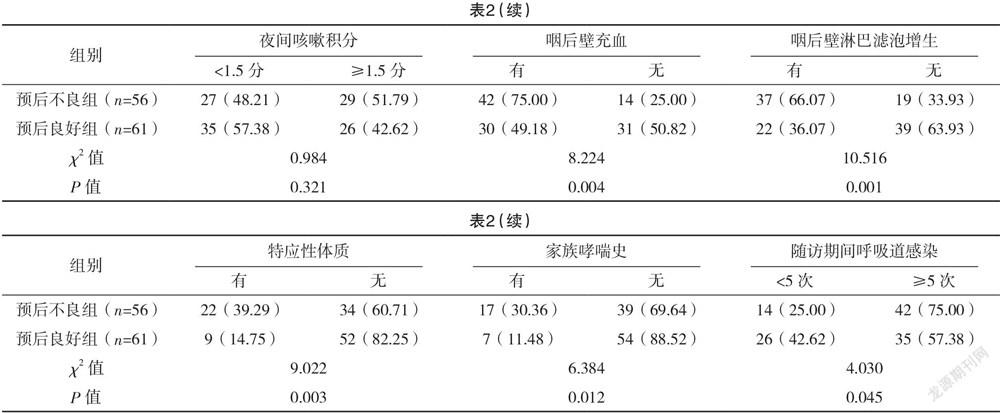
2.3 单因素分析 单因素分析示,两组PD20、病程、咽后壁充血情况、咽后壁淋巴滤泡增生情况、特应性体质、家族哮喘史、随访期间呼吸道感染情况比较,差异均有统计学意义(P<0.05),见表2。
2.4 多因素分析 以预后为应变量(预后良好=0,预后不良=1),对CVA预后的7个可能的危险因素进行赋值,PD20:≥0.5=0,<0.5=1,病程:<2个月=0,≥2个月=1,咽后壁充血:无=0,有=1,咽后壁淋巴滤泡增生:无=0,有=1,特应性体质:无=0,有=1,家族哮喘史:无=0,有=1,随访期间呼吸道感染:<5次=0,≥5次=1。logistic多因素回归分析示,PD20<0.5、病程≥2个月、咽后壁充血、咽后壁淋巴滤泡增生、特应性体质、家族哮喘史、随访期间呼吸道感染≥5次均为影响小儿CVA预后的独立危险因素(P<0.05),见表3。
3 讨论
随着我国居民生活习惯的变化,以及CVA临床认识与诊治水平的提高,近年来小儿CVA发病率与检出率均呈上升趋势[4-5],由于CVA与典型哮喘的病理学改变相似,仅在慢性炎症累及的部位、深浅存在差异,故CVA患儿若未得到及时有效的治疗,极易因气道慢性炎症持续发展、气道损伤加剧而进展至典型哮喘[6-7]。因此,近年来临床愈发重视CVA的早期诊治及预后评估。
本研究选取117例CVA患儿,首先就其临床特征进行了回顾性分析,结果显示,CVA好发于学龄前儿童且具有明显的季节性,其原因考虑与学龄前儿童气道功能、免疫功能发育不完善,且换季时、冬季更易发生呼吸道感染有关,且冷空气刺激也被认为是导致CVA的重要原因[8]。打喷嚏、流鼻涕、鼻塞是患儿常见先兆症状,上述症状与上呼吸道感染类似,应重视鉴别。同时,好食甜食的CVA患儿占比较高,可能与甜食诱发CVA或加重CVA症状有关[9]。此外,在CVA患儿中,有过敏史的患儿占比接近70%,再一次印证了CVA发病与过敏体质的密切关联。
研究表明,CVA患儿经治疗后数年内需再次接受糖皮质激素治疗者,有着更高的进展至典型哮喘风险[10],故早期评估患儿预后不良风险,对指导典型哮喘的预防有着重要意义。本研究通过logistic多因素回归分析,发现PD20<0.5、病程≥2个月、咽后壁充血、咽后壁淋巴滤泡增生、特应性体质、家族哮喘史、随访期间呼吸道感染≥5次均为影响小儿CVA预后的独立危险因素(P<0.05)。其中,PD20<0.5意味着患儿气道反应性更高,加之咽后壁充血、咽后壁淋巴滤泡增生意味着患儿病情更重,此时患儿对刺激的反应更早、更强,且气道上皮对外界刺激的敏感性更高,故其预后不良风险也随之上升,并有着更高的典型哮喘发生风险。既往研究显示,特应性体质可促使易感个体向典型哮喘发展[11],特应性体质是指机体接触环境中变应原后机体产生异常数量的特异性免疫球蛋白E(IgE),特异性IgE结合肥大细胞IgE受体并长期停留,当再次接触相同变应原后,即引发变态反应,并造成呼吸道上皮损伤、炎症介质大量释放及趋化,以及气道神经末梢敏感性上升,从而影响患儿预后。另外,家族哮喘史也使得CVA患儿治疗后典型哮喘风险上升了3.414倍,故对存在家族史的患儿,应强调重视典型哮喘的预防。
流行病学研究显示,急性呼吸道感染是诱发儿童哮喘急性发作的重要原因[12-13]。而本研究结果示,随访期间呼吸道感染≥5次的患儿,其预后不良风险上升了5.104倍,其机制可能与Th1/Th2细胞平衡向Th2细胞为主的变化有关,此时患儿过敏性疾病风险显著上升,故更易出现预后不良甚至进展为典型哮喘[14-16];此外,呼吸道感染所致痰液中性粒细胞及其溶解释放的胰肽酶E增多,也是促进和加重喘息,进而导致预后不良的重要因素[17-20]。
综上所述,小儿CVA好发于学龄前儿童,发病季节以换季、冬季为主,症状好发于睡前,呼吸道感染、气候变化是常见诱因,发病前常有打喷嚏、流鼻涕、鼻塞等症状,好食甜食、有过敏史者更易发生CVA;PD20、病程、咽部症状、特应性体质、家族史、呼吸道感染情况与患儿预后有关,应予以重视。
参考文献
[1]丁冬胜,王丽,姜勇超.咳嗽变异性哮喘病情进展与患儿血清微量元素锌、钙水平和免疫功能的关系分析[J/OL].中国医学前沿杂志(电子版),2020,12(5):131-135.
[2] FENG B W,HE C Y,LIU X Q,et al.Effect of congenital heart disease on the recurrence of cough variant asthma in children[J].BMC Cardiovascular Disorders,2021,21(1):1-9.
[3] WEI H,LI W,JIANG Z,et al.Clinical efficacy of montelukast sodium combined with budesonide or combined with loratadine in treating children with cough variant asthma and influence on inflammatory factors in the serum[J].Experimental and Therapeutic Medicine,2019,18(1):411-417.
[4]李俊丽,桑娟,苏玲.武汉某大学医院108例儿童哮喘10年随访转归分析[J].中国校医,2018,32(12):941-942.
[5] SUN W,LIU H Y.Montelukast and budesonide for childhood cough variant asthma[J].Journal of the College of Physicians and Surgeons Pakistan,2019,29(4):345-348.
[6]張洋,侯伟.儿童支气管哮喘心理行为问题研究进展[J].中国儿童保健杂志,2019,27(5):523-526.
[7] ZHANG X,MA Lianmei,LI Xiaomei,et al.Clinical Study on Montelukast in the Treatment of Pediatric Cough Variant Asthma[J].China Pharmacy,2017,28(29):4103-4106.
[8]孙静怡,房定珠,华丽,等.上海地区儿童哮喘急性发作诱因分析及哮喘患者教育[J].教育生物学杂志,2019,7(4):213.
[9] LI X,ZHU B,SHAO X.Manipulation parameter optimization in Liu’s back tuina therapy for kids’ cough variant asthma in remission stage[J].Journal of Acupuncture and Tuina Science,2020,18(1):67-74.
[10] DANG Q,ZHAO W.Influence of budesonide combined with montelukast on lung function and transforming growth factor-β1 of children with cough variant asthma[J].Drug Evaluation Research,2017,40(6):832-835.
[11]李丹,潘家华.儿童哮喘196例控制水平及影响因素分析[J].临床肺科杂志,2018,23(4):686-690.
[12]郭燕華.儿童咳嗽变异性哮喘临床治疗方案的探讨[J].中国药物与临床,2017,17(2):260-261.
[13] KHALMATOVA B T,TASHMATOVA G A,XUDOYQULOV E A,et al.Influence of Ecological Factors on the Development and Progress of Bronchial Asthma in Children[J].European Journal of Molecular & Clinical Medicine,2021,7(8):4374-4377.
[14]谢倩.孟鲁司特钠联合布地奈德治疗儿童咳嗽变异性哮喘的疗效观察[J].临床合理用药杂志,2017,10(19):89-90.
[15]张素红.儿童咳嗽变异性哮喘转为典型哮喘的相关因素研究[J].中国实用医刊,2019,46(10):75-78.
[16] GHASEMPOUR M,BILAN N.The Role of Spirometry in the Diagnosis of Cough Variant Asthma in Children Aged 5 to 15 Years[J].International Journal of Pediatrics,2017,5(12):6329-6336.
[17]卫丽,高颖,焦富勇,等.FeNO联合IgE检测对儿童咳嗽变异性哮喘的诊断价值[J].陕西医学杂志,2017,46(1):123-124.
[18]朱学龙,余国庆,张展.益生菌在儿童咳嗽变异性哮喘治疗中的作用[J].中外医学研究,2019,17(36):150-152.
[19] ENSEKI M,NUKAGA M,TADAKI H,et al.A breath sound analysis in children with cough variant asthma[J].Allergology International,2019,68(1):33-38.
[20] IMAI E,ENSEKI M,NUKAGA M,et al.A lung sound analysis in a child thought to have cough variant asthma:a case report[J].Allergology International,2018,67(1):150-152.
(收稿日期:2021-06-02) (本文编辑:程旭然)
