A valve-in-valve approach to manage severe bioprosthetic tricuspid valve stenosis
2021-06-18DominikaZoltowskaNajiMaalikiBasharAlTurkAndresPinedaMaldonadoSrinivasanSattiraju
Dominika M Zoltowska✉, Naji Maaliki, Bashar Al-Turk Andres M Pineda MaldonadoSrinivasan Sattiraju
1. Cardiology, University of Florida College of Medicine-Jacksonville, Florida, USA; 2. Internal Medicine, University of Florida College of Medicine- Jacksonville, Florida, USA
Severe symptomatic tricuspid stenosis often requires intervention. When the etiology is bioprosthetic valve failure, a challenging situation is met. Surgical valve replacement is the gold standard of treatment for severe tricuspid valve (TV) disease.[1]However, a redo sternotomy is rarely performed for isolated TV disease due to very high perioperative mortality.[2]Evolving percutaneous technology presents new frontiers in treatment, with the valve-in-valve procedure emerging as an alternative. We present a case of a 65-year woman with progressive symptoms due to failure of a bioprosthetic valve in the tricuspid position who was not a surgical candidate but underwent percutaneous intervention with significant clinical improvement.
A 65-year-old woman presented to our clinic due to dyspnea (NYHA III), dizziness, weight gain, ascites, and lower extremity edema. Symptoms were progressive despite aggressive diuresis (bumex 4 mg twice a day, metolazone 5 mg a day) and a recent successful Mitral-clip procedure with septostomy closure (25 mm Cardioform device) for severe mitral regurgitation two months before presentation. She had a history of TV replacement with a 33 mm Carpentier Edwards Perimount 6 900 (Edwards Lifesciences) due to infectious endocarditis eight years earlier with related transient complete heart block requiring permanent pacemaker implantation with right ventricular lead in the coronary sinus, liver cirrhosis, and severe chronic obstructive pulmonary disease. Echocardiography showed severely calcified TV prosthesis with increased mean gradient at 9 mmHg at HR of 80 beats/min, mildmoderate tricuspid regurgitation (TR), mild residual mitral regurgitation post mitral valve repair,severely enlarged both atria, enlarged and hypokinetic right ventricle (RV), and normal left ventricular size and function (Video1_A, B). Inferior vena cava was dilated with less than 50% collapse during inspiration, suggestive of right atrial pressure of 15 mmHg. The above findings were consistent with severe stenosis of the bioprosthesis in the tricuspid position.
The patient was deemed extremely high risk for re-do sternotomy due to overall frailty and extensive comorbidity after a multidisciplinary evaluation. Nevertheless, she was found to be a suitable candidate for Edward Sapien 3-29 mm (Edwards Lifesciences) valve-in-valve placement in tricuspid position (TVIV) based on transesophageal echocardiographic measurements. The procedure was performed in the Cath Lab under general anesthesia via right femoral vein access (Video_1C). Firstly, the patient underwent TV valvuloplasty (25 mm Edwards balloon). Next, a 29 mm Sapien S3 device was positioned and deployed without rapid pacing.Post-dilation valvuloplasty was performed. The final transvalvular gradient was measured as 2 mmHg(Figure 1). Right atrial pressures improved from 23 mmHg to 16 mmHg. Transesophageal echocardiography (TEE) demonstrated no paravalvular and no valvular TR (Video_1D & E). During follow-up visits, the patient presented with improved clinical status to NYHA class II and euvolemia on exam.
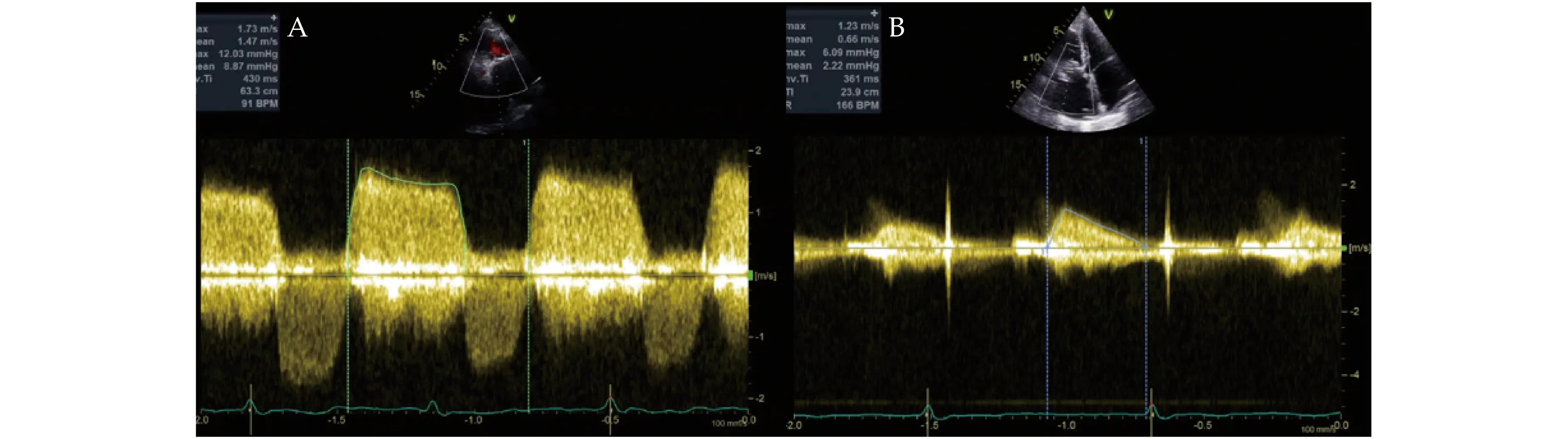
Figure 1 Tricuspid Valve Echocardiography and Doppler. Mean diastolic gradient across a tricuspid valve by continuous wave Doppler before (A), and after the procedure (B).
Tricuspid Stenosis (TS) is rare, compromising less than 1% of total valvular defects, and is often in conjunction with left-sided heart disease and tricuspid regurgitation.[3]Isolated primary TS is especially uncommon and mostly rheumatic.[1,3]Therefore, management has been challenging. Recommendations include valve intervention in patients with severe tricuspid stenosis undergoing left-sided valve surgery, or in patients with severe primary tricuspid stenosis, albeit with limited data.[1,4]Surgical valve replacement is the gold standard, while percutaneous intervention has recently evolved as a consideration in candidates with a high likelihood of success.[1,3,4]As tricuspid valve disease and its subsequent replacement seldom occur, failed valve replacement cases have posed a new treatment challenge. These patients are usually at an elevated risk for a redo sternotomy which necessitates novel percutaneous techniques.
Bioprosthetic valves have increasingly been used due to their lower risk of thrombosis but are associated with a risk of valve failure, multiple mechanisms of which exist.[5]Structural valve degeneration includes calcification, tears, flailing, or fibrosis of the implanted valve, whereas nonstructural degeneration can occur from a pannus formation. Valve endocarditis or thrombosis can also lead to prosthetic valve failure.[6]As mentioned above, these patients need new procedural techniques of correction as a redo sternotomy may not be feasible.
Expanding Transcatheter Tricuspid Valve technology offers new options for minimally invasive treatment, with new bioprosthetic valves such as Navigate, Intrepid, and Evoque, for patients with severe TV disease.[7]Nevertheless, access to them is limited beyond large academic centers, so most affected patients remain untreated.
Intervention on the tricuspid valve is relatively rarely performed, as a bioprosthesis in this position is more susceptible to failure than the analogous valve type on the left side. Edward 3 Sapien is a stented bioprosthetic valve with FDA approval for valve-in-valve procedure in high-risk patients who failed aortic and mitral bioprosthesis.[8]While the off-label use of an Edward 3 Sapien valve in the tricuspid position has limited data in the literature, reports have demonstrated considerable success. To date, the largest published study of 58 patients with NYHA III-IV undergoing Sapien TVIV procedure for dysfunctional bioprosthetic valves revealed favorable safety and efficacy profile across a wide range of valve size.[9]
For our patient, the off-label procedure was the last resort to improve her quality of life, and the decision was made after a detailed discussion between her and our Structural Heart Team. Rapid pacing is not obligatory for transcatheter valve positioning of right sided valves and was not applied in our case based on our experience. Post-procedural echocardiography displayed proper valve placement, and the patient clinically improved.
In conclusion, the presented approach can be considered as a reasonable alternative treatment for failed tricuspid bio-prosthesis in selected cases.
ACKNOWLEDGEMENTS
This case was not presented at a previous scientific meeting or journal. There were no additional contributions to this manuscript other than the ones listed.
DISCLOSURES
All authors declare that are no conflicts of interest or financial considerations, and that theyhad access to the data and a role in writing the manuscript.
AUTHOR CONTRIBUTIONS
Zoltowska D: acquisition of data, drafting of the manuscript, critical revision of the manuscript;Maaliki N: acquisition of data, drafting of the manuscript; Al-Turk B: drafting of the manuscript,critical revision of the manuscript; Maldonado A:drafting of the manuscript, critical revision of the manuscript; Sattiraju S: drafting of the manuscript,critical revision of the manuscript.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Atrial fibrillation in patients with systolic heart failure:pathophysiology mechanisms and management
- Beta-blocker treatment in heart failure patients with atrial fibrillation: challenges and perspectives
- A case series of precipitous cardiac tamponade from suspected perimyocarditis in COVID-19 patients
- Coronary artery disease presenting as intractable hiccups: an unclear mechanism
- Anticoagulation for atrial fibrillation in heart failure patients:balancing between Scylla and Charybdis
- Cardiac papillary fibroelastoma