Ewing sarcoma of the jejunum:A case report and literature review
2021-05-29KamleshsinghShadhuDadhijaRamlagunMungurXiaoChunPing
Kamleshsingh Shadhu,Dadhija Ramlagun-Mungur,Xiao-Chun Ping
Kamleshsingh Shadhu,Dadhija Ramlagun-Mungur,Xiao-Chun Ping,Department of General Surgery,Gastrointestinal Surgery,The First Affiliated Hospital of Nanjing Medical University,Nanjing 210029,Jiangsu Province,China
Kamleshsingh Shadhu,Dadhija Ramlagun-Mungur,Pre-registration House Officer,Medical Council of Mauritius,Floreal 0000,Plaine Whilhems,Mauritius
Abstract BACKGROUND Ewing sarcomas(ESs)are highly aggressive malignancy and are predominant in the long bones of extremities of children and young adults with a slight male predilection and rarely presents at extra skeletal locations.CASE SUMMARYA 55-year-old woman came to our hospital after finding elevated tumor biomarkers during her physical examination.Her enhanced computed tomography scan showed a jejunal mass.The patient underwent laparoscopic enterectomy.The mass was later diagnosed as ES,evidenced by fluorescence in situ hybridization whereby the GLP ES breakpoint region 1 probe was used,showing that more than 10% of the cells showed a red-green-yellow signal proving the breakpoint rearrangement of the ES breakpoint region 1 gene in chromosome 22.CONCLUSION We describe a case of localized ES at the jejunum in China based on the literature.
Key Words:Ewing sarcoma;Small bowel;Fluorescence in situ hybridization;Ewing sarcoma breakpoint region 1 gene;Jejunum;Enterectomy;Case report
INTRODUCTION
Ewing sarcoma(ES)is a small round-cell tumor with simple sarcoma-specific genetic alterations resulting in a TET/FET family member and E26 transformation-specific family member[1].ESs are rare small round-cell tumors that arise predominantly in children and young adults with a slight male predilection[2-4].ES most often arises in the mid-shaft or diaphysis of the long bones of the extremities with the spine making up 8% of the primary sites[5].Extra osseous ES occurs in the soft tissue of the extremities,paravertebral region,and pelvic cavity[6] and has also been discovered in most organs including the pancreas,liver,adrenal gland,esophagus,and uterus[7-13].Extra skeletal cases are rare,and these patients generally present at an older age and demonstrate a greater overall 5-year survival than skeletal ES tumors[14,15].Reports of primary liver involvement have been noted,as well as gastrointestinal sites of origin including the stomach,small intestine,and colorectal[16-19].Nevertheless,ES is extremely rare in the small bowel.Here,we report a case of primary ES in the jejunum with EWS rearrangement.
CASE PRESENTATION
Chief complaints
A 55-year-old otherwise healthy female patient came to our hospital after finding out that she had elevated tumor biomarkers during her annual physical examination.
History of present illness
She had no other complaints.Her sleep and appetite were normal.Her excretion and egestion were all normal.
History of past illness
The patient had a free past medical history.
Personal and family history
The patient grew up in her locality,denies any contact with contaminated water or radiation exposure,and denies smoking and alcohol consumption.She had a gestational history of 1-0-0-1.Her menstruation was 16(5-6/28-30)50.
Physical examination
On examination,the patient’s temperature was 37.0 °C,heart rate was 85 beats per min,respiratory rate was 16 breaths per min,and blood pressure was 110/65 mmHg.The Glasgow coma scale was 15/15 without any pathological signs.Her S1 S2 sounds were regular.Her chest was bilaterally clear;no rhonchi or crackles were heard.Abdominal examination revealed a soft and non-tender abdomen.No mass or distension was observed.Bowel sounds were active.
Laboratory examinations
Her carbohydrate antigen 153(CA-153)level was 38.04 u/mL,CA-199 was 109.5 u/mL,and CA-125 47 was u/mL.The white blood cell count was low at 3.39 × 109/L(normal range 3.50-9.50 × 109/L)and lymphocytes were low at 0.79 × 109/L(normal range 1.10-3.20 × 109/L).
Imaging examinations
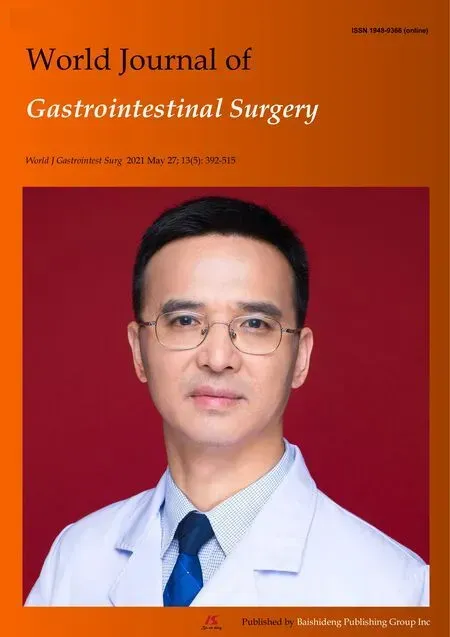
Her abdominal computed tomography scan showed a contrast-enhanced mass in the small intestine at the left lower quadrant of the abdomen(Figure 1).
Further diagnostic work-up
The patient underwent minimally invasive exploratory laparotomy.During the exploration,the tumor was located in the distal jejunum.It was well-circumscribed and had a fleshy pink surface similar to that of a gastrointestinal stromal tumor.A segment of the jejunum was resected 5 cm away from the edges of the tumor on both sides and an anastomosis was made using mechanical staple.The patient recovered uneventfully after surgery.
Pathological report
Pathological examination showed that the tumor of 3.5 cm × 3.0 cm × 2.3 cm in size was malignant,as there was invasion of the entire wall of the intestine.The resected sample had negative margins(R0)(Figure 2).Immunohistochemical analysis showed CD117(-),CD34(-),DOG-1(-),Ki67(35%),CK-pan(partly +),CK-L(+),CD56(-),Syn(+),Villin(-),CK7(-),Cg A(-),CD99(+ +),INI-1(+),Desmin(-),Inhibin-α(-),ER(-),PR(-),Calretinin(-),WT-1(-),SF(-),HMB45(-),S-100(-),and Melan A(-).Fluorescence in situ hybridization(FISH)for an ES breakpoint region 1(EWSR1)gene rearrangement(22q11)was performed using GLP EWSR1 probe,showed that more than 10% of the cells had a red-green-yellow signal,demonstrating the breakpoint rearrangement of the EWSR1 gene in chromosome 22(Figure 3).
Post-operative course
Post-operatively,bone X-rays were done to rule out any primary lesion from her skeletal system(Figure 4).The patient was discharged on post-operative day 8.
Further work and follow-up
She was referred to the oncology department for further treatment.The regimen included vincristine,adriamycin,cyclophosphamide,doxorubicin,and addition of ifosfamide and etoposide(VACD-IE),given every 2 wk for 12 cycles.It started 1 mo post-operatively.However,after four cycles,the patient stopped the adjuvant therapy due to a fear of side effects.To date,there has been no sign of relapse and the patient recently showed interest in continuing the adjuvant therapy.
FINAL DIAGNOSIS
Extraosseous ES at the jejunum.
TREATMENT
Minimally invasive exploratory laparotomy.Referred to the oncology department for further treatment.The regimen included VACD-IE,given every 2 wk for 12 cycles.It started 1 mo post-operatively.
OUTCOME AND FOLLOW-UP
After four cycles,the patient stopped the adjuvant therapy due to a fear of side effects.To date,there is no sign of relapse and the patient recently showed interest in continuing the adjuvant therapy.
DISCUSSION
Figure 1 Transverse spiral computed tomography scan of the abdomen,with intravenous contrast enhancement showing dilation of jejunal wall of the left lower quadrant.

Figure 2 Immunohistochemical analysis.A:Low magnification of the resected sample using formalin-fixed(magnification:× 40);B:Paraffin-embedded sections of tumor stained with hematoxylin and eosin demonstrating sheets of small(magnification:× 100);C:Round-to-spindle,uniform tumor cells with clear cytoplasm(magnification:× 200);D:Higher magnification of C(magnification:× 200).
ES harbors multiple balanced translocations,and fusions involving the EWSR1 gene on chromosome 22 exist.The most common translocation is t(11;22),EWSR1-FLI1 fusion(85% of cases),causing overexpression of the FLI-1 protein.The second most common translocation is t(21;22),EWSR1-ERG fusion(5%-10% of cases).Numerous other less common variant translocations exist.Lack of reverse transcriptionpolymerase chain reaction fusion transcripts for EWSR1-FLI1 and EWSR1-ERG does not exclude the possibility of ES because it does not rule out fusion transcripts that may be present below the limit of detection for the given assay(5%)[20].It most commonly arises from bone but can develop in extra skeletal sites[21].ES of the small intestine is extremely rare based on the literature[22-24].
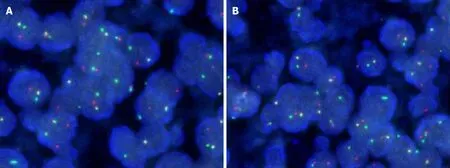
Figure 3 Fluorescence in situ hybridization.A:Fluorescence in situ hybridization of the resected tumor showing more than 10% of the cells showed a redgreen-yellow signal,proving the breakpoint rearrangement of the Ewing Sarcoma breakpoint region 1 gene;B:More than 10% of the cells from resected sample showing a red-green-yellow signal(magnification:× 200).
Malignant GIST usually expresses CD117,Dog-1,and CD34,which were all negative in this case.Although both synovial sarcoma and ES/PNET could have genetic rearrangements,the regions of these translocations are quite different.In ES/PNET,Chr22 EWS-FLI or EWS-FEV translocations are commonly reported[25].However,in synovial sarcoma,SYT-SSX translocation is frequently observed[26].Clear-cell sarcoma could be ruled out by negative immunohistochemistry for HMB45,S-100,and Melan A.A previous study also indicated the necessity of distinguishing from an intraabdominal desmoplastic small round-cell tumor by histological and immunohistochemical characteristics when ES/PNET occurs in the abdominal cavity[27].
Among the 37 cases found,3 were derived from the esophagus,9 from the stomach,5 were of colorectal origin and 20 arose from the small intestine.Twenty-two cases were in males and fifteen were in females.The age range was 9-years-old to 68-yearsold.FISH break-apart EWSR1 was positive in 19 cases,negative in 1 case and was not conducted in 17 cases[9,18,22,23,28-51].Our patient’s characteristics fell within these demographic data.Demographic research has shown that the frequency of EW is higher in United States Caucasian population than in China[52].
ES predominantly affects children and young adults with a peak incidence between 10 and 20 years of age.About 30% of cases occur in adults over the age of 20 and fewer than 5% occur in adults over the age of 40[53].
to date,the outcome of the 5-year survival rate of metastatic patients is usually poor(< 30%)compared to localized ES(65%-75%),despite the use of chemotherapy[54].Several studies have indicated that localized extra skeletal ES has a more favorable outcome than skeletal tumors[55,56].
According to National Comprehensive Cancer Network guidelines,postoperative radiation therapy should begin within 60 d of surgery and is given concurrently with consolidation chemotherapy[57].This explains why our patient was referred to oncology department shortly after surgery for further treatments.
Intergroup Ewing’s Sarcoma Study-I and Intergroup Ewing’s Sarcoma Study-II showed that radiation therapy and chemotherapy with VACD was superior to vincristine,adriamycin,cyclophosphamide(VAC)[58].The 5-year relapse-free survival rate was 60% and 24 % for VACD and VAC,respectively(P < 0.001).The corresponding overall survival rate was 65% and 28%(P < 0.001).Womer et al[59] reported that VACD-IE given on every 2 wk schedule was found to be more effective and no increase in toxicity.
CONCLUSION
ES is a highly aggressive small round-cell tumor that arises in adults.We have described a patient with ES occurring in the jejunum.This case report helps solidify jejunum as a potential site for ES origin and surgical approach with adjuvant chemotherapy does prove beneficial.However,this is a single case study and conclusion be made only based on our experience.

Figure 4 Post-operative bone X-ray which shows no lesion in skeletal system thereby excluding metastasis.A:Anterior-posterior view of the chest;B:Posterior-anterior right upper thigh;C:Posterior-anterior left upper thigh;D:Anterior-posterior right upper thigh;E:Anterior-posterior left upper thigh;F:Anterior-posterior lower leg;G:Anterior-posterior lower leg;H:Medial-lateral lower leg;I:Medial-lateral lower leg.
ACKNOWLEDGEMENTS
We’d like to thank Dr.Ding ZY for the radiological images and Dr.Fang HS for processing the pathological images.
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Biliary drainage in inoperable malignant biliary distal obstruction:A systematic review and meta-analysis
- Liver resection for hepatocellular carcinoma larger than 10 cm:A multi-institution long-term observational study
- Comparison of effects of six main gastrectomy procedures on patients’ quality of life assessed by Postgastrectomy Syndrome Assessment Scale-45
- Practices concerning sleeve gastrectomy in Turkey:A survey of surgeons
- Therapeutic effects of the TST36 stapler on rectocele combined with internal rectal prolapse
- Could neoadjuvant chemotherapy increase postoperative complication risk of laparoscopic total gastrectomy?A monoinstitutional propensity score-matched study in China