Digestive system involvement of infections with SARS-CoV-2 and other coronaviruses: Clinical manifestations and potential mechanisms
2021-04-13GaoFengZhanYueWangNingYangAiLinLuoShiYongLi
Gao-Feng Zhan, Yue Wang, Ning Yang, Ai-Lin Luo, Shi-Yong Li
Abstract Although coronavirus (CoV) infection is often characterized by respiratory symptoms, the virus can also result in extrapulmonary symptoms, especially the symptoms related to the digestive system. The outbreak of coronavirus disease 2019 (COVID-19) is currently the world’s most pressing public health threat and has a significant impact on civil societies and the global economy. The occurrence of digestive symptoms in patients with COVID-19 is closely related to the development and prognosis of the disease. Moreover, thus far, there are no specific antiviral drug or vaccine approved for the treatment or prevention of COVID-19. Therefore, we elaborate on the effects of CoVs on the digestive system and the potential underlying mechanisms.
Key Words: SARS-CoV-2; Gastrointestinal diseases; Liver dysfunction; COVID-19;Coronavirus; Mechanisms
INTRODUCTION
In December 2019, an outbreak of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; previously called 2019-nCoV), initially emerged in Wuhan, China. It has posed a serious threat to human health worldwide. The World Health Organization has declared that COVID-19 is a public health emergency of pandemic proportions[1]. As of December 9, 2020, a total of 67780361 laboratory-confirmed cases including 1551214 deaths have been reported in 220 countries, areas, and territories[1]. The COVID-19 pandemic is currently the world’s most pressing public health threat and has a significant impact on civil societies and the global economy.
It is well established that most individuals with COVID-19 present with fever and typical respiratory symptoms, such as cough and dyspnea, similar to those of SARS and Middle East respiratory syndrome (MERS)[2-5]. Therefore, nasopharyngeal and oropharyngeal swabs are the suitable samples for reverse transcriptase-polymerase chain reaction detection of SARS-CoV-2. However, concurrent extra-pulmonary symptoms, such as gastrointestinal manifestations, mainly including diarrhea, nausea,vomiting, abdominal pain, and anorexia, have also been reported in recent studies[6,7].In addition, rectal swabs and stool specimens of patients with COVID-19 have shown to be positive for SARS-CoV-2, and the virus remained detectable even after the clearance of the virus in the respiratory tract[7-10]. Furthermore, Pan et al[11]demonstrated that patients with digestive symptoms have a longer time from onset to admission and a worse prognosis than that of patients without digestive symptoms[11].Together, these indicate that SARS-CoV-2 can infect and replicate in the gastrointestinal tract, and it may also have potential to cause digestive system damage.With the ongoing COVID-19 pandemic, those studies are of great guiding significance for disease prevention, control, and management. The present review aims to summarize data regarding epidemiology, gastrointestinal characteristics, possible mechanisms, and potential therapeutic strategy in patients infected with coronaviruses(CoVs) from the perspective of the digestive system (Figure 1).
EFFECTS OF COVS ON THE DIGESTIVE SYSTEM
CoVs are a group of enveloped, positive-sense, single-stranded RNA viruses (+ssRNA)with a crown-like appearance, which belongs to the family Coronaviridae of order Nidovirales[12,13]. CoVs harbor the largest genome among those known RNA viruses,with a genome length ranging from 26-32 kilobases (kb) and a diameter in the range of 120-160 nm[14-16]. CoVs are genetically classified into four genera: Alpha-coronavirus,Beta-coronavirus, Gamma-coronavirus, and Delta-coronavirus[12,17]. Alpha-coronavirus and Beta-coronavirus primarily infect mammals, whereas Gamma-coronavirus and Deltacoronavirus usually infect birds[16]. To date, seven coronavirus species under two genera have been identified to cause diseases in human: Alpha-coronavirus (HCoV-NL63 and HCoV-229 E) and Beta-coronavirus (HCoV-OC43, HCoV-HKU1, SARS-CoV, MERSCoV, and SARS-CoV-2)[18].
HCoV-NL63, HCoV-229 E, HCoV-OC43, and HCoV-HKU1 cause mild common cold symptoms, whereas the other three highly pathogenic CoVs have caused large-scale pandemic since the beginning of the 21stcentury: SARS-CoV in 2002 and 2003, MERSCoV in 2012, and the newly emerged SARS-CoV-2[19]. The three highly contagious pathogens are zoonotic in origin and have crossed the species barrier to human.Furthermore, these three viruses are known to cause digestive symptoms.

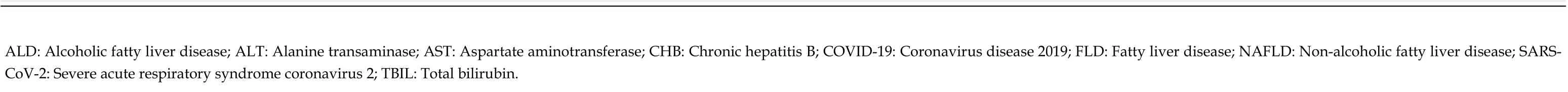
Figure 1 Possible mechanisms of coronavirus disease 2019 on the digestive system. ACE2: Angiotensin-converting enzyme 2; CXCL10: Interferongamma-inducible protein-10; GM-CSF: Granulocyte-macrophage colony stimulating factor; IL: Interleukin; MCP: Monocyte chemoattractant protein; SIRS: Systemic inflammatory response syndrome; TMPRSS2: Transmembrane serine protease 2; TNF: Tumour necrosis factor.
CoVs and digestive manifestations
SARS-CoV: SARS-CoV has a large RNA genome length of 27.9 kb, emerged in the Guangdong Province of China, and had spread to 29 countries and areas worldwide.By July 2003, there were a total of 8098 laboratory-confirmed cases including 774 deaths (case-fatality rate: 9.6%) of SARS[20]. SARS-CoV has been considered to originate from bats, and market palm civets and racoon dogs have been unequivocally considered the intermediate hosts[21].
SARS is characterized by fever and respiratory complications, and it may also lead to acute respiratory distress syndrome and multiple organ failure in severe cases.Moreover, gastrointestinal manifestations are frequently observed in patients with SARS-CoV infection[22]. The tropism of SARS-CoV in the digestive system is commonly known to occur, and a retrospective study demonstrated that 38.4% of patients with SARS had diarrhea, usually within the first week of the disease course[23]. It was also demonstrated that up to 60% of patients with SARS suffered from liver impairment,and SARS-CoV was detected in liver tissue although viral inclusions were not observed[24]. In addition, the rate of SARS-CoV RNA positivity in collected stool specimens increased progressively and peaked at day 11 of the illness, with viral RNA remaining detectable in a stool sample in a patient even 73 d after symptom onset[23,25].Furthermore, the presence of SARS-CoV RNA in the gastrointestinal tract may indicate a poor prognosis, and the viral load in the stool is correlated with death[26].
MERS-CoV: MERS-CoV has a large RNA genome length of 30.1 kb, emerged in the Saudi Arabia, and then spread to 27 countries and areas with a total of 2468 confirmed cases and including 851 associated deaths (case-fatality rate: 34.4%) by the end of September 2019[27]. MERS-CoV has originated from bats, but dromedary camels has been considered the intermediate host[28].
Human-to-human transmission of MERS-CoV occurred mainly through nosocomial transmission[29]. Although most patients with MERS present with nonspecific respiratory symptoms, such as fever, cough, and shortness of breath, approximately one third of patients have gastrointestinal symptoms, such as diarrhea, vomiting, and abdominal pain, which were the most commonly demonstrated extrapulmonary clinical features[30]. In addition, MERS-CoV RNA was detected in 14.6% of stool specimens from patients with MERS, but the positive rate of virus detection was lower than that of SARS[31,32]. Moreover, an in vitro study has shown that MERS-CoV can successfully replicate in human primary intestinal epithelial cells[33].
SARS-CoV-2: SARS-CoV-2 has a genome length of 29.9 kb, shares an approximately 79% sequence identity to the SARS-CoV and the similarity of the whole-genome to BatCoV RaTG13 (a bat coronavirus detected in Rhinolophus affinis) is up to 96.2%[34].Recent studies have suggested that bats may be the natural reservoir of SARS-CoV-2,and that there may be multiple potential intermediate hosts, such as pangolins, minks,and snakes[35-37]. In terms of the current pandemic situation, the case fatality of COVID-19 may not reach as high as that of SARS and MERS.
The majority of patients with COVID-19 exhibit mild to moderate pulmonary symptoms, and SARS-CoV-2 can extend to multiple extra-pulmonary organs including the heart, brain, kidneys, liver, and gut. Based on the data presented in Table 1, 6.7% of the total patients with SARS-CoV-2 infection have diarrhea and there are a great number of patients who had abnormal liver function with a paucity of concurrent or isolated pre-existing digestive system comorbidities. It was reported that COVID-19 patients with diarrhea presented severe symptoms of pneumonia compared to those without diarrhea, and COVID-19 patients with gastrointestinal manifestations or liver injury are more likely to require mechanical ventilation and hospitalization in the intensive care unit than those without gastrointestinal manifestations or liver injury[7,38-40]. Followed by the detection of SARS-CoV-2 RNA in the stool of the first case of COVID-19 in the United States, it was recently reported that viral RNA was detected in 59% of patients with COVID-19 in stool samples and the SARS-CoV-2 lasts significantly longer in stool samples than in respiratory and serum specimens[41,42]. In addition, To and colleagues demonstrated that SARS-CoV-2 was detected in the selfcollected saliva specimens in 91.7% patients with COVID-19[43]. Furthermore, autopsy studies have demonstrated varying degrees of degeneration, necrosis, and shedding in the gastrointestinal mucosa and segmental dilatation and stenosis in the small intestine of patients with COVID-19[44,45]. Taken together, it is therefore likely that SARS-CoV-2 poses a serious threat to the digestive system.
Digestive diseases related to CoV infections
Digestive diseases include a series of disorders that affect the oropharynx and digestive tract, liver and biliary system, and pancreas, affecting human lives commonly. At the beginning of the COVID-19 outbreak, more medical resources were freed up to control the spread of the virus so that more individuals can be protected.Meanwhile, it is safe for most patients with pre-existing diseases. However, it may also increase the relative risk of complications caused by delayed screening, diagnosis, and treatment, and being afraid of seeking medical attention[46]. Challenges encountered regarding the most common pre-existing digestive diseases during the ongoing COVID-19 pandemic are described below.
Liver diseases
Hepatitis refers to inflammation of the liver caused by multiple pathogens (viruses,bacteria, drugs, autoimmune factors, and so on), which can progress to fibrosis,cirrhosis, and even liver cancer, posing a great threat to human health. The most common causes of hepatitis are the five main hepatitis virus types (A, B, C, D, and E)[47]. In a number of studies, hepatitis was noted in patients with SARS and COVID-19[7,11,48,49]. SARS patients with hepatitis B are more likely to develop severe hepatitis than in those without. Similarly, severe cases of COVID-19 were more prone to infect HBV than non-severe cases[48,50]. Collectively, these findings show that CoVs might play a significant role in hepatitis, although detailed studies are needed to confirm this.
Fatty liver disease is a spectrum of disorders characterized predominantly by macrovesicular hepatic steatosis, and it presents a condition of excess fat stored in theliver, including non-alcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease (ALD). Patients with hypertension, diabetes, obesity, and old age have a high risk of developing severe COVID-19[51]. These comorbidities also increase the risk of NAFLD, thus leading to liver injury. The ongoing COVID-19 pandemic has several negative effects on individuals, especially those encountering job loss, financial strain,death of a loved one, and so on. Under these stressors, an individual’s alcohol consumption is likely to increase[52]. Therefore, COVID-19 is likely to have a longlasting impact on the development of ALD.
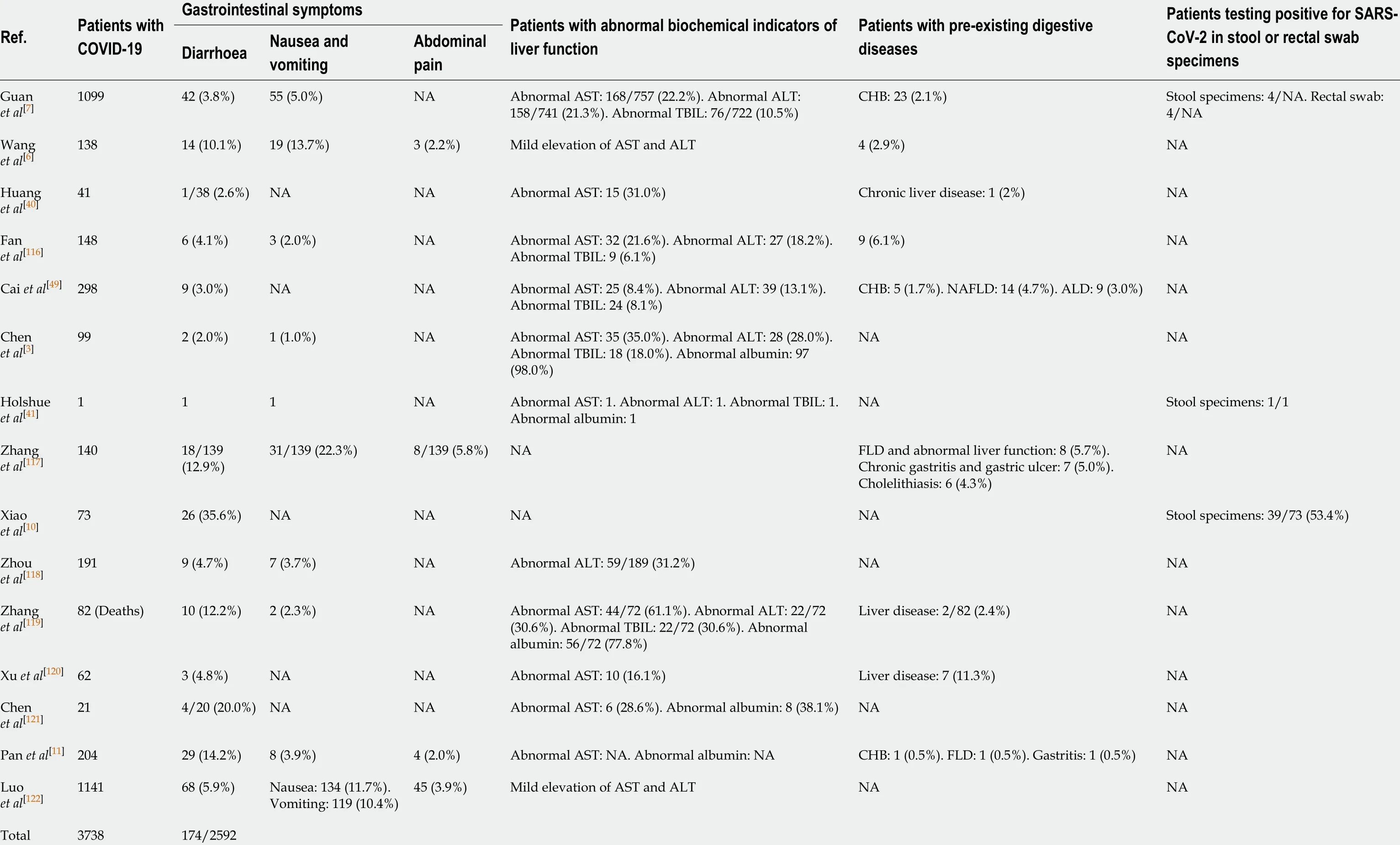
Table 1 Presentation of gastrointestinal symptoms, abnormal liver function, and pre-existing digestive diseases in patients with severe acute respiratory syndrome coronavirus 2 infection
(6.7%)
Given that patients with liver cirrhosis and cancer have a high risk of infection due to the immunocompromised status[53], measures to prevent SARS-CoV-2 infection are needed. Xiao and colleagues designed a study showing that none of the participants who undertook precautionary and protective measures had clinical symptoms suggestive of SARS-CoV-2 infection, whereas 17 of 101 patients with decompensated cirrhosis who did not undertake these measures were diagnosed with COVID-19[54].This research suggests that more strategies should be implemented to prevent SARSCoV-2 infection in patients with liver cirrhosis and cancer, such as online health education and medication guidance.
The outbreaks of SARS and MERS might potentially increase the risk of transmission of viral infection from donors to recipients and thus even lead to death[40,55]. Tzedakis et al[56]reported that a local liver transplant center decreased transplant activity by 60% since the COVID-19 pandemic and that it is crucial and necessary to balance costs and benefits while performing liver transplant[56]. During the COVID-19 pandemic, all donors and recipients of liver transplant must be screened for the presence of SARS-CoV-2 to ensure the safety and success of the liver transplantation.
Gastrointestinal diseases
Ulcerative colitis and Crohn's disease are two major idiopathic inflammatory bowel disorders (IBDs) that could cause prolonged inflammation of the gastrointestinal tract[57]. Patients with IBD who use immunosuppressive and biological agents are more susceptible to opportunistic and severe infections than those who do not[58,59].Therefore, it is reasonable to assume that patients with IBD have more severe COVID-19, although there has been no direct clinical evidence to prove it. An and colleagues showed that none of the 318 patients with IBD (204 with ulcerative colitis and 114 with Crohn‘s disease)developed SARS-CoV-2 infection with early effective warning and protective measures[60]. In addition, patients with cancer also have an increased risk of infection[61]. Furthermore, it was demonstrated that individuals with cancer may have a high risk of severe COVID-19 and a poorer prognosis[62]. Although the risk of SARSCoV-2 infection in patients with gastrointestinal cancer remains unknown, effective precautionary approaches are necessary to better protect patients.
POSSIBLE MECHANISMS OF COVID-19 ON THE DIGESTIVE SYSTEM
It has been commonly known that respiratory droplets and direct contact are the two major transmission pathways of SARS-CoV-2. However, a recent study performed by Liu and colleagues has shown a possibility of aerosol transmission[63]. A large number of studies have reported gastrointestinal symptoms and liver dysfunction in patients with SARS-CoV-2 infection. At the same time, SARS-CoV-2 could be detected in rectal swabs and stool specimens in patients with COVID-19[7,10]. Moreover, biopsy and autopsy reports have revealed that COVID-19 caused pathological changes in the digestive system. In addition, high airborne concentration of SARS-CoV-2 was detected in toilet room of Fangcang Hospital where patients with COVID-19 were treated[63]. Taken together, these research findings provide a theoretical basis for the spread of COVID-19 through the faecal-oral route, although there is no direct evidence for the transmission pathway thus far.
The digestive tract communicates with the outside world directly, similar to the respiratory tract. Therefore, SARS-CoV-2 has the opportunity to enter the gastrointestinal tract and cause a direct cytopathic effect by local replication. In addition, systemic responses to excessive immune inflammation induced by SARSCoV-2 infection may also cause damage to the digestive system indirectly. However,the mechanisms of how COVID-19 affects the digestive system remain poorly known.Furthermore, there is also no specific antiviral drug or vaccine approved to treat or prevent COVID-19 to date. Hence, it is particularly urgent to identify the potential therapeutic strategies for COVID-19.
Angiotensin-converting enzyme 2 and transmembrane serine protease 2
Angiotensin-converting enzyme 2 (ACE2) is a well-known receptor located on cells of various organs for regulating cardiovascular function through the renin-angiotensin system, playing a major role in regulating hypertension and anti-atherosclerosis mechanisms[64,65]. In recent two decades, the role of ACE2 in SARS-CoV and influenza virus infection as a target functional receptor has attracted widespread attention[66-68]. It has been reported that the entry of SARS-CoV-2 into the host cell depends on the binding of viral spike (S) proteins to the SARS-CoV receptor ACE2 followed by the transmembrane serine protease 2 (TMPRSS2) for the S protein priming[69]. Therefore,human cells co-expressing ACE2 and TMPRSS2 are susceptible to SARS-CoV-2 infection[70]. A recent study performed by Zhang and colleagues has demonstrated that type II alveolar cells have higher expression of ACE2 and TMPRSS2 than type I alveolar cells in the lung. Besides, co-expression of ACE2 and TMPRSS2 has also been found in the glandular cells of upper esophageal and absorptive enterocytes of the ileum and colon[70,71]. Intestinal epithelial cells can act as a barrier and help to coordinate immune responses in microbial infections[72]. A number of studies have reported that absorptive enterocytes can be damaged or developed malabsorption and intestinal secretion abnormalities due to coronavirus or rotavirus infection, thus resulting in diarrhea and vomiting[73,74]. Therefore, gastrointestinal manifestations in patients with COVID-19 might be associated with infected enterocytes co-expressing ACE2 and TMPRSS2. Moreover, co-expression of ACE2 and TMPRSS2 has been observed in cholangiocytes, but not in hepatocytes[75]. Cholangiocytes play a pivotal role in liver regeneration and immune responses, and injury of cholangiocytes may cause a variety of diseases and even lead to liver failure[76]. Therefore, we can preliminarily conclude that the abnormal liver function in patients with COVID-19 may not be directly caused by the damage to hepatocytes, but it may be caused by damage to cholangiocytes. Liver damages may also be caused by other factors, such as drugs used in the treatment or systemic inflammatory response.
Compared with control mice, ACE2 knockout mice are more susceptible to induced colitis upon treatment with chemical irritants[77]. The expression of ACE2 protein is downregulated after virus entry, which may worsen the digestive symptoms.Recently, studies have demonstrated that the fusion protein of human recombinant ACE2 (hrACE2) with the Fc fragment of the human immunoglobulin IgG1 showed high affinity to the receptor-binding domain (RBD) of SARS-CoV-2 and potently neutralized SARS-CoV-2 in vitro[78,79]. A newly online published report in Nature demonstrated that CB6, a neutralizing monoclonal antibody (mAb) isolated from a patient with convalescent COVID-19, can block the binding of soluble SARS-CoV-2 RBD with ACE2 receptor and showed inhibitory effect to SARS-CoV-2 infection in vitro and in rhesus monkeys[80]. Additionally, a recent in vivo study has reported that hrACE2 can block the early stages of SARS-CoV-2 infection at the organoid level in engineered human blood vessels, kidneys, and small intestinal enterocytes[78,81].Moreover, a serine protease TMPRSS2 inhibitor has been approved for clinical use to block the entry of CoVs[69]. Taken together, it is therefore likely that ACE2 and TMPRSS2 may be the potential targets for prevention and treatment of the COVID-19 patients with digestive symptoms.
Immune injury
Immune injury plays an important role in the occurrence, development, and prognosis of digestive diseases[82-84]. A growing body of evidence suggests that severe SARS-CoV-2 infection can activate innate and adaptive immune responses, increase serum levels of pro-inflammatory cytokines and chemokines including interleukin (IL)-6, IL-1β, IL-2, IL-10, tumor necrosis factor α (TNF-α), interferon-gamma-inducible protein-10(CXCL10), monocyte chemoattractant protein-1, and granulocyte-macrophage colony stimulating factor, and even induce systemic inflammatory response syndrome (SIRS)and cytokine storm, thus leading to local and systemic tissue damage[40,85,86].Concentrations of IL-6 were significantly different between patients with mild and severe COVID-19, and elevated IL-6 was found to be a stable indicator of adverse outcomes for severe COVID-19 patients. A clinical trial (ChiCTR2000029765) that explored the potential therapeutic effect of IL-6 receptor-targeted mAb in patients with severe COVID-19, has shown the effectiveness of controlling fever and improving respiratory function quickly[87]. It has been reported that vagus nerve stimulation(VNS) can exert anti-inflammatory effects via activation of the cholinergic antiinflammatory pathway[88,89]. Based on preliminary observations and available scientific and clinical data, it is speculated that VNS may play a vital role in improving the prognosis of patients with COVID-19[90]. Additionally, patients with severe COVID-19 more frequently have lymphopenia, and drastically decreased numbers of CD4+and CD8+T cells than moderate cases. Furthermore, inflammation-mediated gastrointestinal tissue damage in patients with COVID-19 is supported by the histopathological evidence of diffuse endothelial inflammation in the small intestine submucosa[91]. It has also been confirmed by the presence of numerous infiltrating plasma cells and lymphocytes with interstitial edema in the lamina propria of the stomach, duodenum, and rectum of patients with COVID-19[10].
Gut microbiota
The human intestine harbors nearly 100 trillion microorganisms, which are composed of more than 1000 different bacterial species, including but not limited to bacteria,fungi, and viruses[92,93]. It is known that gut microbiota plays a vital role in a variety of diseases, including digestive, metabolic, respiratory, and even neuropsychiatric diseases[94-96]. Additionally, many studies have reported that chronic respiratory diseases and pneumonia can not only change the airway microbiota, but also alter the gut microbiota indirectly through the circulatory and lymphatic systems[97-100]. SARSCoV-2 can down-regulate the expression of ACE2 in the intestine, which affects the absorption of tryptophan, resulting in damage to the gut microbiota and possibly influencing intestinal inflammation[101,102]. Xu et al[103]indicated that some patients with COVID-19 showed gut microbial dysbiosis with decreased abundance of Lactobacillus and Bifidobacterium[103]. Zuo et al[104]showed that the increased levels of Coprobacillus,
Clostridium hathewayi, and Clostridium ramosum were positively correlated with the susceptibility and severity of COVID-19[104]. Furthermore, studies have shown that short-chain fatty acids, the most critical metabolites of the gut microbiota, play an important role in reducing the intestinal pH, maintaining the integrity of the intestinal epithelium, and enhancing the host systemic immunity[105-107]. Antibiotics are commonly prescribed in patients with COVID-19, however, it can also profoundly perturb the composition of the human gut microbiota[108]. Guidance from China’s National Health Commission and National Administration of Traditional Chinese Medicine suggested that the use of probiotics has a good curative effect in patients with severe SARS-CoV-2 infection. Taken together, improvement of the composition of the gut microbiota and its metabolites may be a potential strategy for the treatment of COVID-19.
Hypoxemia
After SARS-CoV-2 infects the lungs, it causes inflammation and edema of the pulmonary parenchyma and interstitium, which in turn affect alveolar gas exchange and thereby lead to hypoxemia[109]. Hypoxemia can cause metabolism and normal physiological dysfunctions in various tissues and organs including the digestive system. Long-term hypoxemia can cause cell necrosis, which in turn leads to damage of the gastrointestinal mucosal cells, thus leading to gastrointestinal ulceration and bleeding.
Psychological stress
Psychological stress has a profound influence on the digestive system, it can alter the intestinal motility, increase the gastrointestinal permeability, and change the composition of intestinal microbiota[110]. A study on active Weibo users showed that individuals were more concerned about their health and showed more negative emotions, such as anxiety and depression, after the outbreak of the COVID-19[111].Quarantine is an effective measure to protect individuals from contagious patients and those who are at risk of infection, however, it may also increase negative psychological stress[112]. Taken together, digestive diseases and symptoms in patients with COVID-19 may be partially caused by psychological stress.
Others
Multiple lines of evidence has shown that some patients with COVID-19 have digestive system symptoms, such as nausea, vomiting, and anorexia, which indirectly reflect the impairment of the dorsal vagal complex[6,113,114]. One of the possible mechanisms is that the neurotropic virus retrogrades along the vagus nerve once the virus enters the vagal nerve endings, thus damaging the brainstem[115]. Moreover, the virus may reach the brainstem through the circulatory system with or without crossing the blood–brain barrier[113].
CONCLUSION
CoV infections can cause a series of digestive diseases, and may also be accompanied by digestive manifestations and abnormal digestive function. Although it is still unknown whether the SARS-CoV-2, which causes abnormalities in the digestive system, enters the digestive system directly or indirectly affects the digestive system, it is necessary to undertake early measures to prevent the spread of the virus through the fecal-oral transmission. In addition to ACE2 and immune injury, gut microbiota,hypoxemia, and psychological stress may also be targets for future intervention and treatment of digestive system damage caused by SARS-CoV-2 infection. Further research is warranted to elucidate the relationship between the COVID-19 and the digestive system.
杂志排行
World Journal of Gastroenterology的其它文章
- Xiangbinfang granules enhance gastric antrum motility via intramuscular interstitial cells of Cajal in mice
- Sinapic acid ameliorates D-galactosamine/lipopolysaccharideinduced fulminant hepatitis in rats: Role of nuclear factor erythroidrelated factor 2/heme oxygenase-1 pathways
- Quantitative multiparametric magnetic resonance imaging can aid non-alcoholic steatohepatitis diagnosis in a Japanese cohort
- Clinicopathological features and prognostic factors associated with gastroenteropancreatic mixed neuroendocrine non-neuroendocrine neoplasms in Chinese patients
- Effect of liver inflammation on accuracy of FibroScan device in assessing liver fibrosis stage in patients with chronic hepatitis B virus infection
- Simultaneous partial splenectomy during liver transplantation for advanced cirrhosis patients combined with severe splenomegaly and hypersplenism
