Prognostic factors affecting long-term outcomes in patients with brain metastasis from esophageal carcinoma
2021-01-18PengZhangLejingYaoMingChenWeiFeng
Peng Zhang ,Lejing Yao ,Ming Chen ,Wei Feng
1Department of Radiology Physics,The Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital),Institute of Basic Medicine and Cancer (IBMC),Chinese Academy of Sciences,Hangzhou 310022,China;2Department of Radiation Oncology,The Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital),Institute of Basic Medicine and Cancer (IBMC),Chinese Academy of Sciences,Hangzhou 310022,China
Abstract Objective:The incidence of brain metastasis from esophageal cancer (BMEC) has increased in recent years.Thus,it is necessary to identify factors that affect long-term outcomes for such patients.Methods:From January 1997 to July 2018,consecutive patients (10,043 patients,31 with brain metastasis) with esophageal cancer (EC) treated at Zhejiang Cancer Hospital were recruited for retrospective analysis.Demographic,clinical,and pathological variables and the survival data were retrieved.Results:The median time from diagnosis of EC to diagnosis of brain metastases was 7.67 (range,0.43-55.20)months.The median survival time of BMEC patients from diagnosis of primary esophageal tumor was 16.7 (range,2.33-163.30) months and the median survival time from the point of diagnosis of brain metastasis was 6.47 (range,0.43-148.13) months.Univariate and multivariate analyses showed that the pathology type,EC without chemotherapy,and bone metastasis history were significantly associated with a shorter time interval between the first treatment of EC and brain metastasis.Chemotherapy history after brain metastasis,whole brain radiation therapy (WBRT) history,and surgery were significant predictors for better long-term survival outcomes.Conclusions:Our findings indicate that the use of surgery,WBRT,and chemotherapy can achieve the best therapeutic effects for BMEC patients.
Keywords:Brain metastasis from esophageal cancer;time to brain metastasis (TTBM);prognosis factors;survival time;radiotherapy;chemotherapy
Introduction
Esophageal cancer (EC) is the eighth most common cause of cancer and the sixth most common reason for cancerrelated mortalities worldwide (1).In China,EC is the fourth leading cause of cancer deaths,with an incidence of 27.54/100,000 in men and 14.05/100,000 in women (2).Currently,despite the availability of various clinical therapeutics for EC,the 5-year survival rate is less than 15%. Therefore, it is important to determine the prognostic factors for EC in order to improve patient survival.
Risk factors for the development of EC include biological factors (3),dietary factors (4),lifestyle and habits(5),mental health (6),and environmental factors (7).EC can metastasize to multiple organs throughout the body (8).The invasion and metastasis of EC to the surrounding tissues can cause superior vena cava compression syndrome(9),voice hoarseness (10),jaundice,ascites,and liver failure(11).The most common sites of distant metastases of EC are the lungs,pleura,liver,stomach,peritoneum,kidneys,adrenal gland,and bones (12).The reported incidence of lung metastases from EC is 14.97% (13).Gastric metastasis from EC is very rare,with an incidence of 1%-4.58% in clinical practice,and is often found accidentally during autopsy or surgery (14).Renal metastasis from EC is also rare,with an overall survival of 2 months to 9 years after nephrectomy with or without adjuvant chemotherapy (15).Studies have shown that the incidence of bone metastases from EC is 2%-6%,with a mean survival time of 4 months after the first detection of sclerosing lesions (16).In addition to these distant metastases mentioned above,brain metastases from EC (BMEC) have also been reported,but the incidence is rare (17-19).However,most of the studies on BMEC are case reports and about 200 cases of BMEC have been reported to date (17-19).The autopsy of patients with primary EC revealed that the incidence of BMEC was 5% (20).Because BMEC is rare,the risk and prognostic factors for BMEC are not clear.Further,there are no standardized treatment guidelines for such patients.
In this study,we performed a retrospective review of consecutive patients with EC who received treatment at Zhejiang Cancer Hospital.We analyzed the frequency of brain metastases,survival,and prognosis-associated factors as well as the therapeutic options for BMEC.
Materials and methods
Patients
Our retrospective study has been reviewed and approved by the Ethics Review Committee of Zhejiang Cancer Hospital.In this retrospective study,EC patients with brain metastases diagnosed and treated at Zhejiang Cancer Hospital from January 1997 to July 2018 were evaluated.We collected demographic characteristics,clinical features,and treatment methods for patients with BMEC and obtained informed consent from all participants.
Data collection
Using the clinical information,patients were classified into three groups according to the Radiation Therapy Oncology Group Recursive Partitioning Analysis (RTOG RPA)grades:grade I,Karnofsky performance status (KPS) ≥70,age <65 years old,primary foci were controlled,and no extracranial metastasis was observed;grade III,KPS<70;grade II,patients who did not satisfy the above-mentioned grade I or III criteria.
Magnetic resonance imaging (MRI) features including the number,location,size,nature,and imaging features of primary lesions including the length of lesions were collected.The extent of surgical resection and the clinical and radiological follow-up details were also collected.We documented the critical time points for patients and the causes of death whenever possible.The clinical staging of the disease,the details about the treatment of BMEC,the status of the primary tumor at the time of death or before death,and the follow-up records were noted in this study.
Follow-up protocol
Telephone or outpatient follow-up is performed at Zhejiang Cancer Hospital.Outpatient follow-up was comprehensive and included the medical history,physical examination,and imaging examination [chest computed tomography (CT),upper abdominal CT,head MRI,head CT,etc].Endoscopic examination was also performed if necessary.The frequency of follow-up was determined by the attending physician according to the patient’s condition.Follow-up was generally conducted once every 3 months within 2 years,once every 6 months within 2-5 years,and once a year after 5 years.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics (Version 25.0;IBM Corp.,New York,USA).Descriptive analysis was conducted to illustrate the patients’ clinicopathological characteristics.For survival analysis,the Kaplan-Meier survival curve was used to estimate the median survival time and the log-rank test was used for comparisons.A Cox proportional hazards model was used to evaluate the prognostic factors that affected survival in the multivariate analysis.A two-sided P<0.05 was considered statistically significant.
Results
Baseline characteristics
Out of 10,043 patients with EC treated at Zhejiang Cancer Hospital during the study period,31 patients developed brain metastases.Clinical features of these 31 patients (30 males and 1 female) diagnosed with BMEC are presented inSupplementary Table S1.The median age was 58 (range,42-74) years.Among the 31 BMEC patients,26 (83.9%)patients had squamous cell carcinoma,3 (9.7%) patients had adenocarcinoma,and 2 (6.5%) patients had small cell carcinoma.The median time from the diagnosis of EC to the diagnosis of brain metastases was 7.67 (range,0.43-55.20) months.Twenty-eight patients (90.3%) had a KPS score ≥70 and 3 patients (9.7%) had a score <70 at the time of BMEC diagnosis.Nine (29%),19 (61.3%),and 3(9.7%) patients were classified as Recursive Partitioning Analysis (RPA) grades I,II,and III,respectively.Sixteen patients with BMEC had distant metastases at other sites at the time of diagnosis.Eleven patients (35.5%) had BMECrelated clinical symptoms while 20 patients (64.5%) had no obvious BMEC-related clinical symptoms at the time of diagnosis of brain metastases.Supplementary Table S2shows various treatments patients received for the primary esophageal tumor.Two patients who were diagnosed with brain metastases during primary radiotherapy were included in the other category as shown inSupplementary Table S2.
Radiological features
The median length of esophageal primary lesions was 5(range:1-9) cm.Full-thickness involvement of esophagus for primary lesions was observed in 3 (9.7%) patients.Eighteen (58.1%) patients had solitary metastases,4(12.9%) patients had 2 metastatic lesions,and 9 (29.0%)patients had multiple metastases (3 or more tumors).Additionally,75.8% of 62 lesions were located in the cerebrum (12 frontal lobe,24 parietal lobe,6 temporal lobe,5 occipital lobe),and 15 lesions were located in the cerebellum.There were 49 lesions from esophageal squamous cell carcinoma,of which 40 (81.6%) were located in the cerebrum and 9 were located in the cerebellum.There were 8 lesions from esophageal adenocarcinoma,of which 7 (87.5%) were in the cerebrum and 1 was in the cerebellum.There were 5 small cell cancer lesions located in the cerebellum.The brain lesions were solid,cystic,and solid-cystic in 5 (16.1%),6 (19.4%),and 20 (64.5%)patients,respectively (Supplementary Table S1).
Management of BMEC
Among the 31 patients,9 patients underwent whole brain radiation therapy (WBRT) alone and 3 patients were administered chemotherapy alone.Eleven patients received combined radiation therapy and chemotherapy,and 2 patients underwent combined surgery and radiation therapy.Four patients received triple therapy including surgical resection,radiation therapy and chemotherapy.Two patients did not receive any aggressive treatment due to prognostic factors such as advanced primary tumor and other systemic metastases (Supplementary Table S3).Surgery was performed to select patients with predominantly single lesions.
Follow-up data
The median survival of BMEC patients from the time of diagnosis of primary esophageal tumor was 16.70 (range,2.33-163.30) months and that from the time of diagnosis of brain metastasis was 6.47 (range,0.43-148.13) months.During the follow-up period after BMEC treatment,2 patients experienced a recurrence of brain metastases,in which one metastasis recurred after gamma knife surgery and 3 cycles of chemotherapy.This patient was again treated with WBRT and subsequently received local radiation therapy for the inguinal lymph nodal metastasis.Until the statistical deadline (July 2018),the patient was alive at 22.10 months from the time of diagnosis of primary esophageal tumor.Another patient who suffered relapses underwent 3 brain resections during follow-up period and had survived for 11.63 months from the time of diagnosis of the primary esophageal tumor.One patient who had undergone surgery, whole brain irradiation, and chemotherapy after the diagnosis of brain metastases was still alive at 148 months from the time of diagnosis of primary esophageal tumor.In the final phase of follow-up,5 patients were alive and 26 patients had died(Supplementary Table S4).Among the fatal cases,15(48.4%) patients died due to brain metastasis and 11(35.5%) patients died of other systemic lesions.
Survival analysis
For survival analysis,the study period was divided into 2 parts:1) The time interval between the first treatment of EC and the diagnosis of brain metastasis (time to brain metastasis,TTBM);and 2) The time interval between the diagnosis of brain metastasis and the time of death or the last follow-up (survival time).
The median TTBM was 6.200 [95% confidence interval(95% CI):3.139-9.261] months.The median TTBMs for patients with squamous cell carcinoma and adenocarcinoma EC were 10.000 (95% CI:0.631-19.369) months and 4.270(95% CI:0-8.975) months,respectively (Figure 1A,P=0.015).The median TTBM for patients with bone metastases was significantly shorter than that for those without bone metastases [1.03 (95% CI:0-2.35) monthsvs.8.000 (95% CI:2.564-13.430) months,P=0.028] (Figure 1B).As shown inFigure 1C,the median TTBM for patients who received chemotherapy for the primary tumor was significantly shorter than that for those who did not [0.900(95% CI:0.148-1.652) monthsvs.8.000 (95% CI:2.222-13.778 months,P=0.005)].The Cox proportional hazards model revealed that TTBM was significantly shorter in patients who received surgery and chemotherapy for primary esophageal tumors (P=0.013),bone metastasis(P=0.021) and stage of T (second class) (P<0.001) (Table 1).
We performed univariate analysis to determine factors that affect the survival time using the Kaplan-Meier method (Table 2).The median survival time for the 31 patients with brain metastasis was 17.530 (95% CI:8.233-26.827) months and the 1-year survival rate for this group was 56.9% (70.8% for single brain lesions and 30.8% for multiple brain lesions,P=0.946) (Figure 2A).The median survival time for BMEC patients was 6.900 (95%CI:5.102-8.698) months and the 1-year survival rate was 23.8% (31.5% for single brain lesions and 0 for multiple brain lesions,P=0.179) (Figure 2B,C).Furthermore,the median survival times for BMEC patients with different RPA grades were compared.The median survival times for patients with RPA grades I,II,and III were 7.800 (95% CI:3.914-11.686) months,6.300 (95% CI:4.870-7.730)months,and 28.170 (95% CI:0-72.243) months,respectively (P=0.184) (Figure 2D).BMEC patients who received WBRT had a median survival time of 10.300(95% CI:5.182-15.418) months,which was significantly longer than the time for those who did not receive WBRT[3.200 (95% CI:1.159-5.241) months,P<0.01] (Figure 2E).
The multivariate analysis showed that surgery for brain lesion (P=0.035) chemotherapy for brain metastasis(P=0.048) and WRBT (P=0.001) were independent predictors of survival time after the diagnosis of brain metastasis (Table 3).
Discussion
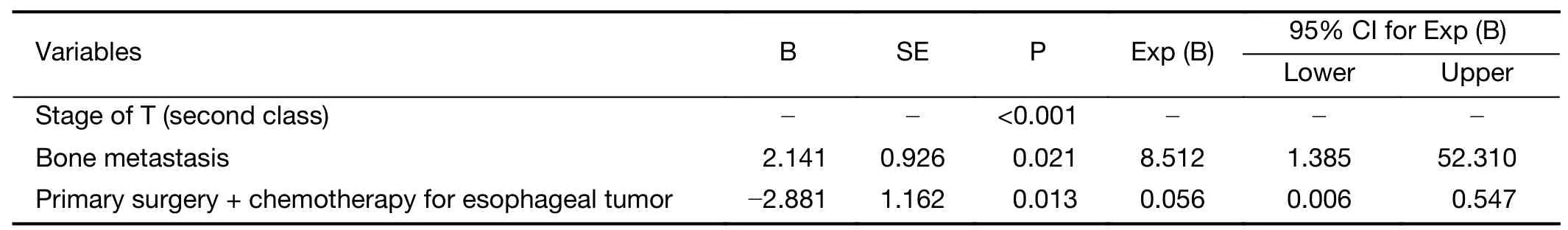
Table 1 TTBM-related factors analyzed with proportional hazards model
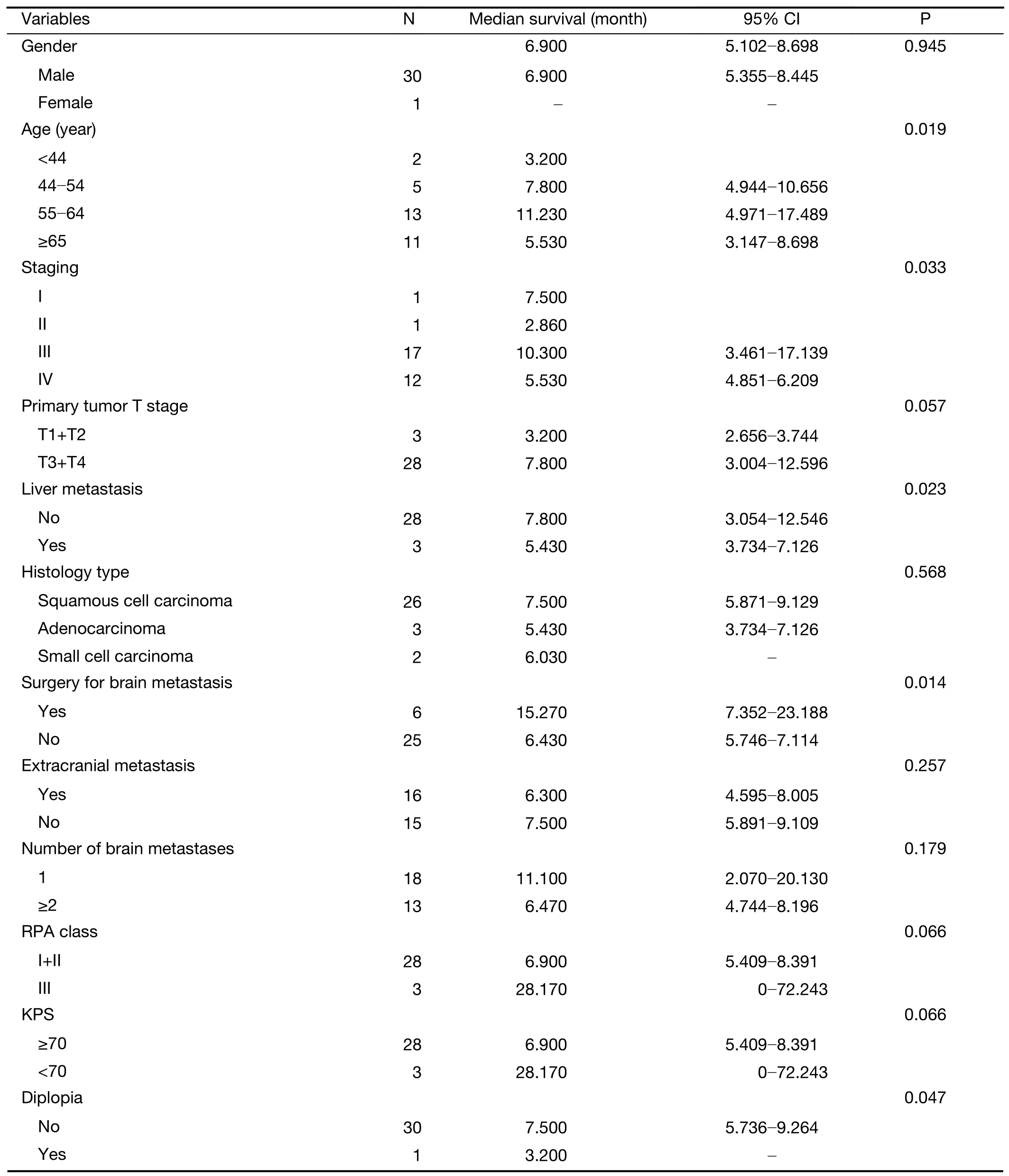
Table 2 Factors that affect survival time after brain metastasis as analyzed with univariate analysis
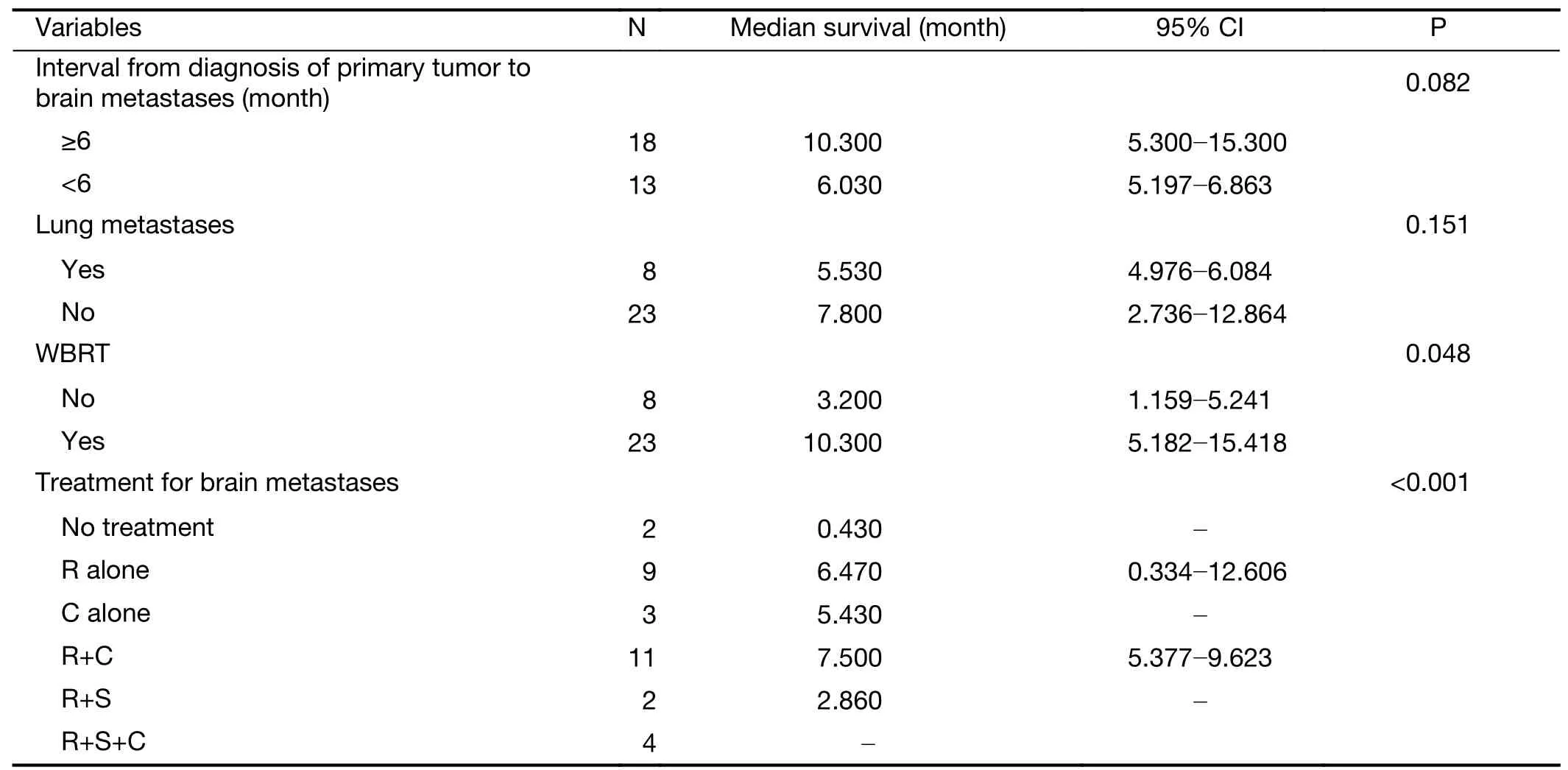
Table 2 (continued)
BMEC is rare,with an estimated incidence of 0.4%-5.1%in patients with EC (21-23).The frequency of BMEC was 0.3% in the current study,which was lower than the reported incidence.This finding could be because many asymptomatic cases of BMEC were missed during the follow-up examination as brain imaging of EC patients is not a mandatory test at Zhejiang Cancer Hospital.
The median TTBM was calculated and the impact of various clinicoradiological characteristics on TTBM was analyzed.The results showed that the stage of primary esophageal tumors and the length of primary esophageal lesions significantly affect the risk of BMEC development.It was reported that 26 (81%) of 32 BMEC patients had EC of grade III (lesion invaded the adventitia with chest lymph node positivity) or grade IV (distant metastasis),implying that a late stage of the disease may be a risk factor for brain metastases (23,24).In the present study,51.6% of patients had distant metastases outside the brain when BMEC was diagnosed.Moreover,patients with stages III and IV disease had significantly shorter TTBM compared to those with stage I/II disease (7.67vs.38.4 months,P=0.017).
The pathological type of EC appears to affect TTBM.A study showed that there was no association between the susceptibility to brain metastasis and the primary tumor pathology type (25).In the present study,the majority of BMEC patients had esophageal squamous cell carcinoma(83.9%).Previous studies have shown that the predominant pathological types of BMEC are squamous cell carcinoma in Asian countries and adenocarcinoma in Western countries (22,23,25).The incidence of brain metastases in small cell EC has been reported to be high in Japanese studies,probably due to the high incidence of small cell EC(39 of 44 cases were small cell carcinomas) (19,23).Herein,brain metastases in small cell EC accounted for 2% of cases.The median TTBM for squamous cell carcinoma was 9.73 months.There were significant differences in TTBM among the three types of EC (squamous cell carcinoma,adenocarcinoma,and small cell types).We could not determine whether this finding has real significance because the 10,043 EC patients in the study were not classified pathologically due to multiple factors.
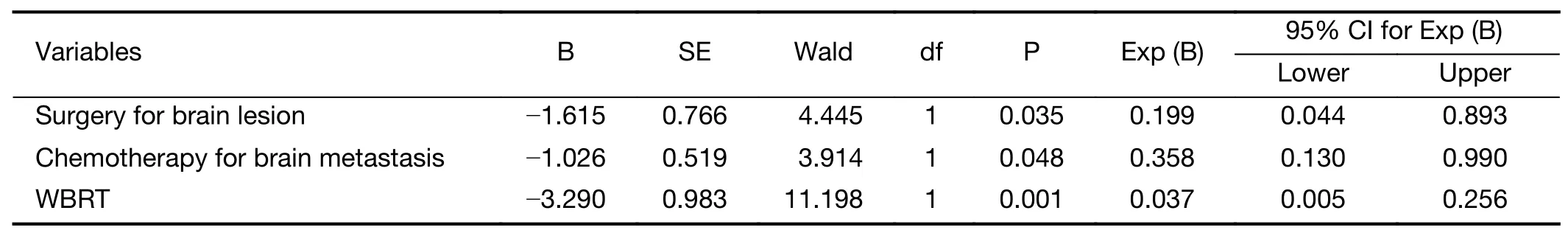
Table 3 Factors that affect survival time after brain metastasis as analyzed with proportional hazards model
Although local invasion and blood stream dissemination are the main causes of BMEC,the dissemination theory of lung metastasis could also be another risk factor for BMEC(23,25-27).It is believed that lesions actually exist in the lungs,but are too small to be detected by current imaging techniques (23,28).Another hypothesis for brain metastasis is the theory of propagation of tumor cells through the spinal venous plexus proposed by Batson (23,25,26).The most common organ for distant metastasis in our study was the lungs [8 cases (25.8%)].This is consistent with the findings reported by Weinberget al(26%) (22).In this study we did not observe any relation between lung metastasis and BMEC.However,patients without bone and liver metastases had longer TTBM than those with bone/liver metastases (P=0.027 and P=0.008).Additionally,patients who received primary chemotherapy or primary surgery and chemotherapy for esophageal tumor had significantly shorter TTBM (P=0.05 and P=0.016).We suspect that patients who received chemotherapy had a higher stage of disease with presence of micro-metastasis,which initially went undetected.The extensive metastasis would certainly increase the risk of brain metastasis.
High RPA grades are often associated with poor prognosis and are predictors of poor survival in all pathological types of brain metastases (29,30).However,we found that difference in survival time between patients with RPA grades I/II and those with RPA III was not statistically significant (P=0.066).
Patients with a single brain metastasis have a better prognosis and longer TTBM than those with multiple brain metastases (19).However,the survival times for BMEC patients with single and multiple lesions were similar in our study.We believe that most of brain lesions were too small to be detected on imaging examinations.In addition,we did not have the pathological reports to determine whether patients with single metastatic tumors had meningeal involvement.Active treatment of BMEC has been reported to improve the prognosis (31).We found the median survival time was 6.47 months after diagnosis of brain metastases,which is different from the findings in a previous study (3.9 months) (23).Other studies have indicated that the median survival time of brain metastases in 14 patients ranged from 2.0 months to 25 months(19,32).Patients who received a combination of radiotherapy and chemotherapy for BMEC had the longest survival time of 7.5 months.However,patients with the longest survival were those who were treated with WBRT,as well as patients with multiple lesions treated with surgery,chemotherapy,and radiotherapy,whose survival periods were 28.17 months and 148.13 months,respectively.These data indicated that BMEC patients who had received chemotherapy or surgery had longer survival times.A previous study cautiously inferred that the use of aggressive treatments can improve survival for patients with multiple lesions (31).
Our team had previously conducted a study on BMEC,as the research on this topic is limited and was mostly performed in Japan and the United States (a total of 26 cases) (33).We had also reviewed the relevant medical records for patients with BMEC to determine whether there were similarities between the radiological findings and clinical characteristics.However,because the sample size was small,the reference value for our conclusion was limited (34).
Conclusions
In the present study,we identified various factors that affect TTBM and the survival time after diagnosis of BMEC.Despite clinicopathological factors,the survival time for patients with single brain metastasis was improved with multimodal treatment.However,future studies with larger sample sizes are required to validate the findings of this study.
Acknowledgements
This study was supported by grants from the Public Technology Application Research Project of the Science and Technology Agency of Zhejiang Province,China (No.2017C33084),the Medical Talents Research Project of Zhejiang Province, China (No. 2016RCA005) and Zhejiang Medical and Health Science and Technology Project (New Technology Product R &D Project:No.2020PY001).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
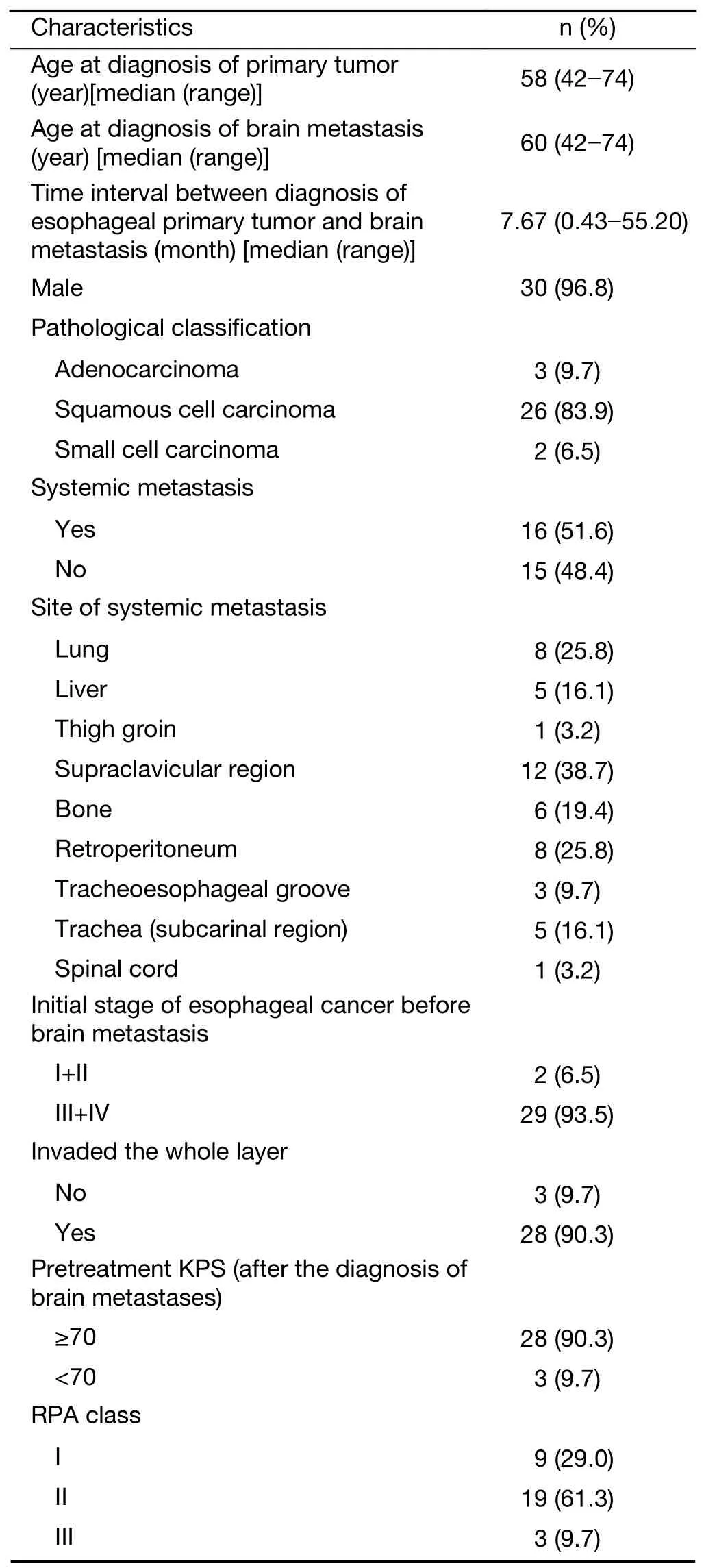
Table S1 Clinical characteristics of patients with BMEC (N=31)
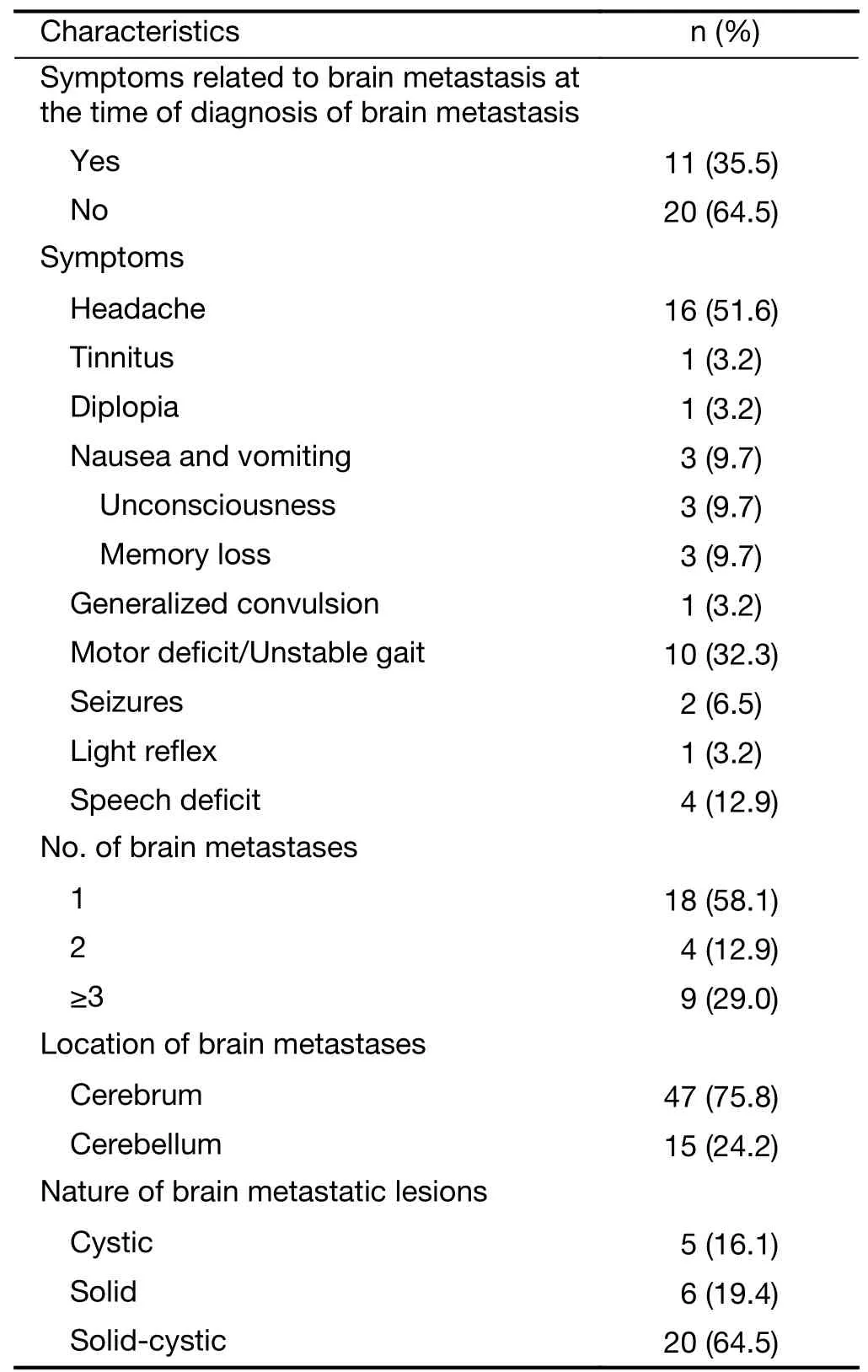
Table S1 (continued)
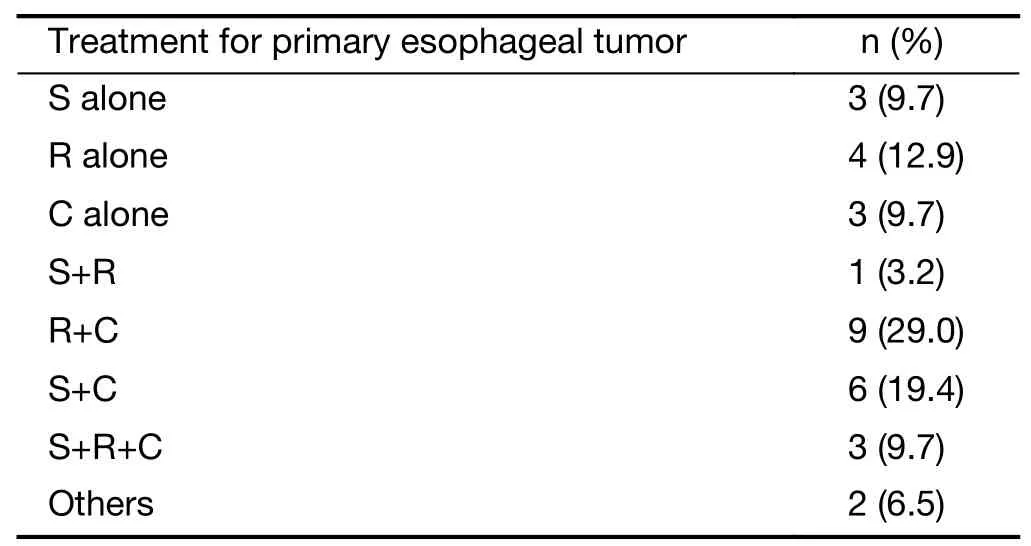
Table S2 Number of patients with brain metastases based on different treatments they received for primary esophageal tumors

Table S3 Data for BMEC patients treated with different methods
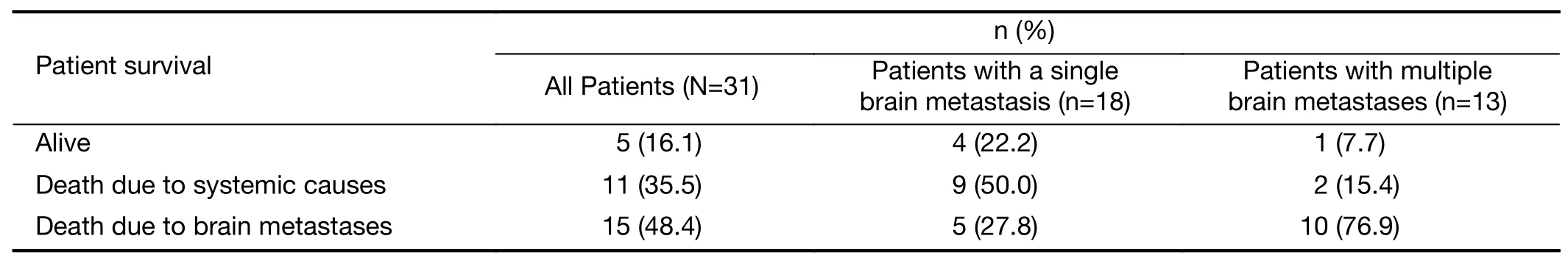
Table S4 Survival of patients with brain metastasis in follow-up period
杂志排行
Chinese Journal of Cancer Research的其它文章
- Separate lateral parametrial lymph node dissection improves detection rate of parametrial lymph node metastasis in early-stage cervical cancer:10-year clinical evaluation in a single center in China
- Hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastasis:A multicenter propensity scorematched cohort study
- Development and validation of prognostic nomogram based on log odds of positive lymph nodes for patients with gastric signet ring cell carcinoma
- Signatures within esophageal microbiota with progression of esophageal squamous cell carcinoma
- Oral microbiome and risk of malignant esophageal lesions in a high-risk area of China:A nested case-control study
- Current epidemiology of pancreatic cancer:Challenges and opportunities