Surgical outcomes in inferior recurrences of rhegmatogenous retinal detachment
2021-12-17SergeyChurashovTatianaShevalovaAlexeiKulikovDmitriiMaltsev
Sergey V. Churashov, Tatiana N. Shevalova, Alexei N. Kulikov, Dmitrii S. Maltsev
Department of Ophthalmology, Military Medical Academy, St Petersburg 194044, Russia
Abstract
● KEYWORDS: rhegmatogenous retinal detachment; pars plana vitrectomy; scleral buckling; retinotomy; recurrence rate
INTRODUCTION
Rhegmatogenous retinal detachment (RRD) is a visionthreatening condition with an annual incidence rate of approximately 10 cases per 100 000[1]. Proliferative vitreoretinopathy (PVR) is the most significant cause of failure in the surgical treatment of RRD, both in primary cases and in recurrence[2-4]. Depending on the duration of the follow-up and the definition, the recurrence rate after surgical treatment of RRD varies from 5% to 37.3% and from 21.4% to 77.0%,with silicone oil (SiO) tamponade, and to 34% after removal of SiO[5-7].
Surgical treatment of inferior RRD is a significant technical and clinical challenge. SiO is lighter than water, and intraocular fluid may accumulate in the inferior quadrants of the eye fundus, enabling the progression of PVR within this space[8]. Inferior retinal breaks, therefore, are difficult to block with SiO, and RRD recurrence in these cases frequently requires some additional measures to vitreoretinal surgery,including scleral buckling (SB). SB is considered to improve outcomes in RRD recurrence; however, the results of studies are somewhat conflicting[3,9-11]. The inferior recurrence of RRD,especially when it is complicated by PVR grade C anterior,represents a challenge for the surgeon[11]. The most common causes of recurrent RRD are the reopening of retinal breaks due to persistent or progressive vitreoretinal tractions and the progression of PVR anterior[9]. So far, there is no consensus on the selection of adequate surgical options to treat the inferior recurrence of RRD. Therefore, the aim of this study was to analyze anatomical and functional outcomes in the inferior recurrence of RRD according to the surgical approach.
SUBJECTS AND METHODS
Ethical Approval The study followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee. The informed consent was obtained from the subjects.
In this study, we retrospectively analyzed electronic medical records of RRD patients who were treated in our clinic from 2010 to 2019 by two experienced vitreoretinal surgeons.
The inclusion criterion was a documented case of the inferior recurrence of RRD. In this study inferior recurrence of RRD was defined as the appearance of subretinal fluid in at least one of the inferior quadrants of the eye fundus after more than two weeks postoperatively. Exclusion criteria were incomplete data on the surgical procedure and follow-up, pneumatic retinopexy or meridional SB performed during primary surgery, traumatic retinal detachment, and primary surgical failure.
All patients received a comprehensive ophthalmic examination,including indirect ophthalmoscopy after medically induced mydriasis. Data on the extent of retinal detachment, location,and the number of retinal breaks and PVR associated changes were documented on retinal maps during the patients’ first presentation and at each recurrence.
The intraoperative techniques for each case, use of postoperative SiO tamponade or short-term postoperative tamponade with perfluorocarbon liquid (pPFCL), phakic status, PVR stage and type, as well as other possible causes (e.g., new or reopened retinal brakes) for the recurrence of RRD were analyzed.Endolaser photocoagulation was performed as a standard part of pars plana vitrectomy (PPV) and was not analyzed as an independent factor. For the classification of PVR, the updated Retina Society Classification was used. The mean duration of the short-term pPFCL tamponade was 7d.
All patients were categorized as having received either circular SB, PPV, a combination of SB+PPV, PPV with retinotomy(PPV+RT), or PPV+RT+pPFCL. For SB procedure we used round 3.5-mm silicone sponge, which was placed underneath all 4 rectus muscles over 360 degrees. RT was applied for the most challenging cases, with substantial retinal foreshortening when retina failed to be mobilized, despite extensive membrane peeling. In all cases, RT was performed as peripheral RT up to 90 degrees without retinectomy after endodiathermy, followed by accurate incision of the retina.
The patients who were able to visit the clinic were followed up monthly or were referred by the local ophthalmologist during outpatient visits if recurrence was diagnosed. The primary outcome measures were the rate of achievement of the surgical goal without the recurrence of RRD and best-corrected visual acuity (BCVA) logMAR.
Statistical Analysis Statistica 10.0 (StatSoft, Inc., Tulsa,OK, USA) was used for statistical analysis. To compare the recurrence rate of RRD in eyes with different surgical approaches, the Chi-square test was used. The Wilcoxon test was used to compare BCVA before and after surgical treatment, and the Mann-Whitney test was used to compare BCVA between the groups of different surgical treatments.The data was presented as mean±standard deviation.P<0.05 was considered to be statistically significant. For the correction of multiple comparisons between three and four surgical approaches, the Bonferroni’s correction was used.
RESULTS
First RecurrenceEighty-one eyes of 81 patients (47 males and 34 females with a mean age of 54.8±14.1y) who demonstrated inferior recurrence of RRD met the criteria for inclusion in the study. As primary surgery, SB was performed in 21 (25.9%)cases, PPV in 44 (54.4%) cases, PPV+SB in 12 (14.8%) cases,and PPV+RT in 4 (4.9%) cases. SiO tamponade was performed in 49 (60.5%) cases. Before the first RRD recurrence, 39(48.1%) eyes were pseudophakic.
Before the primary surgery, mild PVR (stage B) was diagnosed in 10 (12%) cases, advanced PVR (C posterior) in 35 (43%) cases,and advanced PVR (grade C anterior) in 36 (44.4%) cases (Table 1).Sixty-five eyes (80%) had a macula-off retinal detachment.
Recurrence of RRD was diagnosed in 41 (51%) cases at 1-3mo, in 24 (30%) cases at 4-6mo, and in 16 (20%) after 6mo.The mean time before the first recurrence was 109.0±91.0d.The mean follow-up in patients without recurrence was 15.0±6.5mo. In 49 (60%) eyes, the recurrence occurred despite SiO tamponade, including 18 cases where the redetachment occurred after SiO removal.
In patients with RRD recurrence, PVR grade C anterior was diagnosed in 71 (87.7%) eyes, of which 11 were previously treated with SB, 48 with PPV (including those with RT), and 12 with PPV+SB. New retinal breaks were found in 5 (24%),36 (75%), and 6 (50%) eyes previously treated with SB, PPV(including those with RT), and PPV+SB, respectively. The reopening of previously existing retinal breaks was diagnosed in 16 (76%), 12 (25%), and 6 (50%) eyes previously treated with SB, PPV (including those with RT), and PPV+SB (Table 2),respectively. In 73 (90%) eyes, redetachment involved the center of the macula.
Out of 81 eyes, 39 (48%) were treated with PPV, 9 (11%)with PPV+SB, 13 (16%) with PPV+RT, and 20 (25%) with PPV+RT+pPFCL (Table 3). Postoperative SiO tamponade was used in all 81 eyes.
Recurrence rate in PPV+SB group was statistically significantly lower than that of the PPV (P=0.0012), PPV+RT (P=0.028), and PPV+RT+pPFCL (P=0.047) groups. There was no statistically significant difference in preoperative or postoperative BCVA between all study groups (P>0.05; Table 4). Improvement of BCVA was not statistically significant in either group (P>0.05).

Table 1 Stages of proliferative vitreoretinopathy before primary intervention in study eyes n (%)
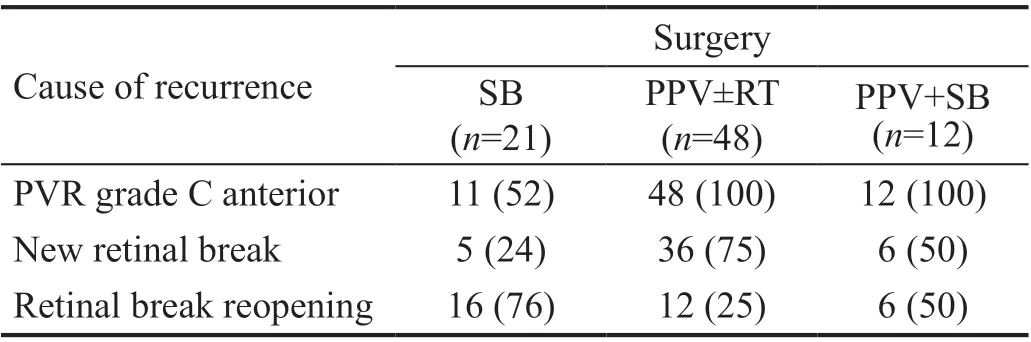
Table 2 Causes of first inferior recurrence of rhegmatogenous retinal detachment n (%)

Table 3 Surgical treatment of inferior recurrences of rhegmatogenous retinal detachment n (%)
Second Recurrence The second recurrence was diagnosed in 42 out 81 patients (52%). The mean period between previous surgery and the second recurrence was 210.0±186.6d. The mean follow-up in patients without the second recurrence was 15.0±6.5mo. In 28 (66.7%) out of 42 eyes second recurrence occurred despite SiO tamponade, including 14 eyes where redetachment was diagnosed after SiO removal. In all cases,SiO was removed not earlier than 3mo postoperatively if the retina remained attached during follow-up. PVR grade C anterior was diagnosed as the leading cause of the recurrence.Twenty eyes (47.6%) were pseudophakic at the moment of the second recurrence.
PPV+SB was performed in 9 (21.4%), PPV+RT in 15 (35.7%),and PPV+RT+pPFCL in 18 (42.9%) cases. Postoperative SiO tamponade was used in all 42 eyes. A third recurrence was diagnosed in 8 (19%) eyes.
There was no statistically significant difference in the recurrence rate between all study groups (P>0.05). However,from PPV+SB to PPV+RT and to PPV+RT+pPFCL there was a statistically significant trend towards a decrease of recurrence rate (P=0.016). There was no statistically significant difference in preoperative or postoperative BCVA between all study groups (P>0.05; Table 5). Improvement of BCVA was not statistically significant in either group (P>0.05).
DISCUSSION
In this study, we retrospectively analyzed the rates of inferior recurrences of RRD and their outcomes according to the surgical approach. We found that SB as an adjunct to PPV significantly decreases the rate of the second recurrence of RRD compared to PPV alone. Although the difference in the recurrence rate between PPV+SB and PPV+RT, with or without short-term pPFCL tamponade, was not significant,PPV+SB looks more attractive as a less complex procedure.We found no statistically significant difference between surgical approaches in the prevention of the third recurrence.However, the recurrence rate was the numerically lower in the group, which received PPV+RT+pPFCL compared to the groups which received PPV+RT or PPV+SB. Moreover, there was a statistically significant trend towards a lower recurrence rate in the group which received PPV+RT+pPFCL. All of this may indicate the potential benefits of PPV+RT+pPFCL in the surgical treatment of multiple inferior recurrences of RRD.
In our study, the progression of PVR was the main cause of inferior retinal redetachment in both second and third recurrences. From presentation to the first and second recurrence, the prevalence of PVR grade C anterior progressively increased from 45.0% to 87.7%, and to 100%,respectively, while the prevalence of PVR grade C posterior decreased from 43% to 0, respectively. This fact explains why SB alone cannot be considered as an adequate option in multiple recurrences of RRD where the retina is substantially affected by PVR. RT may be an adequate alternative for these cases. However, in inferior recurrence, RT can help to achieve better anatomical outcomes in combination with short-term postoperative PFCL tamponade.
Our results generally agree with previously reported studies. In the retrospective study of Weiet al[9], the efficacy of additional SB was compared against repeated PPV for inferior recurrence of RRD. The authors concluded that additional SB might be an early option (before 1mo) after recurrence, while in longstanding cases (1-6mo) PPV appears to be superior to SB. It seems logical to assume that if a patient undergoes several unsuccessful surgeries, the PVR will continue to progress over this period, reducing the effectiveness of SB.
Eleinenet al[12]has compared the anatomical and functional outcomes of PPV with SB as well as with RT, both of which showed similar results in detachments with inferior retinal breaks and PVR grade C. The authors conclude, therefore,that RRD with inferior retinal breaks and PVR remains a challenging situation for vitreoretinal surgeons and that choosing between the techniques is still controversial.
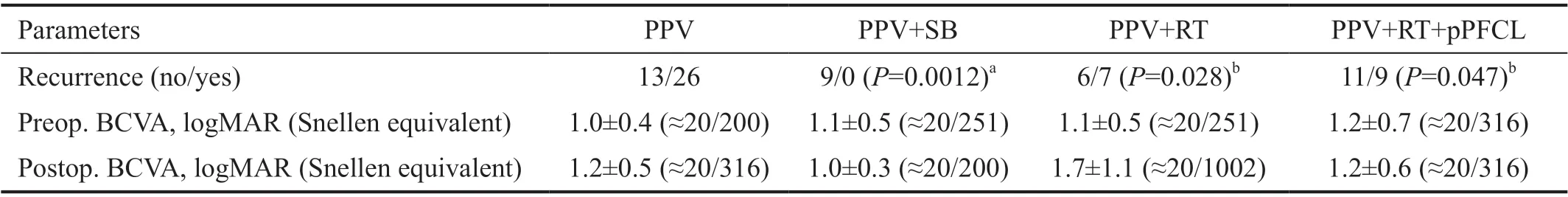
Table 4 Recurrence rate and functional outcomes after surgical treatment of first recurrence of rhegmatogenous retinal detachment
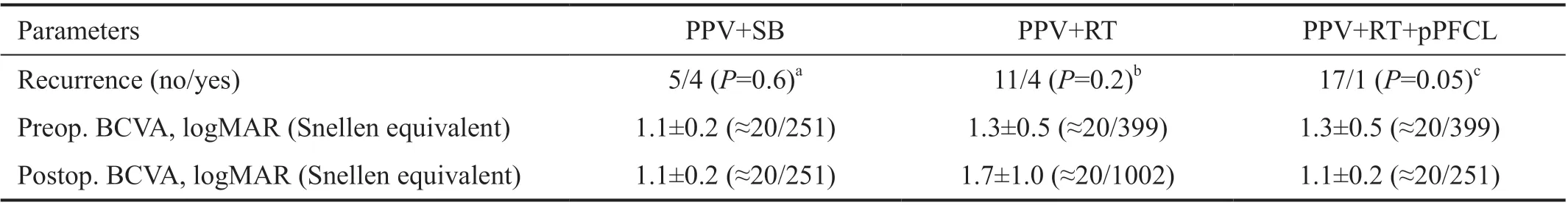
Table 5 Recurrence rate and functional outcomes after surgical treatment of second recurrence of rhegmatogenous retinal detachment
In the study of Alkinet al[13], the anatomical success rate after repeated PPV was similar after both primary PPV and SB(92.8% and 100%, respectively). However, SB showed a trend towards better anatomical outcomes and a lower reoperation rate, at least in a single recurrence. The Meta-analysis of Heet al[14]of the risk factors for the recurrence of RRD showed that SB as primary surgery reduces the recurrence rate of RRD.Alexanderet al[15]showed anatomical success rate to be as high as 95% after PPV and SB and concluded that supplementary SB improves primary success rate in inferior break detachments. However, the authors excluded cases with PVR grade C and no comparison with other techniques was performed while in our study PVR grade C was an important factor determining recurrences.
In our study, after a second recurrence, PPV+SB showed better anatomical outcomes than PPV alone and was non-inferior compared to more complex vitreoretinal techniques. SB in addition to SiO tamponade, relieves vitreoretinal tractions and enhances the effect of SiO. However, SB for inferior recurrences of RRD in combination with SiO tamponade has one disadvantage: due to the deformation of the inferior eye,which deviates from a homogenous concavity, inferior regions are difficult to tamponade effectively. PFCL can readily fill these cavities due to lower surface tension. Additionally,in inferior recurrence, a heavy SiO or PFCL may be used without SB. In a study of Caporossiet al[16], Densiron 68 showed good anatomical and functional results in the surgical treatment of inferior recurrence of RRD. However, there are substantial disadvantages with Densiron 68, including ocular hypertension in 34.7%, emulsification, and anterior uveitis in 26.5%[16]. Additionally, 2 cases of corneal opacification were described[16]. Until now, therefore, the choice of surgical approach to inferior recurrence of RRD remains debatable[17].Several studies showed that in recurrent RRD a combination of PPV with RT and SiO tamponade results in a success rate of up to 90%[18-20]. In the retrospective study of Mancinoet al[21],the success rate of PPV with inferior RT and SiO tamponade for inferior recurrence of RRD with PVR grade C posterior was also 90%. In 51 eyes with PVR grade D treated with RT over 180 degrees, the success rate was 86.3%[22]. In our study,PPV+SB and PPV+RT showed similar outcomes in the second recurrence of RRD. The success rate of RT in our study was not as high as was shown in previous studies, possibly due to the challenging nature of the cases, which experienced two recurrences. In many studies, RT showed high efficacy when performed over 180 degrees or larger[18-22]. However, we performed RT up to 90 degrees, since in our patients, retinal foreshortening was mostly local. The reduced volume of RT allows excessive retinal damage to be avoided but at the same time may be one of the explanations for the relatively poor outcomes in our study.
Short-term postoperative tamponade with PFCL in inferior recurrence of RRD with advanced PVR enables improved anatomical outcomes with the surgical goal achieved in 86%of cases[11]. Some concern exists regarding the application of PFCL beyond its intraoperative use. However, Rushet al[23]showed that it is a safe and effective option for short-term (7-17d) postoperative tamponade in cases with PVR grade C posterior and in cases with inferior or multiple breaks. Shortterm pPFCL is an effective option for the treatment of giant retinal breaks, with a success rate of 92%[24].
In our study, short-term pPFCL tamponade did not result in a statistically significant reduction of recurrence rate after the second redetachment. However, the recurrence rate in this group was numerically the lowest among all surgical techniques. Moreover, a reduction of the recurrence rate with the introduction of pPFCL was statistically significant.Therefore, the difference between surgical approaches for multiple recurrences of inferior RRD requires further studies.
The limitations of this study include the retrospective character of the data collection and the relatively long period chosen for analysis since both surgical equipment and the experience of the surgeons will have improved over this period. Additionally,not all patients were followed-up in the clinic until recurrence,and, in some cases, patients were observed by the local ophthalmologist and were only referred to the clinic after recurrence. This fact may explain relatively high mean time until the diagnosis of RRD recurrence[25]. Furthermore, since this was a retrospective study, the choice of the surgical technique was not predefined and was likely influenced by retinal findings at the time of recurrence and possibly by the personal preference of the surgeon. Finally, the comparison of the effectiveness of surgical approaches in different situations is debatable. However, it is hardly possible to divide the extremely broad variety of retinal detachment cases into comparable groups.
In conclusion, this study showed that patients with first inferior recurrence of RRD may benefit from SB as an adjunct to PPV.RT and short-term pPFCL tamponade in the second inferior recurrence may allow better anatomical outcomes, however,without substantial functional improvement.
ACKNOWLEDGEMENTS
Conflicts of Interest:Churashov SV, None; Shevalova TN,None; Kulikov AN, None; Maltsev DS, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
