Coronary artery disease presenting as intractable hiccups: an unclear mechanism
2021-06-18AlorSahooSarabjeetSingh
Alor Sahoo, Sarabjeet Singh,✉
1. Central Cardiology Medical Center, Bakersfield, CA, USA; 2. Central Cardiology Medical Center, Cedars-Sinai, College of Osteopathic Medicine, Touro University California, Vallejo, CA, USA
A 66-year-old gentleman presented for a cardiovascular evaluation secondary to chest discomfort, right knee pain, and intractable hiccups. The patient also had type 2 diabetes mellitus, hypercholesterolemia, aortic atherosclerosis, and ascending aortic aneurysm. His family history was also significant for premature coronary artery disease in the father. The patient had been compliant with his medical therapy, which included subcutaneous 200 units/mL insulin degludec,18 mg/3 mL subcutaneous liraglutide, daily oral 500 mg metformin hydrochloride, daily oral 100 mg sitagliptin, daily oral 12.5 mg zolpidem, daily oral 5 mg tadalafil, and 20 mg tablet rosuvastatin daily.
He was initially referred for an upper gastrointestinal(GI) endoscopy due to his persistent hiccups, but no GI etiology was found for his persistent symptoms.A cardiac stress test was conducted roughly three months after. There was no significant evidence of ischemia, though the patient complained of dyspnea(unstable angina) at the end of the exercise treadmill stress test. He underwent a transthoracic echocardiogram, which suggested a preserved ejection fraction with no other abnormalities.
Afterwards, a coronary calcium score study was immediately taken and revealed that the patient had an Agatson calcium score of 1 185, categorizing him as high risk for future cardiovascular events.
The noninvasive cardiovascular workup was inconclusive and all the other differentials considered were not suggestive of any particular etiology. Thus,we decided to do a cardiac catheterization four months after the initial consultation to confirm the patient's suspected diagnosis of occlusive coronary artery disease. The study revealed that multiple arteries were severely calcified, with the left main artery having a 10% stenosis, the left anterior descending artery (LAD) having a 99% stenosis, the circumflex artery having a 20% stenosis, and the right coronary artery (RCA) having a 30% stenosis; the initial LAD is shown in Figure 1.
The patient underwent successful revascularization with a drug eluting stent placed in the mid-segment of the LAD, the culprit lesion. This result is seen in Figure 2. Patient was discharged the same day and was followed up in the office in the same week. He was compliant with his dual antiplatelet therapy,which included 81 mg aspirin and 90 mg ticagrelor twice a day. The patient had post-interventional followups after 30 days, 6 months, and a year. The patient neither reported or nor displayed the return of intractable hiccups.
When intractable hiccups occur in hospitalized patients, digestive tract problems should be suspected, as they account for around 62.5% of clinical cases.[1]However, in our patient, the etiology was not gastrointestinal. Due to his lack of traditional symptoms associated with severe atherosclerotic plaque, cardiac catheterization was delayed.
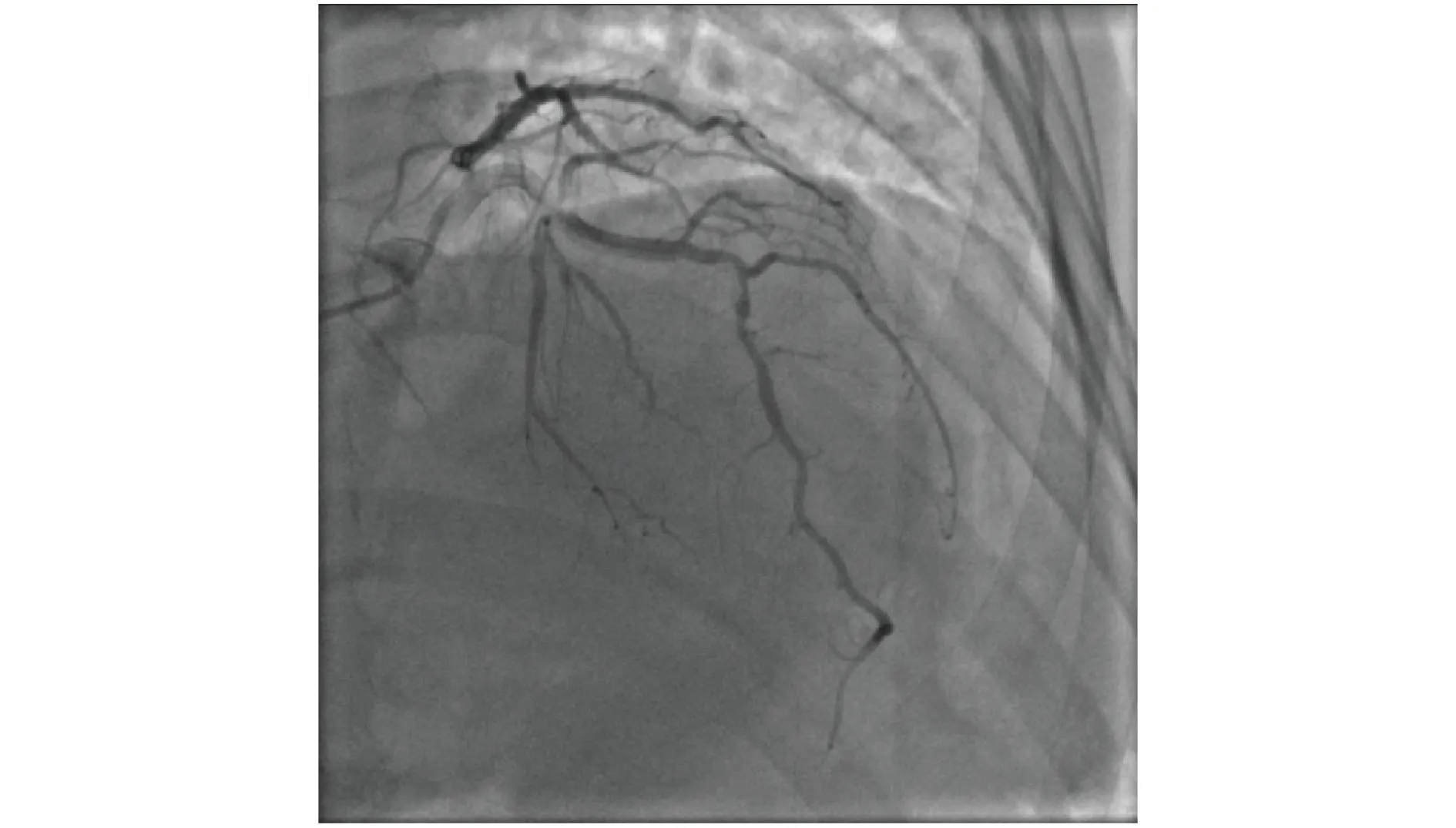
Figure 1 Pre-stent of mid-LAD. 99% stenosed, just before catheterization. LAD: left anterior descending artery.

Figure 2 Post-stent of mid-LAD. LAD: left anterior descending artery.
In our patient’s case, the computed tomography(CT) coronary calcium score of 1,185 Agatson units was an indicator of plaque deposits in the LAD and RCA primarily.
Most notably, other reports linked abnormalities of the LAD to intractable hiccups.[2]While there were multiple theories suggesting the mechanism through which this occurs, many case reports suggested that some part of the afferent limb of the reflex arc of the hiccup (phrenic, vagus, and sympathetic nerves) was affected in some way.[1]One case report suggested that occlusion of the LAD caused myocardial necrosis, which in turn disintegrated into materials that continually irritated the vagus nerve and caused persistent hiccups.[3]Since our patient had a 99% stenosis in the LAD, this theory was plausible.
Also, some case reports suggested that irritation of the phrenic nerve, which was in close proximity to the inferior wall of the heart, may have caused these persistent hiccups.[3]Others suggested a pathway involving the irritation of the vagus nerve,which supplies the pericardium.[3]Nonetheless, the exact mechanism through which hiccups are caused hasn’t been elucidated.
Such a case has not been thoroughly reported before in the literature. Many case reports on this topic focused on acute cardiac events, such as ST-elevation myocardial infarctions (STEMIs) and non-ST elevation myocardial infarctions (NSTEMIs), amongst others.[4]Of the remaining case reports that focused on myocardial ischemia as a cause of hiccups, the patient was usually accompanied by a variety of other severe symptoms that our patient did not present with.[5]Interestingly, other case reports found that when both the RCA and LAD were significantly obstructed, opening of the RCA relieved symptoms even when the LAD was still stenosed.[6]Crucially,our patient did not have an atypical stress test, unlike some other case reports.[5]
Despite the delay in intervention, cardiac catheterization of the LAD immediately resolved hiccups,and the patient has neither reported nor presented with hiccups over the long term.
We thus caution cardiologists in having a high index of suspicion when treating elderly patients with persistent hiccups who have cardiac risk factors, including but not limited to, hypercholesterolemia,type 2 diabetes, or a relevant family history.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Atrial fibrillation in patients with systolic heart failure:pathophysiology mechanisms and management
- Beta-blocker treatment in heart failure patients with atrial fibrillation: challenges and perspectives
- A case series of precipitous cardiac tamponade from suspected perimyocarditis in COVID-19 patients
- A valve-in-valve approach to manage severe bioprosthetic tricuspid valve stenosis
- Anticoagulation for atrial fibrillation in heart failure patients:balancing between Scylla and Charybdis
- Cardiac papillary fibroelastoma