Evaluation of the long-term effect of foldable capsular vitreous bodies in severe ocular rupture
2021-12-17JinDengHuPingSongRongLeZhouTaoChenJianZhouWangZhaoLiangZhu
Jin Deng, Hu-Ping Song, Rong-Le Zhou, Tao Chen, Jian-Zhou Wang, Zhao-Liang Zhu
Xi’an People’s Hospital (Xi’an Fouth Hospital), Shaanxi Eye Hospital, Affiliated Guangren Hospital, School of Medicine,Xi’an Jiaotong University, Xi’an 710004, Shaanxi Province,China
Abstract
● KEYWORDS: foldable capsular vitreous body; severe ocular rupture; long-term effect
INTRODUCTION
Ocular rupture is often complicated by severe retinal detachment, choroidal detachment, subretinal haemorrhage, and subchoroidal haemorrhage. Successful pars plana vitrectomy (PPV) surgery has enabled ophthalmologists to restore vision in a number of patients who would have previously been regarded as incurable[1]. Current vitreous substitutes, such as silicone oil, that are directly injected into eyes frequently cause intraocular toxicity. Silicone oil was recently used as an internal tamponade in PPV, but its complications were corneal degeneration, corneal endothelial decompensation, silicone oil emulsification[2-3], secondary glaucoma and other complications[4], and the material is difficult to completely remove. There is a very urgent need to find a more suitable artificial vitreous substitute for PPV surgery. Ideally, the key properties of good biomaterials must be safe and easy to remove. The clinical application of the foldable capsular vitreous body (FCVB) overcomes the complications caused by silicone oil[5-6]. Our hospital successfully implanted FCVB. We retrospectively analysed 26 patients (26 eyes), 23 males and 3 females, with severe ocular rupture who underwent FCVB implantation after PPV in Xi’an No.4 Hospital between March 2018 and September 2018.
SUBJECTS AND METHODS
Ethical Approval The study protocol followed the Declaration of Helsinki and was approved by Xi’an No.4 Hospital. Patients provided written informed consent for participation prior to study enrolment.
Study Design and Subjects We retrospectively analysed 26 patients (26 eyes) with severe ocular rupture with FCVB implantation in our hospital from March 2018 to September 2018. There were 23 males and 3 females with an average age of 36y (20-60y). Primary FCVB implantation was performed in the first PPV for 5 patients who had severe retinal defects and choroidal defects. Twenty-one patients underwent secondary FCVB implantation, and the eyes were filled with silicone oil after PPV. Thirteen of these patients had re-degeneration of the retina, and 8 patients had silicone oil-dependent eyes.Inclusion criteria: According to the international classification of mechanical ocular trauma, all open ocular trauma wounds located in zone III, with preoperative visual acuity grade IV and above. The patients or their family were informed of the FCVB implantation-related matters in detail before the surgery,and informed consent was signed.

Figure 1 Air was injected into the capsule through the drain tube valve (red arrow), the airtightness of the FCVB was checked.

Figure 2 Procedure of FCVB implantation A: The incision on the sclera was prolonged (red arrow); B. C: The three-folded FCVB was placed in the vitreous cavity (red arrow); D: Suture of the scleral incision (red arrow) and drain tube-valve system (yellow arrow); E: Silicone oil was injected into the capsule through a drain tube-valve system to support the retina; F: The fundus condition was observed under the a retinal mirror(red arrow); G: Tube ligation (red arrow) prevented silicone oil from flowing out; H: Suture of the scleral incision (red arrow), and the drain tube-valve of the FCVB was fixed onto the sclera (yellow arrow); I: Tenon’s sac and bulbar conjunctiva were sutured in layers.
All patients underwent best corrected visual acuity (BCVA),intraocular pressure (IOP), ultrawide-field fundus fluorescein angiography, and orbital CT examination before surgery, and the FCVB model was determined according to the eye axis measured by orbital CT. The postoperative follow-up time was 12mo.
Preparation and Procedure of FCVB Implantation The following surgical procedure was used for implanting the FCVB (Figures 1, 2). Patients were endotracheally intubated under general anaesthesia, the towel was disinfected. The apparatus was connected to the perfusion 3.5 mm below limbus and connected to the negative pressure system of vitreous cutter 3.5 mm above the upper limbus. Silicone oil was actively aspirated through the negative pressure system of the vitrectomy machine. The airtightness of the FCVB was checked underwater to ensure that the FCVB was intact. The incision on the sclera was prolonged and formed a 3.5×0.5 mm2L-type incision. The size of the incision on the sclera should be appropriate. It should be too large to prevent explosive suprachoroidal haemorrhage, and too small to prevent the FCVB from entering the upper ciliary body,causing ciliary body and choroidal detachment. The capsule was aspirated to a vacuum state then three-folded into a special shape, such as a spindle, to ensure that the direction of the lens surface was upward. The folded FCVB was placed in the vitreous cavity, paying attention to the preservation of the lens surface towards the anterior chamber. Silicone oil was injected into the capsule through the drain tube valve. If the position of the FCVB was tilted, a crystal adjustment hook was used to adjust it slightly. The silicone oil was injected while slowly withdrawing the perfusion to prevent the perfusion puncture of the FCVB. The fundus condition was observed. The valve of the FCVB was fixed onto the sclera, and Tenon’s sac and the bulbar conjunctiva were sutured in layers. Systemic and local anti-inflammatory and corticosteroid drugs were routinely given after surgery, prophylactic antibiotics were given intravenously, and haemostatic drugs were given for 3d.
Follow-up examinations were performed 7d and 1, 3, 6,and 12mo after surgery and included BCVA, Goldmann applanation tonometry, slit-lamp microscopy, direct ophthalmoscopy, and fundus photography. Orbital CT was also performed to determine the positioning and flexibility of the FCVB at 1, 6, and 12mo postoperatively. The patient’s subjective feelings were recorded at the same time.
RESULTS
The BCVAs at 7d and 1mo after surgery were the same as before surgery. There were 2 cases of no light perception that increased 3mo after surgery, and 2 cases were increased at 6 and 12mo after surgery. The IOP was elevated in 1 case after FCVB implantation, and it was normal after drug control.The rest of the patients had stable IOP (Table 1). There was slight conjunctival hyperaemia on day 7 after surgery. Anterior chamber haemorrhage occurred in 8 cases after surgery,and it was basically absorbed during the re-examination.Corneal oedema occurred after surgery, and most of the corneal oedema was reduced during the re-examination. At the 12-month follow-up, 3 cases of corneal degeneration and 7 cases of corneal endothelial decompensation occurred that were involved in trauma. Eight patients had shallow anterior chambers, and 14 patients developed proliferative membranes in the pupil area. Postoperative vision loss was considered due to pupillary area proliferation. All the patients with primary FCVB implantation had a severe proliferative membrane in the pupil area. Retinal reattachment was achieved in 12 cases,and the retinal condition could not be checked in 14 cases due to proliferative membrane in the pupil area. Three patients had continuous tears after surgery. Orbital CT showed that the smooth contact between the retina and capsule of the FCVB suggested that the FCVB was evenly distributed and that it supported the entire retina. The position of the FCVB was normal in all cases. Compared to the findings at the 1-, 3-, and 6-month follow-up, the corneal structures, anterior chamber depth, and retina were all stable with no apparent changes at the 12-month follow-up, which indicates that the FCVBsupported fundus was stable during the 12-month follow-up.The FCVB effectively supported the retina, controlled IOP, and had good biocompatibility (Figures 3 and 4).
Complications and Management The valve of the FCVB was exposed in 3 cases and was fixed again at thefornix conjunctiva (Table 2). Eight patients had a shallow anterior chamber during follow-up, which was stable and temporarily untreated. Fourteen cases had varying degrees of proliferative membrane in the pupil area (Figure 5).No serious complications, including retinal haemorrhage,retinal detachment, intraocular inflammation, or explosive suprachoroidal haemorrhage, were noted during the 12-month follow-up.
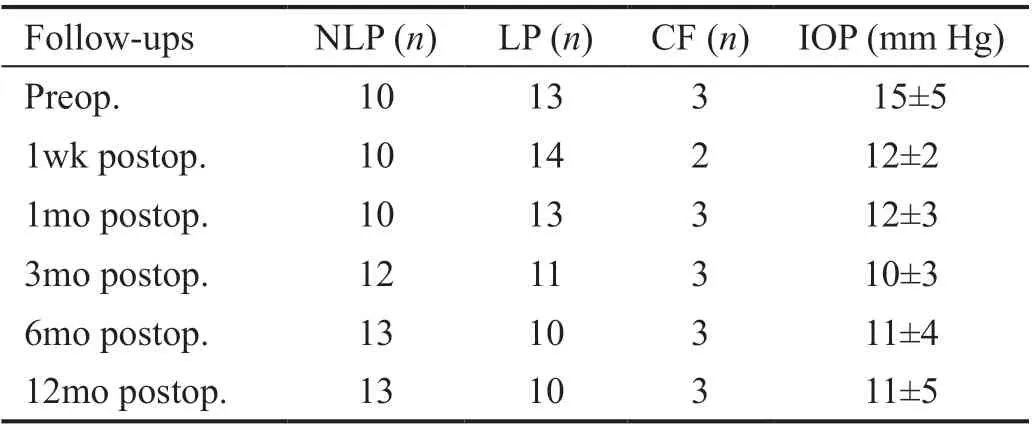
Table 1 BCVA and IOP changes in patients after surgery
DISCUSSION
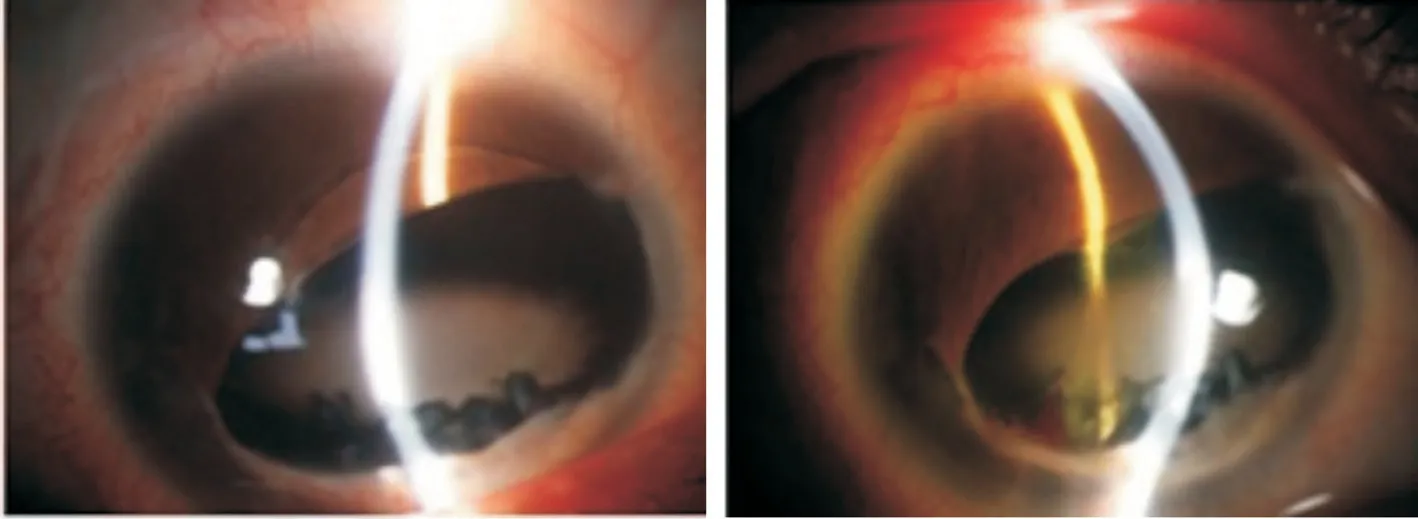
Figure 3 Slit-lamp anterior segment examination after FCVB implantation and silicone enters the anterior chamber in the silicone oildependent eyes.

Figure 4 Silicone oil enters the optic nerve in the silicone oil-dependent eyes after ocular trauma (A-C, red arrow) and slit-lamp anterior segment examination (D-E) and ultrawide-field fundus fluorescein angiography (F) after FCVB implantation.

Figure 5 Corneal degeneration and proliferative membrane in the pupil area 6mo after FCVB implantation.
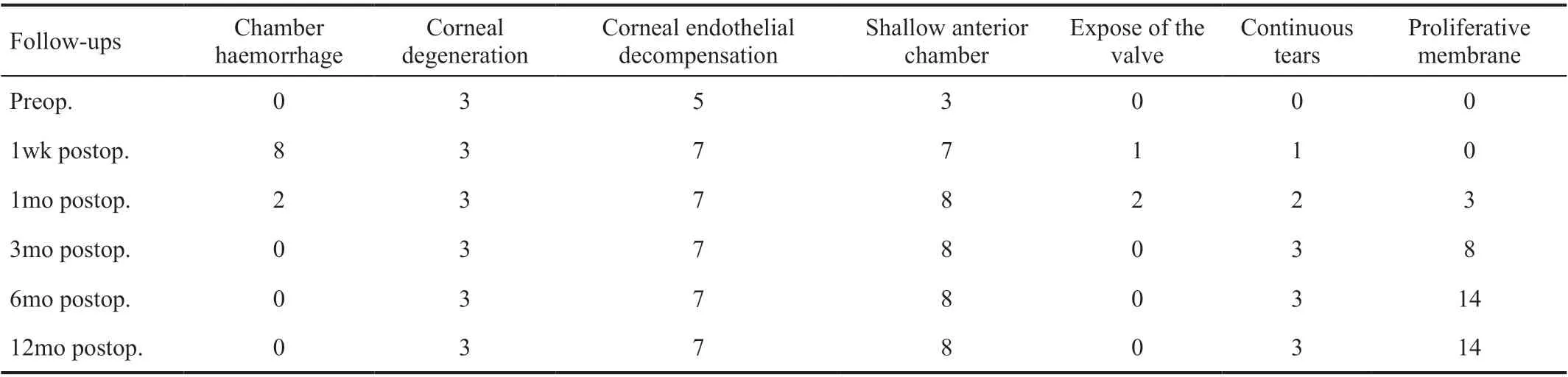
Table 2 Complications of FCVB implantation n
Severe ocular rupture seriously damages ocular tissues and visual function and causes severe trauma to the patient’s psychology and physiology. Severe ocular rupture is also a major challenge for ophthalmologists and is often associated with the loss of ocular contents, accompanied by retinal detachment or defects, subretinal haemorrhage, choroid detachment or defect, suprachoroidal haemorrhage, and detachment of the ciliary body. These factors cause visual acuity loss and no light perception[3]. In the age of ophthalmic microsurgery, eye enucleation in the primary surgery is underdeveloped. However, with the rapid development of ophthalmic microsurgery equipment and the continuous improvement of ophthalmologist medical technology, it is important for severe open eye trauma. In patients, debridement and suture of the eyeball were performed in the primary surgery, and PPV was performed in the secondary surgery.The silicone oil was used to fill the eye during the surgery to maintain the shape of the eyeballs of most patients, and some visual function was retained. However, for patients with severe ocular rupture accompanied by retinal defects and massive choroidal haemorrhage, PPV was performed.Silicon oil-filled eyes often form silicone oil-dependent eyes during surgery. Silicone oil-dependent eyes refer to trauma.The eyeball structure is severely damaged. Only long-term filling with silicone oil maintains the shape of the eyeball. If the silicone oil is removed, the eyes have a high risk of redetachment and further atrophy. However, long-term storage of silicone oil may cause a series of complications, such as corneal band degeneration, silicone oil emulsification,corneal endothelial decompensation, lens opacity, secondary glaucoma, silicone oil emulsified drops that enter ocular tissues and other complications[7]. Therefore, most scholars advocate the removal of silicone oil after 5 or 6mo. Clinically, the silicone oil in patients with silicone oil-dependent eyes cannot be removed but only replaced constantly. Therefore, there is a very urgent need to find a more suitable artificial vitreous substitute to replace silicone oil for PPV surgery[8]. Ideally, the key properties of good biomaterials must be safe and easy to remove. The emergence of FCVB solves this problem well[9-11].The clinical application of FCVB overcomes the complications caused by silicone oil. After the folded FCVB is placed in the vitreous cavity, silicone oil is injected into the capsule through the valve to restore IOP and support the retina. Because the inside of the capsule is vacuum, the silicone oil cannot contact the air, and the silicone oil does not emulsify, so it avoids the complications caused by silicone oil emulsification. In this clinical trial, retinal reattachment was successful in all cases,and no keratopathy, secondary glaucoma, silicone oil leakage,silicone oil emulsification, or any other apparent complications occurred in the follow-up period. The results demonstrated that FCVB filled with silicone oil is effective and safe in the treatment of severe ocular rupture during the 12-month follow-up.The invention of the foldable FCVB is the world’s first case.All these devices were independently researched and produced in China. The FCVB surface is transparent and uniform in colour, the light transmittance is over 90% in physiological saline or silicone oil, and it has good optical properties. The shape design of the vitreous cavity is compatible with eye tissues. The basic shape may be maintained at an IOP less than 24 mm Hg, which can contact the retina and maintain the shape and pressure of the eyeball. Previous studies showed[12-18]that FCVB implantation reduced the complications of silicone oil filling, and the IOP was normal. No corneal degeneration,corneal endothelial cell loss, secondary glaucoma, silicone oil emulsified drops into the eye tissue or other complications occurred during follow-up. The present study found that some patients may have anterior chamber haemorrhage at an early stage, which may be absorbed after the administration of drugs. A common complication was exposure of the FCVB drainage tube, which was related to the method of drainage tube fixation. The drainage tube and valve should be fixed in sections, and Tenon’s sac and the conjunctival layer should be sutured in layers to avoid postoperative displacement and exposure of the valve. Only one patient had postoperative high IOP in this study, and it was normal after the administration of IOP drugs. Some patients who had anterior chamber reactive exudation were normal after the administration of local antiinflammatory and corticosteroid drugs. The research findings are consistent with previous studies. During the follow-up period, half of the patients had different degrees of proliferative membranes in the pupil area. Although the appearance was affected, their vision was stable. FCVB implantation requires the experience of ocular trauma specialists. Postoperative patient comfort is better, and the occurrence of postoperative complications may be greatly reduced.
At present, FCVB implantation provided good treatment effects for patients with severe ocular rupture, but it is also necessary to grasp its indications and contraindications. It is suitable for patients who are 18-65 years old. Treated eye vision is less than 0.05, and ocular axial length is between 16 and 28 mm. Patients have severe retinal detachment and cannot be treated with existing vitreous substitutes, have silicone oildependent eyes, retinal insufficiency, retinal rupture caused by ocular trauma, retinal choroidal haemorrhage, retinal defects, choroidal defect, retinal detachment surgery and silicone oil filling after two retinal detachments, and retinal detachment after silicone oil removal. Contraindications:Patients with known silicone allergies and scar constitutions,endophthalmitis, uveitis, intraocular lens transparency,proliferative diabetic retinopathy, corrected visual acuity of the contralateral eye ≤0.4, history of intraocular surgery on the contralateral eye, uncontrollable other ophthalmology concomitant diseases, severe liver and kidney impairment,severe systemic system disease, preparing or pregnant or lactating women, and a history of drug abuse or alcohol abuse[19].
In the early stage, patients with severe ocular trauma often undergo eye enucleation in the primary surgery. With the development of vitrectomy, surgeons tried to keep the eyeball as much as possible in the first stage and perform vitrectomy and silicone oil filling. However, often because of serious trauma, long-term silicone oil is required, and the silicone oil is emulsified. This leads to repeated replacement of silicone oil and eventually causes eyeball shrinkage. With the advent of FCVB, patients with such severe ocular trauma undergo FCVB implant silicone oil filling surgery, which avoids the surgical operation of repeated replacement of silicone oil due to silicone oil emulsification. The advantage of FCVB is that it has good tissue compatibility, the patient has no obvious foreign body sensation, and the FCVB filled with silicone oil does not meet air, which reduce the complications caused by silicone oil emulsification and maintain the shape of the eyeball. The anterior chamber response of some patients was relatively large after implantation, but they were stable after drug treatment. Although the clinical effect of FCVB was definite, there are also certain drawbacks. Some patients had FCVB drainage tube exposure, which was greatly reduced by improvements in surgical methods. With the occurrence of this complication, some patients had a shallow anterior chamber,and some patients experienced proliferation of the anterior segment. The procedure is also expensive, and some patients will have an economic burden.
In summary, the long-term effect of FCVB for the treatment of patients with severe ocular rupture was beneficial, but the indications and contraindications must be strictly grasped,and surgery should be performed by an experienced eye trauma surgeon. The effect of secondary FCVB implantation was better than primary FCVB implantation. Long-term proliferative membrane formation in the pupil area affected the patient’s appearance. Studies showed that FCVB provides a new option for the clinical treatment of severe ocular trauma.However, the present study was a retrospective case analysis.Because a control group was not included in this study, this technique should be further explored in future studies. A larger sample size and long-term follow-up are also needed to determine its long-term efficacy.
ACKNOWLEDGEMENTS
Foundations: Supported by 2020 Shaanxi Provincial Natural Science Basic Research Program (No.2020JM-683); 2020 Scientific Research Incubation Fund of Xi’an People’s Hospital(Xi’an Fourth Hospital) (No.FZ-63).
Conflicts of Interest:Deng J, None; Song HP, None; Zhou RL, None; Chen T, None; Wang JZ, None; Zhu ZL, None.
杂志排行
International Journal of Ophthalmology的其它文章
- Upregulation of ASPP2 expression alleviates the development of proliferative vitreoretinopathy in a rat model
- Mesenchymal stem cell-derived exosomes inhibit the VEGF-A expression in human retinal vascular endothelial cells induced by high glucose
- Protective effects of umbilical cord mesenchymal stem cell exosomes in a diabetic rat model through live retinal imaging
- New technique for removal of perfluorocarbon liquid related sticky silicone oil and literature review
- Quantitative analysis of retinal vasculature in normal eyes using ultra-widefield fluorescein angiography
- Efficacy and safety of non-penetrating glaucoma surgery with phacoemulsification versus non-penetrating glaucoma surgery: a Meta-analysis
