Giant pseudoaneurysm of the splenic artery within walled of pancreatic necrosis on the grounds of chronic pancreatitis
2021-03-05MiliMitroviJovnoviDusnSponjskiAleksndrDjuriStefnoviAleksndrJnkoviStefnMiloseviKtrinStosiDjordjeKnezeviJelenKov
Mili Mitrovi Jovnovi , Dusn Sponjski , , Aleksndr Djuri Stefnovi , ,Aleksndr Jnkovi , Stefn Milosevi , Ktrin Stosi , Djordje Knezevi ,Jelen Kov ,
a Department of Abdominal Radiology, Center for Radiology and MRI, Clinical Center of Serbia, Belgrade, Serbia
b Faculty of Medicine, University of Belgrade, Belgrade, Serbia
c Clinic for Digestive Surgery –First Surgical Clinic, Clinical Center of Serbia, Belgrade, Serbia
Chronic pancreatitis is a long-standing inflammation of the pancreas, characterized by progressive inflammatory and fibrotic changes, resulting in permanent structural damage of pancreatic parenchyma [1]. Pancreatitis (chronic or acute) is the primary risk factor for pseudo-splenic artery aneurysms, along with pancreatic pseudocysts and trauma. As the disease progresses, patients with chronic pancreatitis may develop complications due to exocrine and endocrine pancreatic functional loss, such as fat malabsorption with steatorrhea, glucose intolerance, and ultimately diabetes mellitus [1 , 2]. Furthermore, severe pancreatic inflammation can cause weakening of vessel walls, with subsequent formation of arterial pseudoaneurysms. Splenic artery is the most commonly affected visceral artery [2 , 3]. Liver cirrhosis, portal hypertension, liver transplantation, atherosclerosis, hypertension, pregnancy and multiparity are main risk factors for true splenic artery aneurysms [2]. Rupture and intraperitoneal bleeding is the cause of death in 30% -50%of patients. Thus, prompt diagnosis and appropriate treatment are of great clinical importance [4 , 5]. Herein, we present a case of a giant splenic artery pseudoaneurysm within a walled of necrosis involving pancreatic parenchyma, as a complication of long standing chronic pancreatitis.
A 56-year-old male patient with a history of chronic pancreatitis was referred to our surgery clinic with acute worsening of abdominal pain, dyspepsia and fatigue which lasted for 3 months. Abdominal ultrasound (US) examination with color Doppler showed a large cystic lesion with internal a turbulent blood flow in the pancreatic tail ( Fig. 1 ). Further contrast-enhanced computed tomography (CT) scan revealed a heterogeneous mass with a maximum diameter of 166 ×135 mm at the pancreatic tail extending to the hilum of the spleen ( Fig. 2 A). In addition, multiple calcifications and smaller cysts were found in the head and body of pancreas, as signs of chronic pancreatitis. Central enhancing component in cystic lesion was compatible with pseudoaneurysm originating from the splenic artery, surrounded by necrotic tissue( Fig. 2 B).
Due to the high risk of the aneurismatic rupture, the patient underwent surgery withenblocresection of the spleen, distal pancreas and aneurysmatic segment of the splenic artery. A 20-cm pulsatile splenic artery pseudoaneurysm was found in pancreatic tail, which was even larger than that on previous CT exam ( Fig. 3 ).Histopathological examination revealed a pseudoaneurysm of the splenic artery inside the walled of necrotic collection involving the body and tail of pancreas. The postoperative course was uneventful, and the patient was complication-free 3 months after the procedure.
Chronic pancreatitis is characterized by chronic inflammation of pancreatic parenchyma that leads to permanent deficiency of both endocrine and exocrine functions [1 , 2]. The causes of chronic pancreatitis are complex and involve both environmental and genetic factors, with alcohol consumption, nicotine usage, pancreatic duct obstruction and hyperlipidemia being the most common. Various complications can develop during the course of disease, such as different types of fluid collections (pseudocysts and walled of necrosis), pancreatic ascites, pleural effusion, mechanical obstruction of the gastrointestinal tract and common bile duct,splenic vein thrombosis with portal hypertension and subsequent varices bleeding, and pseudoaneurysm formation. Visceral pseudoaneurysms are rare but life-threatening complication of pancreatitis. The formation of pseudoaneurysm occurs with a higher incidence in chronic pancreatitis (4% -8%) than that in acute pancreatitis [3 , 4]. There are two main mechanism of pseudoaneurysm formation. The most common cause is leakage of pancreatic enzymes and severe peripancreatic inflammation causing disruption of the vessel wall with subsequent pseudoaneurysm formation. Another mechanism is a communication of pancreatic pseudocyst or walled of necrosis with a peripancreatic vessel converting a fluid collection into a pseudoaneurysm [4], as in our case. Most commonly involved artery is the splenic artery, followed by the gastroduodenal,pancreaticoduodenal, and hepatic arteries [4 , 5]. Visceral pseudoaneurysms can also develop as a result of abdominal trauma, peptic ulcer disease and iatrogenic causes [6 , 7].
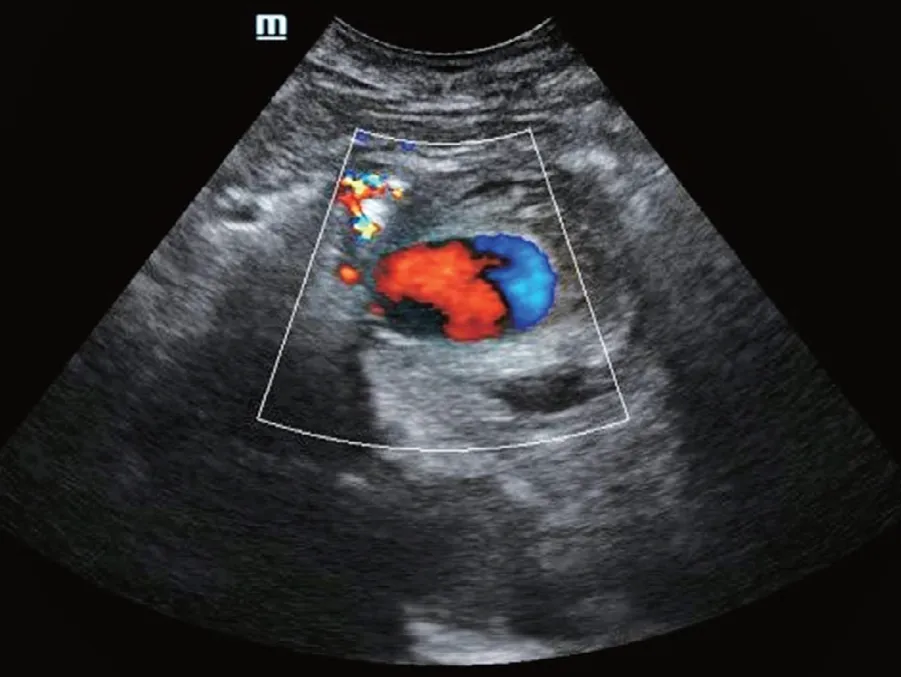
Fig. 1. A large cystic lesion in the pancreatic tail. Color Doppler US revealed a turbulent blood flow in the cyst.
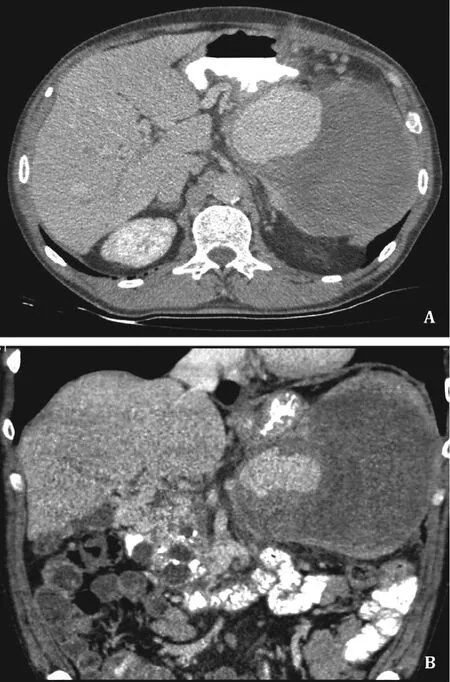
Fig. 2. A: Heterogeneous mass in region of pancreatic tail extending to the hilum of the spleen. B: Central enhancing component in cystic lesion was compatible with pseudoaneurysm originating from the splenic artery, surrounded by necrotic tissue.
Majority of the pseudoaneurysms present nonspecific symptoms, such as abdominal pain. Less than 2.5% of the cases are asymptomatic and discovered incidentally. The most severe complication of pseudoaneurysm is rupture with bleeding in pancreatic duct which mimics gastrointestinal bleeding, or bleeding directly in peritoneal or retroperitoneal cavity with a high mortality rate of 30% -50% [8].
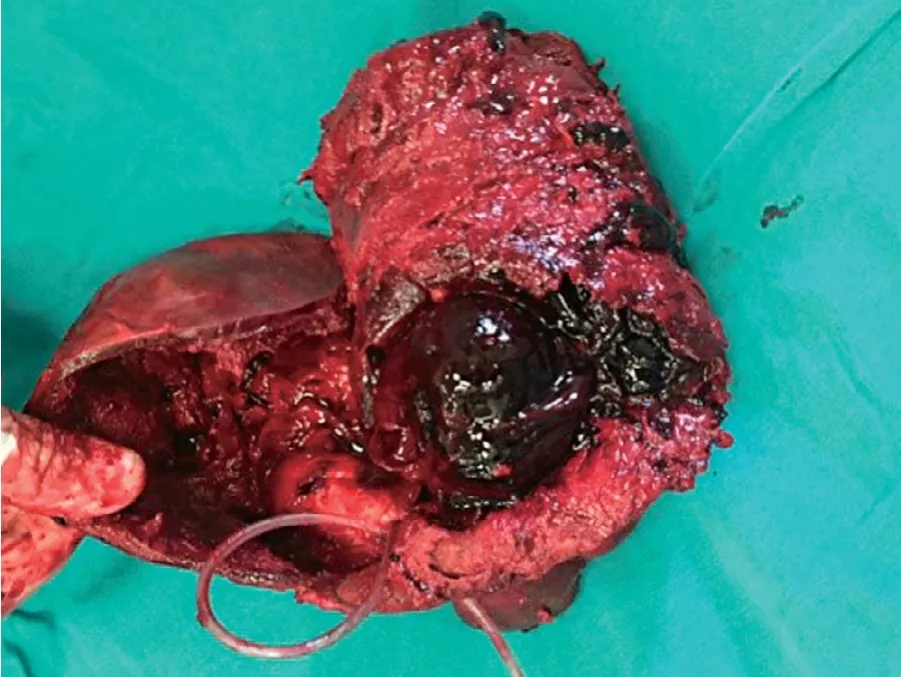
Fig. 3. A 20-cm pulsatile splenic artery pseudoaneurysm was found in pancreatic tail.
Diagnostic modalities used for diagnosis of splenic artery pseudoaneurysm include US, Doppler US, CT and angiography. Doppler US can raise the suspicion of pseudoaneurysm, but CT should be the first choice of diagnostic tool, as it can delineate the anatomy and location of the pseudoaneurysm in details [9]. Several studies have shown that angiography is extremely valuable in localizing bleeding pseudoaneurysms [10-12].
The optimal therapeutic strategy is still controversial. Management of pseudoaneurysms depends on their dimensions, location, complications and most frequently involves open abdominal surgery, as what was performed in our case. Laparoscopic resection is another surgical option in selected cases. Moreover, endovascular treatment with angioembolization is being increasingly used due to improved technical capabilities and low morbidity rates [11 , 12].
In conclusion, pseudoaneurysms are rare complications of pancreatitis, with high mortality rates associated with hemorrhage.Considering these facts, it is important to keep in mind that pseudoaneurysms can develop in patients with chronic pancreatitis and large pseudocysts or incapsulated necrotic collections. Due to possible complications, the prompt diagnosis and appropriate treatment are of greatly clinical importance.
Acknowledgments
None.
CRediT authorship contribution statement
Milica Mitrovic Jovanovic:Conceptualization, Data curation,Writing - original draft.Dusan Saponjski:Conceptualization, Writing - original draft.Aleksandra Djuric Stefanovic:Project administration, Supervision, Validation.Aleksandra Jankovic:Formal analysis, Investigation.Stefan Milosevic:Methodology, Project administration, Resources.Katarina Stosic:Formal analysis, Resources.Djordje Knezevic:Conceptualization.Jelena Kovac:Supervision,Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by the Hospital Ethics Committee.Consent was obtained from the patient for publication of this report and any accompanying images.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- BCLC staging system and liver transplantation: From a stage to a therapeutic hierarchy
- Multidisciplinary management of patients with post-inflammatory pancreatic necrosis
- Abdominal drainage systems in modified piggyback orthotopic liver transplantation
- Liver transplantation for liver failure in kidney transplantation recipients with hepatitis B virus infection
- Transjugular portosystemic shunt for early-onset refractory ascites after liver transplantation
- Hepatic isolated ectopic adrenocortical adenoma mimicking metastatic liver tumor