Correlation between CT dynamic enhanced scanning parameters and serum tumor markers before and after radiofrequency ablation in patients with lung cancer
2021-01-04YiWangXuLiangRuiYuZhan
Yi Wang, Xu Liang, Rui-Yu Zhan
1.Department of Radiology, Zigong Fourth People' s Hospital in Sichuan Province, Zigong, Sichuan Province, 643000 China 2.Department of Radiology, Sichuan Cancer Hospital, Chengdu, Sichuan Province, 610041 China
3.Department of Oncology, Zigong Fourth People' s Hospital in Sichuan Province, Zigong, Sichuan Province, 643000 China
Keywords:Lung cancer Radiofrequency ablation CT dynamic enhanced scanning Tumor marker
ABSTRACT Objective: To study the correlation between CT dynamic enhanced scanning parameters and serum tumor markers before and after radiofrequency ablation in patients with lung cancer. Methods: 60 patients with advanced non-small cell lung cancer who were treated in this hospital between January 2015 and January 2017 were divided into control group (n=30) and observation group (n=30) by random number table method. Control group received conventional intravenous chemotherapy, and observation group received intravenous chemotherapy combined with radiofrequency ablation. The differences in CT dynamic enhanced scanning parameter levels and serum tumor marker contents were compared between the two groups of patients before and after treatment. Pearson test was used to evaluate the correlation between CT dynamic enhanced scanning parameters and serum tumor marker contents in patients with advanced non-small cell lung cancer. Results: Before treatment, the differences in CT dynamic enhanced scanning parameter levels, non-organ-specific tumor marker contents and vascular tumor marker contents were not statistically significant between the two groups of patients (P>0.05). After treatment, CT dynamic enhanced scanning parameters PH and perfusion value levels of observation group were lower than those of control group (P<0.05); serum non-organ specific tumor markers CA125, CA153, CEA and CYFRA21-1 contents of observation group were lower than those of control group; serum vascular tumor markers VEGF, Ang-2, HIF-1α and MMP-9 contents were lower than those of control group (P<0.05). Pearson test showed that CT dynamic enhanced scanning parameters PH and perfusion value levels in patients with non-small cell lung cancer were positively correlated with serum non-organ specific tumor marker and vascular tumor marker contents. Conclusion: Adjuvant radiofrequency ablation can significantly reduce the tumor malignancy of patients with advanced non-small cell lung cancer.
1. Introduction
Non-small cell lung cancer is currently one of the malignant tumor diseases with the highest incidence, and for the patients who are not diagnosed in time and in advanced stage, choosing a therapy to furthest optimize the prognosis is the key of the clinical research [1-2]. Intravenous systemic chemotherapy is the most common way of conservative treatment for patients with malignant tumors, but the blood drug concentration is low in local tumor, and the excessive increase of drug dose can cause serious side effects, which make its application value limited. Radiofrequency ablation treatment is a new minimally invasive therapy for solid tumor, which introduces high-frequency magnetic field through the electrode and makes the temperature in local lesion tissue reach above 75℃ to induce tumor cell death [3-4]. At present, it is considered that radiofrequency ablation is suitable for tumor tissues with dense structure, and lung tissues have high current impedance and meet the relevant technical conditions. In this research, intravenous chemotherapy and radiofrequency ablation were used together for the treatment of patients with advanced non-small cell lung cancer, and the therapeutic effect was discussed from CT dynamic enhanced scanning parameter levels, serum tumor marker contents and other aspects, now reported as follows.
2. Information and methods
2.1 Case information
60 patients with advanced non-small cell lung cancer who were treated between January 2015 and January 2017 were collected and selected as the research subjects, and their families signed informed consent. The 60 patients were divided into control group (n=30) and observation group (n=30) by random number table method. There were 14 males and 16 females in the control group, and they were 41-78 years old; there were 15 males and 15 females in the observation group, and they were 43-76 years. The difference in gender and age distribution was not significant between the two groups (P>0.05), and the hospital ethics committee approved the study.
2.2 Inclusion and exclusion criteria
Inclusion criteria: (1) diagnosed with non-small cell lung cancer by pathological biopsy; (2) diagnosed for the first time and with advanced tumor stage; (3) receiving no systematic treatment before admission; (4) completing the whole treatment and cooperating with relevant examinations. Exclusion criteria: (1) allergic to contrast agent; (2) combined with severe cardiac, hepatic or renal insufficiency; (3) combined with systemic infectious diseases; (4) combined with primary malignant tumors of other tissue viscera.
2.3 Therapy
Control group received routine intravenous chemotherapy. Observation group received radiofrequency ablation combined with intravenous chemotherapy, which was as follows: CT scan (supine position) was conducted at first, the skin surface was marked, ECG monitoring was connected, general anesthesia was started, disinfection and draping were done, 1% lidocaine (Guangxi Nanning Baihui Pharmaceutical Group Co., Ltd., approved by H45020569) 5mL was used for puncture and local anesthesia, the RF needle was guided by CT and inserted in the lesion, the needle tip was adjusted to best position, radiofrequency electrode was connected for continuous 12 min of ablation, saline was injected through the injection hole of needle electrode during ablation to avoid local tissue charring, and the ablation edge should cover 05~1.0cm from tumor lesion edge. CT scan was conducted again, and the tumor ablation was completed if the lesion area was a large area of groundglass opacity in CT; then the puncture needle passage was ablated to prevent implantation metastasis, the puncture needle was removed and the treatment ended. ECG monitoring was performed within 24 hours after surgery.
2.4 Observation indexes
Before treatment and after treatment (1 week after chemotherapy for control group and 1 week after radiofrequency ablation for observation group), the two groups of patients underwent dynamic enhanced CT scanning to obtain the relevant parameters, including peak height (PH), time to peak (Tp) and perfusion values. At the same time point, 3-5mL of fasting cubital venous blood was extracted from the two groups of patients, anti-coagulated, let stand at room temperature for stratification and centrifuged to get the upper serum and store it at low temperature. IECL method was used to determine the serum contents of non-organ-specific tumor markers, including the carbohydrate antigen 125 (CA125), carbohydrate antigen 153 (CA153), carcinoembryonic antigen (CEA) and soluble cytokeratin 19 fragments (CYFRA21-1). Enzyme-linked immunosorbent assay method was used for determining the serum contents of vascular tumor markers, including vascular endothelial growth factor (VEGF), angiopoietin-2 (Ang-2), hypoxia-inducible factor 1α (HIF-1α) and matrix metalloproteinase-9 (MMP-9).
2.5 Statistical processing
CT dynamic enhanced scanning parameters, non-organspecific tumor markers and vascular tumor markers belonged to measurement data, were expressed as mean ± standard deviation and were compared by t test. Correlation was analyzed by Pearson test. Statistical software was SPSS24.0 and statistic P<0.05 indicated statistical significance in the differences.
3. Results
3.1 CT dynamic enhanced scanning parameters
Comparison of the differences in CT dynamic enhanced scanning parameters PH (HU), Tp (s) and perfusion value (mL/min) levels in the two groups of patients before and after treatment was as follows: before treatment, the differences in CT dynamic enhanced scanning parameters PH, Tp and perfusion value levels were not statistically significant between the two groups of patients (P>0.05). After treatment, CT dynamic enhanced scanning parameters PH and perfusion value levels of both groups were lower than those before treatment (P<0.05) whereas Tp levels were not significantly different from those before treatment (P>0.05), and CT dynamic enhanced scanning parameters PH and perfusion value levels of observation group were lower than those of control group (P<0.05) whereas Tp level was not significantly different from that of control group (P>0.05), shown in Table 1.
3.2 Non-organ-specific tumor markers
Comparison of serum non-organ-specific tumor markers CA125 (ng/mL), CA153 (ng/mL), CEA (ng/mL) and CYFRA21-1 (pg/mL) contents in the two groups of patients before and after treatment was as follows: before treatment, the differences in serum non-organspecific tumor markers CA125, CA153, CEA and CYFRA21-1 contents were not statistically significant between the two groups of patients (P>0.05). After treatment, serum non-organ specific tumor markers CA125, CA153, CEA and CYFRA21-1 contents of both groups were lower than those before treatment, serum non-organ specific tumor markers CA125, CA153, CEA and CYFRA21-1 contents of observation group were lower than those of control group, and the differences were statistically significant (P<0.05), shown in Table 2.
3.3 Vascular tumor markers
Comparison of serum vascular tumor markers VEGF (pg/mL), Ang-2 (ng/L), HIF-1α (ng/L) and MMP-9 (ng/mL) contents in the two groups of patients before and after treatment was as follows: before treatment, the differences in serum vascular tumor markers VEGF, Ang-2, HIF-1α and MMP-9 contents were not statistically significant between the two groups of patients (P>0.05). After treatment, serum vascular tumor markers VEGF, Ang-2, HIF-1α and MMP-9 contents of both groups were lower than those before treatment, serum vascular tumor markers VEGF, Ang-2, HIF-1α and MMP-9 contents of observation group were lower than those of control group, and the differences were statistically significant (P<0.05), shown in Table 3.
3.4 Correlation analysis
Pearson test showed that CT dynamic enhanced scanning parameters PH and perfusion value levels in patients with non-small cell lung cancer were positively correlated with serum non-organ specific tumor markers CA125, CA153, CEA and CYFRA21-1 contents as well as serum vascular tumor markers VEGF, Ang-2, HIF-1α and MMP-9 contents (P<0.05).
4. Discussion
The choice of therapy for patients with advanced non-small cell lung cancer will directly decide their prognosis, the applicationof intravenous chemotherapy alone is very popular in patients with advanced cancer, but the role of intravenous chemotherapy alone is limited in inhibiting the malignant biological behaviors of tumor, which is related to the low drug concentration in local tumor after intravenous medication, the normal tissue cell injury caused by chemotherapeutics, etc. Although patients with advanced tumors have lost the opportunity of radical surgery, more and more related local minimally invasive therapies have been developed and applied, and radiofrequency ablation is one of the most concerned at present. The treatment principle of radiofrequency ablation is to use electromagnetic waves to make diseased tissue cell ions vibrate and rub to produce heat, local temperature rises rapidly and can even reach above 75℃ (cancer cells will die at above 45℃), and local high temperature leads to tumor cell membrane fluidity and permeability damage, and eventually cause the internal environmental changes in cells and cell death [5-7]. In this study, radiofrequency ablation was introduced into the overall treatment scheme on the basis of intravenous chemotherapy so as to clarify the value of its adjuvant treatment.
Table 1 Comparison of CT dynamic enhanced scanning parameter levels in the two groups of patients before and after treatment ( ±s )
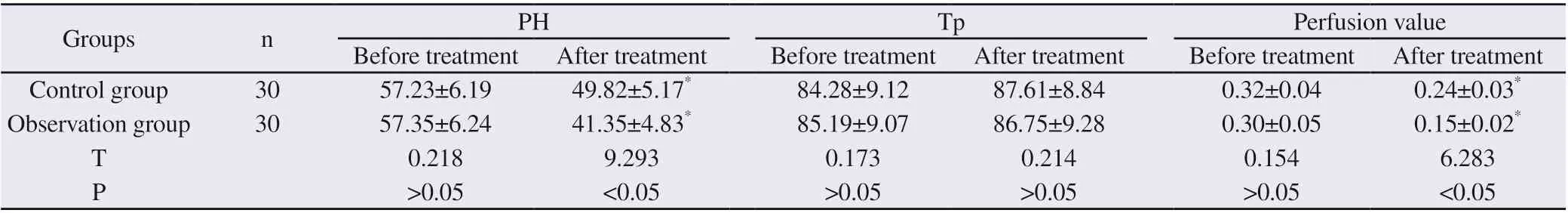
Table 1 Comparison of CT dynamic enhanced scanning parameter levels in the two groups of patients before and after treatment ( ±s )
Note: compared with same group before treatment, *P<0.05
Groups n PH Tp Perfusion value Before treatment After treatment Before treatment After treatment Before treatment After treatment Control group 30 57.23±6.19 49.82±5.17* 84.28±9.12 87.61±8.84 0.32±0.04 0.24±0.03*Observation group 30 57.35±6.24 41.35±4.83* 85.19±9.07 86.75±9.28 0.30±0.05 0.15±0.02*T 0.218 9.293 0.173 0.214 0.154 6.283 P>0.05 <0.05 >0.05 >0.05 >0.05 <0.05
Table 2 Comparison of serum non-organ-specific tumor marker contents in the two groups of patients before and after treatment ( ±s )
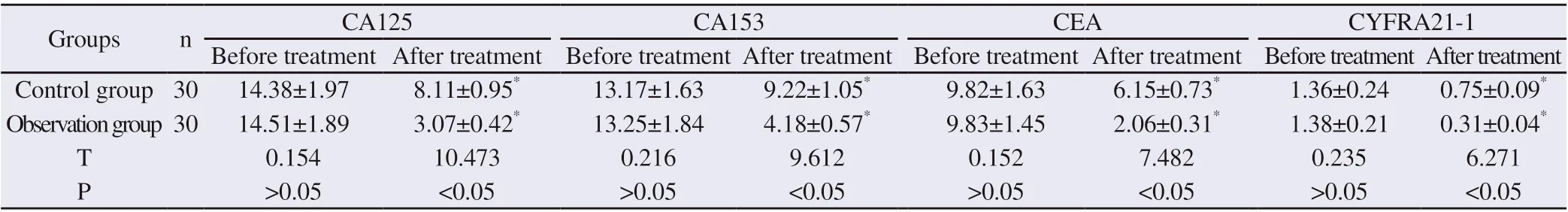
Table 2 Comparison of serum non-organ-specific tumor marker contents in the two groups of patients before and after treatment ( ±s )
Note: compared with same group before treatment, *P<0.05
Groups n CA125 CA153 CEA CYFRA21-1 Before treatment After treatment Before treatment After treatment Before treatment After treatment Before treatment After treatment Control group 30 14.38±1.97 8.11±0.95* 13.17±1.63 9.22±1.05* 9.82±1.63 6.15±0.73* 1.36±0.24 0.75±0.09*Observation group 30 14.51±1.89 3.07±0.42* 13.25±1.84 4.18±0.57* 9.83±1.45 2.06±0.31* 1.38±0.21 0.31±0.04*T 0.154 10.473 0.216 9.612 0.152 7.482 0.235 6.271 P>0.05 <0.05 >0.05 <0.05 >0.05 <0.05 >0.05 <0.05
Table 3 Comparison of serum vascular tumor marker contents in the two groups of patients before and after treatment (±s)
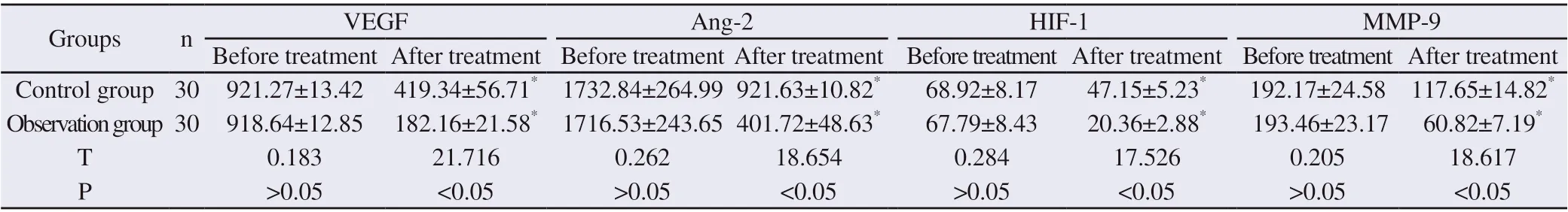
Table 3 Comparison of serum vascular tumor marker contents in the two groups of patients before and after treatment (±s)
Note: compared with same group before treatment, *P<0.05
Groups n VEGF Ang-2 HIF-1α MMP-9 Before treatment After treatment Before treatment After treatment Before treatment After treatment Before treatment After treatment Control group 30 921.27±13.42 419.34±56.71* 1732.84±264.99 921.63±10.82* 68.92±8.17 47.15±5.23* 192.17±24.58 117.65±14.82*Observation group 30 918.64±12.85 182.16±21.58* 1716.53±243.65 401.72±48.63* 67.79±8.43 20.36±2.88* 193.46±23.17 60.82±7.19*T 0.183 21.716 0.262 18.654 0.284 17.526 0.205 18.617 P>0.05 <0.05 >0.05 <0.05 >0.05 <0.05 >0.05 <0.05
Dynamic enhanced CT scan can reflect the blood supply status of local tumor in real time, and the more abundant the blood supply, the higher the malignancy of tumor tissue, and the higher the probability of long-term recurrence and distant metastasis [8]. PH, Tp and perfusion value are all basic parameters of dynamic enhanced CT scanning. PH, i.e. the maximum value of tumor enhancement, represents the blood flow intensity when tumor blood vessels are maximally filled; Tp represents blood flow rate, and the more blood supply, the smaller the Tp value; perfusion value is the most basic indicator to reflect the blood supply within the tumor, and the perfusion value is high if the vascular density inside the tumor is high and the blood flow speed is fast [9-10]. In this study, the differences in the levels of above dynamic enhanced CT scanning parameters were compared between the two groups of patients before and after treatment, and it was found that compared with those before treatment, PH and perfusion value levels of both groups decreased after treatment, showing that both treatments help to reduce the tumor blood supply to different extent; further compared with those of control group, PH and perfusion value levels of observation group were lower after treatment, it proves that adjuvant radiofrequency ablation can be more effective to reduce the tumor blood supply, and this is mainly directly related to its effects on directly killing tumor cells, causing local tissue coagulation necrosis and preventing the surrounding tissue from supplying blood to the tumor blood supply, and so on. In the study, Tp values did not change significantly before and after treatment, which may be because that its results is affected by contrast agent concentration, injection rate, heart rate and so on. The ultimate goal of all treatments for malignant tumors is to reduce the tumor load and inhibit malignant tumor progression, there are many indexes in serum that can reflect the tumor malignancy and evaluate the clinical efficacy, and they are known collectively as tumor markers. CA125, CA153, CEA and CYFRA21-1 are the broad-spectrum tumor markers that are the most commonly used and referred to in various studies, their contents may rise to different extent in a variety of malignant tumor diseases, but they are not organ-specific, the sensitivity and specificity of single index detection are not high, but combined detection of a variety of indicators has high clinical significance [11-13]. In this study, the differences in serum contents of above non-organ-specific tumor markers were compared between the two groups of patients before and after treatment, and it was found that compared with those before treatment, serum CA125, CA153, CEA and CYFRA21-1 contents of both groups decreased after treatment, which shows that both treatments can reduce the tumor malignancy to different levels; further compared with those of control group, serum CA125, CA153, CEA and CYFRA21-1 contents of observation group were lower after treatment, it confirms that intravenous chemotherapy combined with radiofrequency ablation can more effectively reduce the tumor load and inhibit tumor malignancy, this is mainly because that radiofrequency ablation directly induces tumor cell death with high temperature, and it confirms the efficiency of radiofrequency ablation from the serology level. Further Pearson test showed that CT dynamic enhanced scanning parameters PH and perfusion value levels in patients with non-small cell lung cancer were positively correlated with serum CA125, CA153, CEA and CYFRA21-1 contents, which shows that dynamic enhanced CT scanning parameter values can objectively reflect the malignant degree of tumor.
Tumor angiogenesis is the material basis for the tumor cells to obtain oxygen and nutrients, and also the important reason to realize tumor proliferation, invasion and other malignant biological behaviors, and the angiogenesis extent within tumor is directly related to its malignant degree, and can also predict the prognosis of tumor treatment. VEGF is the most powerful factor known to promote angiogenesis, it can regulate the expression of many downstream genes and influence multiple signal pathways, and highly expressed VEGF is a sign of high malignancy of tumors [14]. The pro-angiogenesis effect of Ang-2 is closely related to VEGF. When VEGF exists, the main manifestations of Ang-2 are promoting angiogenesis, accelerating vascular hyperplasia and increasing vascular wall permeability [15]. HIF-1α could mediate the adaptive changes of tumor cells under hypoxic conditions, directly regulate cell transcription level, promote VEGF expression and induce the increase of tumor angiogenesis [16]. MMP-9 belongs to the matrix metalloproteinase family, its main role is to decompose the extracellular matrix and increase cell mobility, and it also promotes angiogenesis [17]. In this study, the serum contents of above vascular tumor markers were compared between the two groups before and after treatment, and it was found that compared with those before treatment, serum VEGF, Ang-2, HIF-1α and MMP-9 contents of both groups were lower after treatment, which represents that both treatments can inhibit tumor angiogenesis; further compared with those of control group, serum VEGF, Ang-2, HIF-1α and MMP-9 contents of observation group were lower after treatment, it confirms that adding radiofrequency ablation can further inhibit tumor angiogenesis, and this is directly related to its roles in killing tumor cells directly and causing the lesions to form fibrosis tissue. Further Pearson test showed that CT dynamic enhanced scanning parameters PH and perfusion value levels in patients with non-small cell lung cancer were positively correlated with serum VEGF, Ang-2, HIF-1α and MMP-9 contents, and it confirms that the dynamic enhanced CT scanning parameter values can objectively reflect the degree of tumor angiogenesis.
To sum up, systemic intravenous chemotherapy combined with radiofrequency ablation can effectively kill the tumor cells and inhibit the local angiogenesis in patients with advanced non-small cell lung cancer, and dynamic enhanced CT scanning parameter value levels have a good correlation with tumor malignancy, and can be used as the effective means to reflect the tumor malignancy and evaluate the clinical therapeutic effect.
杂志排行
Journal of Hainan Medical College的其它文章
- Mechanism of therapeutic effects of Huangbo on ureteral stones based on network pharmacology
- Molecular mechanism of Turmeric in the treatment of liver cancer based on network pharmacology
- Meta-analysis of randomized controlled trials of traditional Chinese medicine in the treatment of obstructive sleep apnea syndrome
- Therapeutic efficacy of traditional Chinese medicine compound in the treatment of membranous nephropathy: A systematic review and metaanalysis
- Effects of fumigation and washing with Shujin Huoluo decoction combined with Duhuo Parasitic decoction on TIMP-1 and PON1 levels in KOA patients
- The effect of Xuebijing on burn patients and its effect on pain and wound healing