Therapeutic efficacy of traditional Chinese medicine compound in the treatment of membranous nephropathy: A systematic review and metaanalysis
2021-01-04FeiGaoZeZeWangBingYangJinChuanTan
Fei Gao, Ze-Ze Wang, Bing Yang, Jin-Chuan Tan✉
1.Hebei University of Traditional Chinese Medicine, Shijiazhuang 050200 2.Hebei Traditional Chinese Medicine Hospital, Shijiazhuang, 050011
Keywords:Chinese herbal compound Hormone Immunosuppressant Membranous nephropathy Systematic review Meta-analysis
ABSTRACT Objective: Systematic review of the clinical efficacy of medicinal nephropathy in the treatment of membranous nephropathy with the addition of traditional Chinese herbal compound on the basis of hormone and immunosuppressive therapy. Methods: Computer search of China Knowledge Network, Wanfang Database, Weipu Database, China Biomedical Database, PubMed Database、Embase Database、Cochrane Database, collect clinical research on Chinese medicine compound + hormone + immunosuppressive therapy for MN, delete duplicate literature, eliminate non-conformity by reading topic, abstract and full text The literature was included in the exclusion criteria, the data was extracted from the included literature, and the meta-analysis was performed using the stata14.0 software package. Results: The top 6 Chinese medicines used were Astragalus, Poria, Atractylodes, Salvia, Angelica and Chinese Yam. The use of traditional Chinese medicine in the treatment of patients with MN on the basis of hormone and immunosuppressive therapy can improve clinical efficacy[OR=2.90,95%CI(2.27, 3.70),P < 0.00001]and TCM symptom efficacy [OR=3.10,95%CI(1.91, 5.05),P < 0.00001], improved TCM syndrome scores [SMD=-0.93,95%CI(-1.34, -0.52),P < 0.00001], reduced 24-hour urine protein levels[SMD=-0.90,95%CI(-1.23, -0.57),P < 0.00001], increased plasma albumin levels[SMD=1.22,95%CI(0.86, 1.58),P = 0.000], decreased blood lipid TC levels[SMD=-0.69,95%CI(-0.98, -0.39),P< 0.00001], lowering blood lipid TG levels[SMD=-0.75,95%CI(-1.09, -0.41),P < 0.0001], in improving renal function BUN levels[SMD=-0.56,95%CI(-0.97, 0.14),P = 0.008] and Scr levels [SMD=-0.58,95%CI(-0.89, -0.27),P = 0.0002], reducing the incidence of adverse reactions [OR=0.25,95%CI(0.17, 0.36),P < 0.00001]. Egger and harbord test results suggest that some indicators have publication bias. Conclusion: The traditional Chinese medicine used is mainly jaundice, and the traditional Chinese medicine for replenishing qi and activating blood is used more frequently. In the basic application of hormone + immunosuppressive agents, Yiqihuoxue Chinese medicine has a good effect on MN, but it is limited to the quality of the included literature. The conclusion needs to be verified by more high-quality studies.
1. Introduction
With the rapid development of society, the incidence of primary glomerular disease in China is increasing year by year. Membranous nephropathy (MN) is the main pathological type, and a large amount of proteinuria is the main clinical manifestation [1]. Some patients can recover, but the condition of MN is easy to repeat [2]. A large amount of persistent proteinuria will eventually progress to end-stage renal disease. At present, hormones combined with immunosuppressants, are often used clinically to reduce patients' urine protein levels, thereby protecting renal function and delaying
its progression to end-stage renal disease [3]. However, there are still many disadvantages in clinical treatment, such as different types of immunosuppressants, dose size, and length of treatment will significantly affect the treatment effect, adverse reactions and relapse probability [4].
Research reports that the efficacy of TCM regimen in treating MN is comparable to that of using hormones plus immunosuppressants, and it has obvious advantages in improving and protecting patients' renal function, and the incidence of adverse events in TCM regimen is lower, and TCM is relatively safer [5]. However, more research evidence at present confirms the efficacy and safety of using Chinese herbal compound to treat MN based on the use of hormone plus immunosuppressive agents, showing that Chinese herbal compound can improve clinical efficacy and TCM symptoms and reduce the incidence of adverse reactions [6-8]. However, clinical studies have different efficacy and scattered research, lacking of evidence-based medical evidence. Therefore, this study is devoted to providing evidence-based evidence on the clinical efficacy and safety of Chinese herbal compound combined with hormone immunosuppressive agents in the treatment of MN.
2. Materials and methods
2.1 Literature search
Choose 5 keywords in China Knowledge Network (CNKI), China Biomedical Literature Database (CBM), Wanfang Medical Journal Database (Wan-fang), and VIP Medical Database (VIP) databases: membranous nephropathy, Membranous nephrotic syndrome, membranous glomerulonephritis, membranous glomerulopathy, Heymann nephritis; Foreign literatures were selected as "Glomerulonephritis, Membranous", Membranous nephropathy, Membranous glomerulopathy, Membranous nephrotic syndrome, membranous glomerulonephritis as keywords to search in PubMed, Embase, Cochrane databases.
2.2 Inclusion and exclusion criteria
Inclusion criteria:①Research object: patients with idiopathic MN (diagnosed by renal pathological biopsy), the patient's age, sex, course, pathological stage and 24h urine protein quantitative level are not limited;②The test type is selected as a randomized controlled trial (RCT);③Intervention measures: Chinese medicine compound plus hormone plus immunosuppressive agent vs hormone plus immunosuppressive agent, the types of hormones and immunosuppressive agents are not limited and the course of treatment is not limited; ④Inclusion studies refer to the same criteria to evaluate the outcome indicators; exclusion criteria: ①Related literature with incomplete data or unavailable data; ②Related literature with duplicate content published by the same researcher.
2.3 Data extraction and literature quality evaluation
The data were extracted by two researchers, such as the researcher's name、publication time、number of cases、gender、age、intervention measures、course of treatment、outcome indicators, etc. If there were disagreements, the two researchers decided to include them after discussion. The literature quality evaluation is based on the Cochrane Collaboration Network bias risk evaluation standard. Randomization, blinding, loss of follow-up, publication bias, and other aspects of the quality of the included studies were evaluated with "low risk", "unclear risk", and "high risk" ) ". The more low-risk items, the lower the risk of bias and the higher the quality of the study.
2.4 Statistical methods
Meta analysis was conducted through the commonly used RevMan 5.3 software. Continuous variables are expressed by standardized mean difference (SMD) and its 95% confidence interval (CI), and binary variables are expressed by relative risk (OR) and its 95% confidence interval (CI). The heterogeneity test uses P <0.10 and I2> 50% as the criterion of significance. When P> 0.10 and I2<50%, it indicates that the heterogeneity is small and the fixed effect model is used; otherwise, the clinical heterogeneity is excluded. In the case of random effects model; use stata14.0 software to draw a funnel chart to judge the publication bias. The continuity variable uses the Egger method, and the binary classification variable uses the harbord method.
3. Results
3.1 Literature screening
A total of 27,753 related literatures were retrieved in this study, including 1711 literatures in CNKI、2493 literatures in CBM、3182 literatures in Wan-fang、2218 literatures in VIP、8171 literatures in PubMed、9592 literatures in Embase and 386 literatures in Cochrane. Firstly, 11124 literatures were deleted using Note express software and manual checking; secondly, 16485 literatures were deleted by reading titles and abstracts; finally 113 literatures were deleted from the full text; 31 literatures were finally included.

Figure 1 Flowchart of literature screening
3.2 Basic characteristics of included studies
Finally included 31 RCT studies [5-23], a total of 2017 MN patients, including 983 cases of a control group by giving hormones and immunosuppressants, and 1034 cases of Chinese herbal compound combined with hormones and immunosuppressants. The pathological stages of MN are in stagesⅠ-Ⅳ. The course of treatment varies from 1-18 months. The reported that the test group and the control group had no statistical significance in terms of age, gender, disease course, and pathological stage in 31 included studies. The basic information specifically included in the study is shown in Table 1.

Table 1 Basic information included in the study
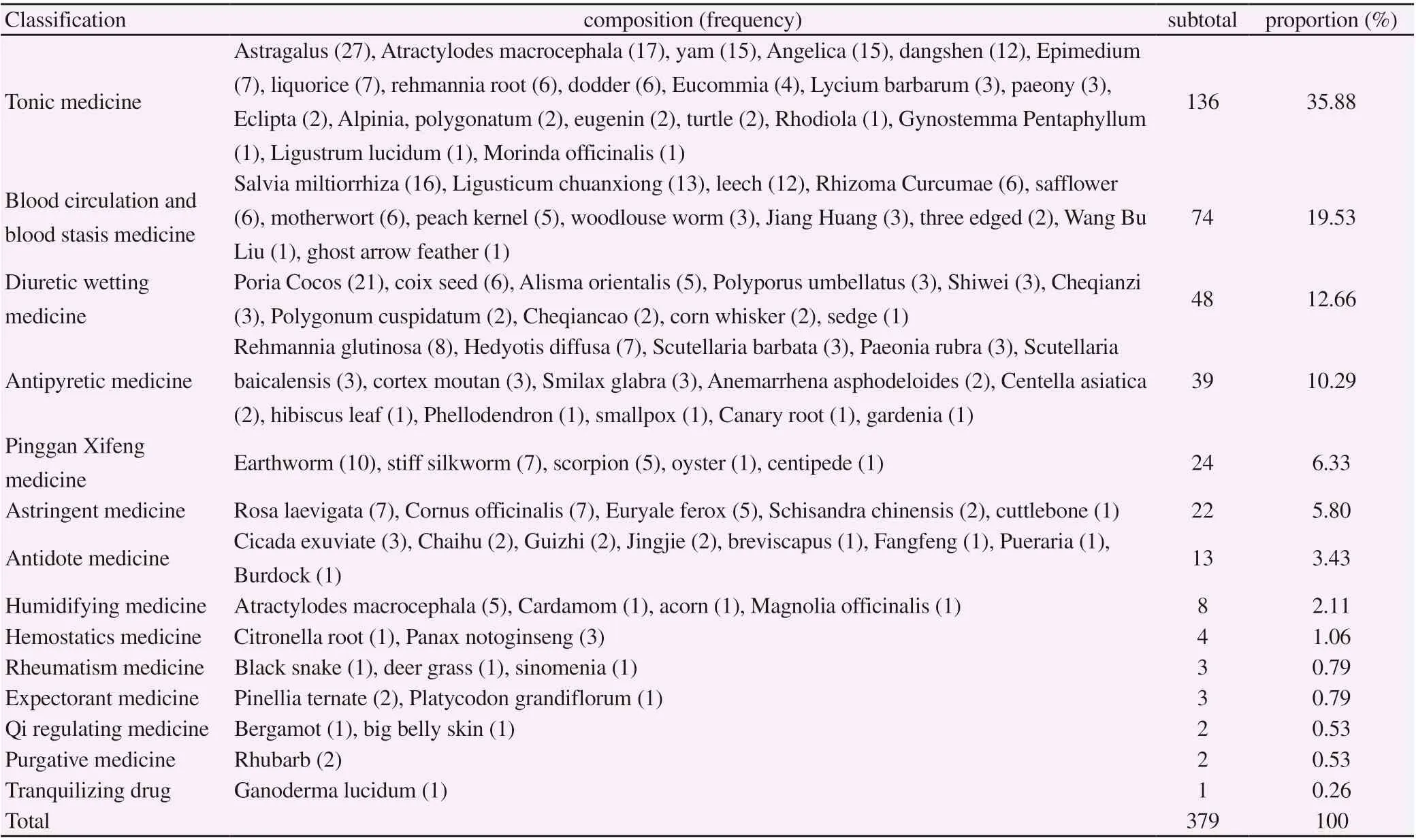
Table 2 Drug classification and frequency of use
3.3 The classification and frequency of the use of Chinese herbal medicines in the study

Figure 2 Network diagram of drug association rules
Among the 31 traditional Chinese medicine prescriptions, the least used Chinese medicine is 5 flavors, and the most used is 20 flavors. The total using frequency is 379 and the top 6 Chinese medicines used are Astragalus、Poria、Atractylodes、Salvia、 Angelica and yam. “buxu” medicines and “huoxuehuayu”medicines are often used. Using R 3.5 software to analyze the association rules of 31 traditional Chinese medicine prescriptions, the results showed that: Astragalus、Poria、Angelica、Chuanxiong、 yam and Salvia miltiorrhiza were highly correlated. The above content suggests that the traditional Chinese medicine treatment of MN is mainly based on “Yiqi Huoxue” medicine.
3.4 Inclusion of literature quality evaluation
The 31 included studies all mentioned random grouping, but only 10 studies indicated specific random methods [7, 15, 16, 18, 19, 21, 25, 26, 31, 32]. None of the included studies reported the implementation of allocation concealment and blinding methods and it may affect the results in the intervention of the experimental group on the basis of treatment with hormones and immunosuppressants combined with Chinese herbal medicines. Four studies reported Lost interview data and missing data. Other information included in the study was incomplete and it was difficult to judge whether the data was complete [15, 18, 19, 33] . The quality evaluation of the included studies is shown in Figure 3.

Figure 3 Quality evaluation of included studies
3.5 Meta analysis of the efficacy and safety of Chinese herbal medicines treatment of membranous nephropathy
3.5.1 Clinical efficacy
27 studies reported clinical efficacy [6, 7, 9, 10, 12-23, 25-28, 30-36]. There was no statistical heterogeneity between the included studies (P = 0.97, I2= 0.00%) and a fixed-effects model was used for Meta analysis. The results showed that the clinical efficacy of the Chinese herbal medicines combined with hormones and immunosuppressants in the experimental group in the treatment of MN was better than the control group [OR = 2.90, 95% CI (2.27, 3.70), P <0.00001], Figure 4.

Figure 4 Meta-analysis forest graph of clinical efficacy
3.5.2 TCM symptom efficacy and symptom score
Nine studies have reported the efficacy of TCM symptoms [8, 10, 11, 17, 20, 28, 29, 31]. There was no statistical heterogeneity between the included studies (P = 0.99, I² = 0.00%), and a fixed-effect model was used for Meta analysis. The results showed that the curative effect of Chinese herbal medicines combined with hormone plus immunosuppressant on MN was better than that of control group [OR = 3.10, 95% CI (1.91, 5.05), P <0.00001], see Figure 5-A. Eight studies reported TCM symptom scores [8, 10, 11, 17, 20, 29, 31]. The heterogeneity between the included studies was large (P = 0.0005, I² = 73%) and a random effects model was used for Meta analysis. The results showed that the curative effect of traditional Chinese medicine combined with hormone plus immunosuppressant on MN was better than that of control group [SMD = -0.93, 95% CI (-1.34, -0.52), P <0.00001], Figure 5-B.

Figure 5-A Meta-analysis forest diagram of the efficacy of TCM symptoms

Figure 5-B Meta analysis forest map of TCM syndrome
3.5.3 24-hour urine protein (24h-upro)
30 studies reported 24h-upro [6-11, 13-36]. The heterogeneity between the included studies was large (P <0.00001, I² = 91%) and a random effects model was used for Meta analysis.The results showed that the combination of Chinese herbal compound combined with hormone and immunosuppressant was superior to the control group in reducing the 24h-upro level [SMD = -0.90, 95% CI (-1.23, -0.57), P <0.00001], Figure 6.

Figure 6 Meta-analysis forest map of 24-hour urine protein
3.5.4 Plasma albumin (ALB)
29 studies reported ALB [6-8, 10, 11, 13-36]. The heterogeneity between the included studies was large (P <0.00001, I² = 92%) and a random effects model was used for Meta analysis. The results show that Chinese herbal compound combined with hormones and immunosuppressants is superior to the control group in improving ALB levels [SMD = 1.22, 95% CI (0.86, 1.58), P = 0.000], Figure 7.

Figure 7 Meta-analysis forest map of ALB
3.5.5 Renal function (BUN, Scr)
16 studies reported BUN [7, 8, 11, 13, 15-17, 19-21, 24-26, 32, 33, 36]. The heterogeneity among the included studies was large (P <0.00001, I² = 90%) and a random effects model was used for Meta analysis. The results showed that the combination of traditional Chinese medicine combined with hormones and immunosuppressants improved the BUN level of patients with MN better than the control group [SMD = -0.56, 95% CI (-0.97, 0.14), P = 0.008], Figure 8-A; 23 items The study reported Scr [6-8, 11, 13-17, 19-22, 24-26, 28, 30-34, 36]. The heterogeneity among the included studies was large (P <0.00001, I² = 88%) and a random effects model was used for Meta analysis. The results showed that the combination of traditional Chinese medicine combined with hormones and immunosuppressants improved the Scr level of MN patients [SMD = -0.58, 95% CI (-0.89, -0.27), P = 0.0002], Figure 8-B.

Figure 8-A Meta-analysis forest map of BUN

Figure 8-B Meta-analysis forest map of Scr
3.5.6 Blood lipids (TC, TG)
Twenty-six studies reported TC [6, 7, 10, 11, 14-20, 22, 24-36]. The heterogeneity between the included studies was large (P <0.00001, I² = 88%) and a random effects model was used for Meta analysis. The results showed that the combination of Chinese herbal medicine combined with hormone and immunosuppressant was superior to the control group in improving the TC level of MN patients [SMD = -0.69, 95% CI (-0.98, -0.39), P <0.00001], Figure 9-A; 26 studies reported TG [6, 7, 10, 11, 14-20, 22, 24-36]. The heterogeneity among the included studies was large (P <0.00001, I²= 90%) and a random effects model was used for Meta analysis. The results showed that the combination of traditional Chinese medicine combined with hormone and immunosuppressant was superior to the control group in improving the TG level [SMD = -0.75, 95% CI (-1.09, -0.41), P <0.0001], Figure 9-B.

Figure 9-A Meta-analysis forest map of TC

Figure 9-B Meta-analysis forest map of TG
3.4.7 Adverse reactions
24 studies reported adverse reactions [6-14, 16-20, 23-25, 28-31, 33-35]. The heterogeneity among the included studies was small (P = 0.06, I²= 36%) and a fixed-effects model was used for Meta analysis. The results showed that the combination of Chinese herbal medicine combined with hormone and immunosuppressant was superior to the control group in reducing adverse reactions in patients with MN [OR = 0.25, 95% CI (0.17, 0.36), P <0.00001], Figure 10.

Figure 10 Meta analysis forest map of adverse reactions
3.5 Publishing bias
The indicators of binary classification such as clinical efficacy、TCM symptom efficacy and adverse reactions were tested for publication bias using the harbord method. The results showed that there was no publication bias for clinical efficacy and adverse reaction indicators (P> 0.05); there was publication bias for the efficacy of TCM symptoms (P <0.05). Continuous variables such as TCM symptom scores、BUN、24-upro、TC and TG were tested for publication bias using the Egger method. The results showed that: BUN、Scr、TC and TG indicators had no publication bias (P> 0.05); TCM syndrome score and 24-upro had publication bias (P <0.05). The funnel chart of Egger and harbord test is shown in Figure 11, taking the clinical efficacy and 24-upro funnel chart as examples. There are publication biases in the study results, suggesting that there may be unpublished negative results, which may be related to the difficulty of publishing negative results.

Figure 11 Inconsistency test of harbord method and Egger method
4. Discussion
MN is currently the second largest primary glomerular disease after IgA nephropathy In China, but the risk of IgA nephropathy is relatively stable, while MN is growing at a rate of 13% per year [1]. Affected by the environment in North China, MN has become the main pathological type of primary glomerular disease [1]. MN is a slow and progressive kidney disease with a long treatment period and a large individual difference in treatment effect and a prognosis that is easy to repeat. Patients need to take drugs all year round. There are toxic and side effects and drug resistance, which causes multiple pressures on the patient's economy and spirit safe, so effective treatment drugs or methods are urgently needed to be resolved. [4]
In recent years, Chinese medicine has shown its great advantages in the treatment of membranous nephropathy. Professor Deng Yueyi 's team reported that the effect of Chinese medicine “Shenqimoshen keli” son reducing urinary protein levels in patients with MN is comparable to immunosuppressants and no adverse reactions Occurred [37]. On the basis of Western medicine treatment, the use of traditional Chinese medicine to treat MN has been recognized by more and more colleagues in the Western medicine community for its attenuating and synergistic effects. There are also many reports on its clinical research and rich practical experience [13, 19, 21, 22 , 24, 26]. In addition, Chinese medicine has a rich theoretical basis for the treatment of MN. The three-joke theory, turbidity theory and collateral disease theory of traditional Chinese medicine have achieved satisfactory results in the treatment of MN [38-40].
MN has a large amount of proteinuria as its main clinical manifestation. In addition to the main symptoms of lower extremity edema and low back pain, MN patients will also experience palpitations, insomnia, dreaminess, frequent urination, spontaneous sweating, fatigue, irritability, depression, bloating, weight and stool deficiencies. However, the clinical efficacy is mostly based on the level of urine protein. The evaluation of drugs or treatment options is measured by the amount of urine protein. The index of clinical cure is also to observe the disappearance of urinary protein and less attention is paid to the improvement of patients' other symptoms [38]. In particular, patients use a lot of hormones and immunosuppressants for a long time and the frequency of secondary symptoms is higher. Although these symptoms will not have a serious impact on the patient's prognosis, these symptoms will directly affect the patient's quality of life and treatment experience and have a direct impact on the patient's confidence in disease resistance and treatment dependence. Traditional Chinese medicine has obvious advantages in improving patients' accompanying symptoms through syndrome differentiation and symptomatic treatment. It not only reduces the urinary protein level of MN patients but also improves the symptoms of traditional Chinese medicine and reduces the incidence of adverse reactions. The effect shows that 1+1 is greater than 2. This is consistent with the results obtained in this study.
27 of the 31 included studies included Chinese herbal medicines containing astragalus. Astragalus is the sacred medicine for nourishing qi, which can not only benefit qi and nourish the kidney but also promote blood circulation and nourish the blood. In addition, Poria, yam, angelica, salvia miltiorrhiza and Chuanxiong are more frequently used and closely related. The above 6 flavors of traditional Chinese medicine are mainly based on Yiqi Huoxue, Poria strengthening spleen and dehumidifying, Chinese yam strengthening spleen and kidney, angelica nourishing blood and promoting blood circulation, Salvia miltiorrhiza and blood stasis, Chuanxiong activating blood circulation, which is also consistent with the pathogenesis of MN: Qi deficiency blood stasis. Deficiency of lung qi means that the imbalanced water overflows to the skin. Deficiency of spleen qi means that water loss often occurs as edema. If the kidney qi is deficient, it will seal the reservoir and lose the division, and make a precise bet. Righteousness keeps the inside、evil is not dry、 qi deficiency is susceptible to external evil and prolonged phlegm, blocking the veins and forming blood stasis; chronic illness will be virtual and chronic illness will stasis. Therefore, blood stasis is not only the causative factor of MN but also its important pathological products; damp heat and blood stasis causes the recovery of the disease slowly. The blood of patients with MN has hypercoagulable state, dyslipidemia and hemodynamic abnormalities. At the same time, the deposition of glomerular basement membrane immune complexes is observed. These performances are closely related to blood stasis. The above drugs are combined with Astragalus membranaceus, which can replenish the lung and regulate the water channel, invigorate the spleen, transport the blood and eliminate the edema, invigorate the kidney, strengthen the essence and stop the turbid urine, and invigorate the blood, activate the blood and remove the stasis.
In the 31 articles included in this study, some researchers did not elaborate on the participants' age、course of disease、MN pathological stage and 24h-upro level, these factors will affect the treatment effect and bias the analysis results. Although the included study groups all used traditional Chinese medicine combined with hormones plus immunosuppressants to treat MN, but it will also bias the analysis results that includes the types of hormones、the initial dose and duration of treatment、the types of immunosuppressants and the cumulative doses. At the same time, it can be seen from the dosage and course of treatment of hormones and immunosuppressants that the design of the study included is not scientific enough and the drugs in some studies have not been used strictly in accordance with clinical guidelines. Moreover, the sample size of the included literature studies is relatively small and only a few studies have pointed out specific random methods. The included studies have not stated in terms of allocation concealment and blind method implementation. Therefore more large-scale double-blind randomized controlled trial evidence is needed to support and verify the effectiveness and safety of using traditional Chinese medicine to treat MN on the basis of hormone and immunosuppressive therapy.
杂志排行
Journal of Hainan Medical College的其它文章
- Mechanism of therapeutic effects of Huangbo on ureteral stones based on network pharmacology
- Molecular mechanism of Turmeric in the treatment of liver cancer based on network pharmacology
- Meta-analysis of randomized controlled trials of traditional Chinese medicine in the treatment of obstructive sleep apnea syndrome
- Correlation between CT dynamic enhanced scanning parameters and serum tumor markers before and after radiofrequency ablation in patients with lung cancer
- Effects of fumigation and washing with Shujin Huoluo decoction combined with Duhuo Parasitic decoction on TIMP-1 and PON1 levels in KOA patients
- The effect of Xuebijing on burn patients and its effect on pain and wound healing
