Hydatidosis and the duodenum: A systematic review of the literature
2020-12-16ctordelaFuenteAguilarPatriciaBeneitezMascaraqueSergioBerguaArroyoMarFernndezRiesgoIreneCamGarcIrisCruzaAguileraKenniaUgarteezJosRamia
Víctor de la Fuente-Aguilar, Patricia Beneitez-Mascaraque, Sergio Bergua-Arroyo, María Fernández-Riesgo, Irene Camón-García, Iris Cruza-Aguilera, Kennia Ugarte-Yáñez, José M Ramia
Víctor de la Fuente-Aguilar, Patricia Beneitez-Mascaraque, Sergio Bergua-Arroyo, María Fernández-Riesgo, Irene Camón-García, Iris Cruza-Aguilera, Kennia Ugarte-Yáñez, José M Ramia, Faculty of Medicine, Universidad of Alcalá, Alcalá de Henares 28801, Spain
José M Ramia, Servicio de Cirugía General y del Aparato Digestivo, Hospital General Universitario de Alicante and Institute for Health and Biomedical Research (ISABIAL) Alicante 03010, Spain
Abstract
Key words: Echinococcosis; Hydatidosis; Duodenum; Surgery; Review
INTRODUCTION
Hydatidosis is a zoonosis caused by the larval form of the genusEquinococcusspp, andEquinococcus granulosus(E.granulosus) causes the formation of hydatid cysts (HC).The life cycle ofE.granulosusincludes different herbivores (lambs, cows, pigs, deer) and carnivores (dogs, foxes, wolves); the dog is the most frequent definitive host[1].The distribution ofE.granulosusis associated with livestock exploitation and temperate climate zones such as southern Europe, Latin America, Australia and New Zealand, Africa, and the Middle East.A prevalence of HC of 2%-6% is estimated in the population in endemic areas[2].
The human being is an intermediate host, as it is infected orally with food contaminated by eggs from the feces of the definitive host.The eggs hatch in the intestine, releasing oncospheres that penetrate the intestinal wall and invade different sitesviathe bloodstream, the most frequent being the liver (50%-70%) and the lungs (20%-30%).The oncospheres evolve into HC, which may remain asymptomatic until their growth causes complications derived from the mass effect, depending on their location.Rupture of the HC can spread its contents throughout the body and trigger anaphylactic shock[3].
The duodenum is an organ that is very rarely affected by HC, either primarily or secondarily.Possible forms of secondary duodenal involvement are compression, or, more frequently, fistulization from HC located in neighboring organs[4].The HC that most often fistulize the duodenum are those located in the liver (0.15% of instances), with cases also described from the pancreas and kidney.Its low prevalence and the few existing records mean that the choice of the best therapeutic management is a challenge[4].
Here we present a systematic literature review of cases of hydatidosis with duodenal involvement published in the scientific literature.
MATERIALS AND METHODS
Literature search
Following the guidelines of the PRISMA methodology for systematic reviews, a search was performed in the PubMed, SCielo and EMBASE databases[5], unlimited by language or time.The terms used for the search were: (duodenum) AND [(echinococcosis, hepatic) OR (echinococcosis) OR (echinococcosis, hepatic) OR (hepatic echinococcosis) OR (hepatic echinococcosis) OR (echinococcosis, hepatic alveolar) hepa (alveolar) hepato) OR (alveolar echinococcosis, hepatic) OR (echinococcosis, hepatic alveolar) OR (hepatic alveolar echinococcosis) OR (hepatic alveolar echinococcosis) OR (hydatidosis, hepatic) OR (hepatic hydatidosis) OR (hepatic hydatidosis) OR (hepatic hydatidosis) hepa (alveolar echinococcus, hepatic) OR (echinococcus, hepatic alveolar) OR (hepatic alveolarechinococcus) OR (hydatid cyst, hepatic) OR (cyst, hepatic hydatid) OR (cysts, hepatic hydatid) OR (hepatic hydatid cyst) OR (hepatic hydatid cyst) OR (hepatic hydatid ) OR (hydatid cysts, hepatic) OR (echinococcosis) OR (echinococcus infection) OR (echinococcus infections) OR (infection, echinococcus) OR (cystic echinococcosis) OR (cysticechinococcosis) OR (echinococcosis, cystic) OR (echinoco cystic) OR (hydatidosis) OR (hydatidosis) OR (cysts, hydatid) OR (cyst, hydatid) OR (hydatid cysts) OR (hydatid cyst) OR (hydatid disease) OR (hydatid diseases) OR (echinococcus granulosus infection) OR (echinococcus granulosus infections) OR (granulosus infection, echinococcus) OR (granulosus infections, echinococcus) OR (infection, echinococcusgranulosus) OR (infections, echinococcus granulosus)].
A case was defined as any patient diagnosed with primary duodenal hydatidosis or hydatidosis in any location with secondary duodenal involvement.
A total of 83 articles were obtained with the search strategy described, and all articles that included patients with the characteristics mentioned were selected.Case reports were not excluded.Fourteen articles were chosen, but only 12 could eventually be studied; the other two could not be accessed even though the corresponding publishers were contacted.
The available data on the patients were extracted and included in Tables 1 to 3, for later discussion.They were classified into three groups: Clinical data, including age, sex, main symptoms and signs and personal history; analytical and radiological data, including laboratory data and the main findings reported in the imaging and endoscopic tests performed; and intra and postoperative findings that include the surgeries performed and the complications detected in the postoperative course and follow-up.
RESULTS
The twelve articles selected were all case reports, describing 14 cases.The countries where the 14 patients were treated were: Spain (6), Tunisia (4), India (2), France (1), and Turkey (1)[4,6-16].
Clinical data
Seven patients were men and seven women, with a mean age of 53.14 ± 17.65 years (range: 28-78) (Table 1).Nine of the patients (64%) had abdominal pain (3/9 located in the right hypochondrium, 2/9 in the epigastrium and in the remaining 4/9 not specified).As for the rest of the clinical data, nine patients (64%) presented nausea and vomiting, two of them with hematemesis and one with hydatidemesis.Six patients (42%) had fever > 38ºC, three did not, and in five this information was not specified.Abdominal palpation was painful in ten cases (71%), and in seven patients masses were noted.Other symptoms and signs described included jaundice, melena, hydatidenteria, anorexia and weight loss.Three patients had previously undergone surgery for liver HC.
本周的市场表现来看,整体呈现出来的是筑底折腾的过程。在12月20日的专栏文章《市场短期反弹后继续下探》中,笔者曾经描述过,市场将会在本周先反抽再震荡回落。文章中如此描述:
二是特殊时期航标巡检的安全管理。在组织相关巡检人员进行特殊时期的航标巡检工作时,相关安全管理人员要结合重点值守、夜巡航标、巡检值班等航标巡检的应急工作安排,针对性的进行巡检工作的安全管理。特别是在特殊天气条件的航标巡检工作中,相关安全管理人员要组织巡检人员利用遥测遥控系统对航标的不良情况进行深入的分析,完成器材的准备。同时,也要加强对海域气候、涌浪等情况的掌握,通过使用定位及通讯设备,加强航标巡检的安全性。
Analytical, radiological and endoscopic studies
Analytical values were only available in nine patients (Table 2).In six of these (66%) leukocytosis was observed, in three neutrophilia, and in one eosinophilia.Blood analysis was only reported in five patients: In one it was found to be normal, and the remaining four presented low levels of hemoglobin and hematocrit.Serological results of hydatidosis (Casoni test or others) were provided in only six cases (42%: Four positive and two negative); in the other eight, no serological studies were mentioned.
As for radiological studies, only abdominal X-ray was reported in six patients (42%) and thorax in three (21%); in one case both tests were discussed.No simple radiology information was available in six cases (the last six published).Abdominal radiography found masses in four patients, two of which presented calcification.The chest radiograph revealed an over-elevation of the right hemidiaphragm in one patient, the presence of intralesional gas in two, calcification of the wall in one.Abdominal ultrasound was reported in only four patients (28%), three of whom presented cystic lesions.
Computed tomography (CT) was performed in ten patients (71%) (in two of them using contrast).In all of them cystic lesions were discovered (two with calcification) a
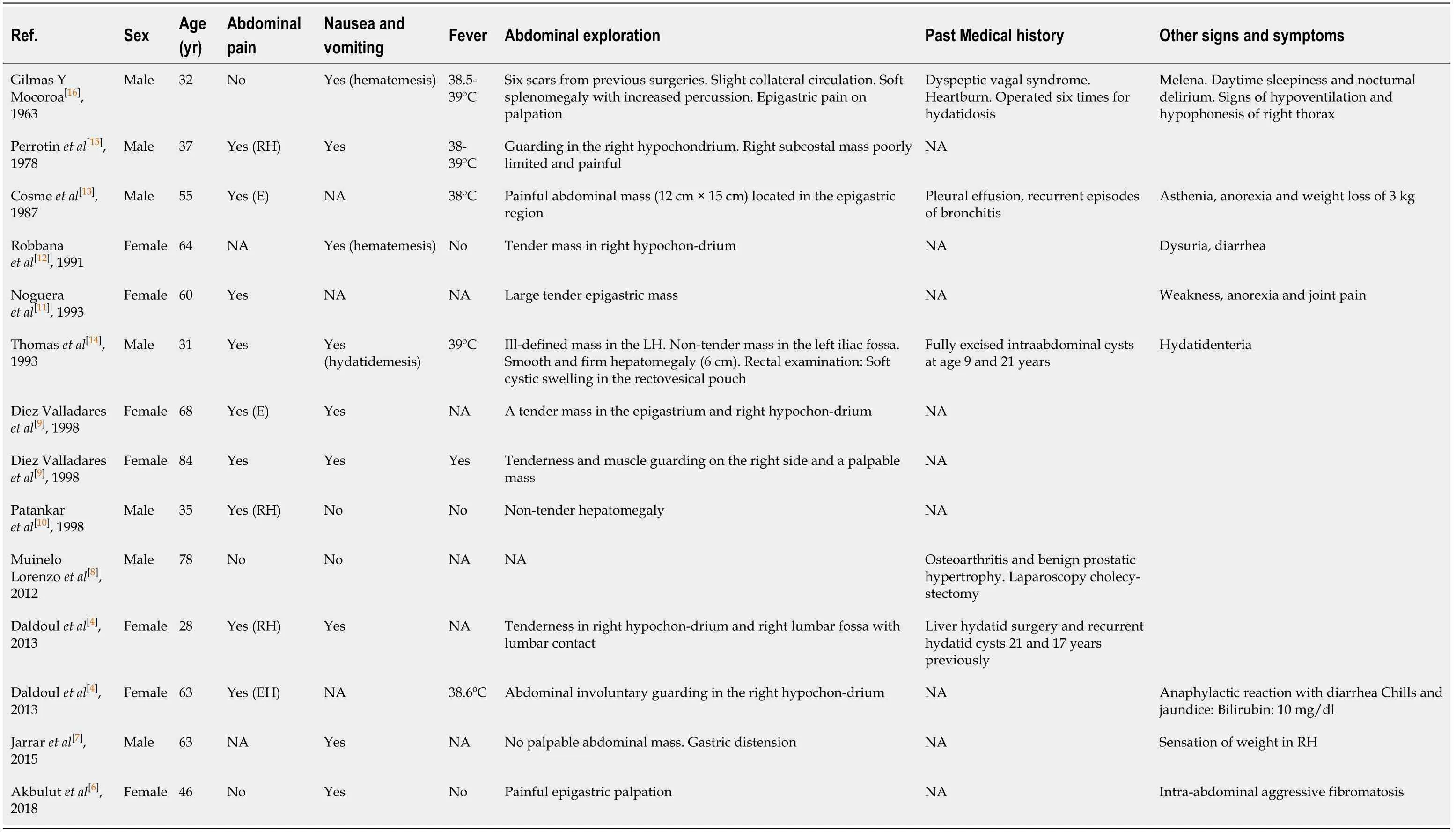
Table 1 Clinical data
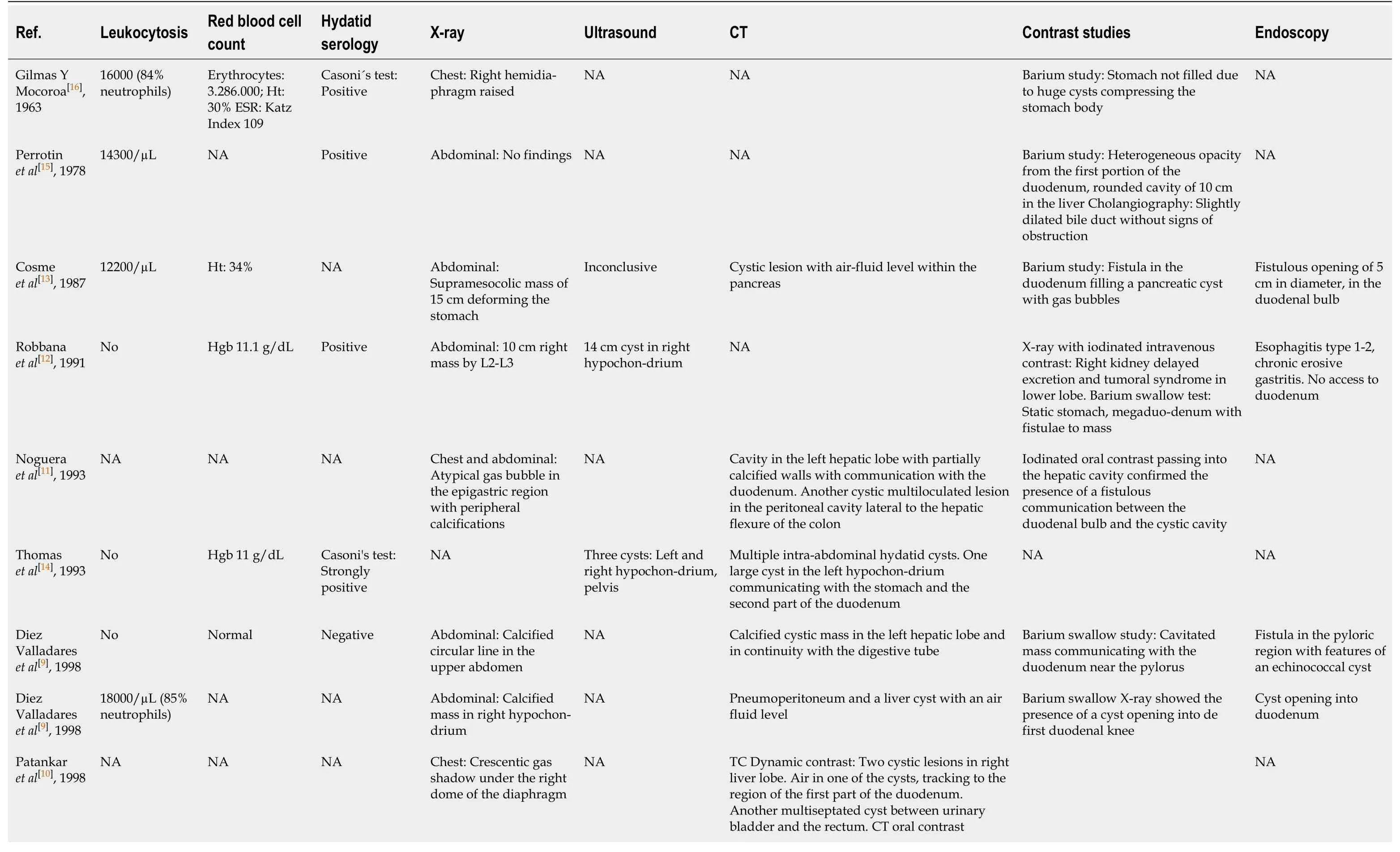
Table 2 Analitical, radiological and endoscopic studies
CT: Computed tomography; NA: Not available; HT: Hematocryte; HGB: Hemoglobin
The location of the HC causing the duodenal fistula, confirmed by imaging techniques, was the liver in 11 cases (78%), and kidney, pancreas and paraduodenal area in one case each.
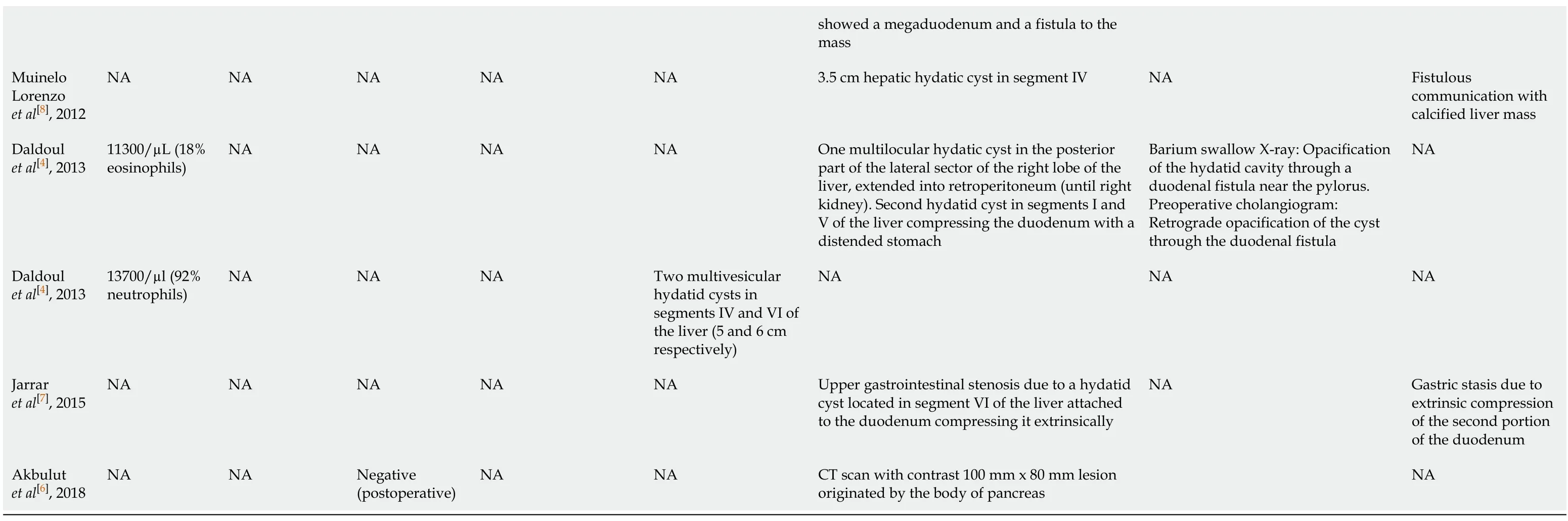
Intraoperative findings, postoperative period and follow-up
Twelve patients presented fistula between the HC and the duodenum (Table 3).One patient presented a paraduodenal HC diagnosed incidentally during surgery for abdominal fibromatosis and another had large-scale duodenal compression due to a liver HC, without a true fistula.
Twelve patients (85%) received surgical treatment.Of the other two, one received only pharmacological medical treatment with antiparasitic drugs and in the other the treatment was not specified.The type of laparotomy was reported in seven patients: Three midline, two bilateral subcostal, and two right; in one, the type was not specified.
The techniques performed to treat HC in the twelve patients operated on were conservative in nine [partial cyst resection (3), enucleation (2), evacuation/drainage (2), Lagrot (1) and ablation (1)] and radical in three (all total cystectomies).The procedures performed on the duodenal fistula in the ten patients with this condition operated upon were: (1) Closure of the duodenal fistula in five patients, in one case associated with vagotomy, and in another with gastrostomy plus pylorotomy; (2) Partial duodenal resection plus pyloroplasty and bilateral truncated vagotomy (one patient); (3) Duodenostomy, gastrostomy and jejunostomy (one patient); (4) Duodenal diverticulization (one patient); (5) Not specified (one patient); and (6) Intracavitary drainage without action on the fistula (one patient).
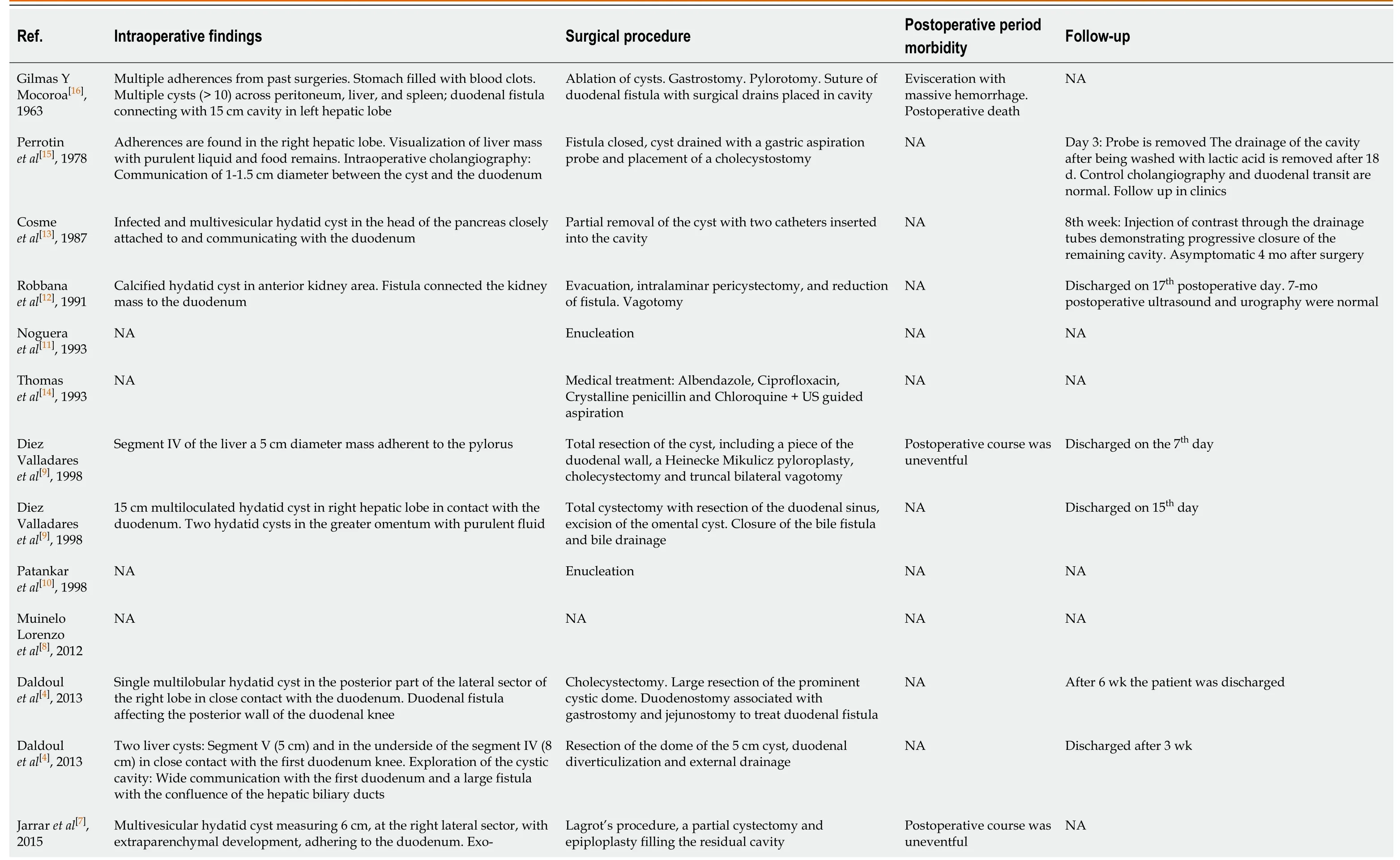
Table 3 Intraoperative findings, postoperative period and follow-up

NA: Not available; US: Ultrasound.
Postoperative morbidity and mortality was not described in detail in the articles consulted.In three patients the postoperative period was reported to be uncomplicated, and one patient (7%) died due to hemoperitoneum following massive hemorrhage.In the five cases in which mean hospital admission was mentioned, it was 20.4 ± 11.72 d (range: 7-42).The follow-up was not described in detail, though it was usually very short.
DISCUSSION
Hydatidosis is a zoonosis caused by Echinococcus spp associated with livestock activity, predominantly in geographical areas with temperate climates such as Southern Europe, Latin America, Australia, New Zealand, Africa and the Middle East[2].Primary or secondary duodenal involvement due to HC via fistulization or compression from other locations is extremely rare and the number of reported cases is very low[4,6-16].The main objective of our study was to evaluate the clinical, diagnostic and therapeutic data of duodenal involvement recorded in the literature and to assess whether a diagnostic and therapeutic algorithm could be obtained.
The articles included do not describe any etiological factors or pathogenesis related to duodenal injury caused by HC.HC located in segments IVB, V and VI, and those located in the kidney or pancreas may affect the duodenum, but this is exceptional.Our (unprovable) opinion regarding this low frequency is that a series of conditions must exist for a fistula to appear: The cyst must be large, complicated, and longstanding, since the duodenal wall is sufficiently thick to allow compression without fistulization.If these conditions are met, after very prolonged inflammatory processes the fistula eventually forms.
The epidemiological data of the 14 patients studied do not indicate any differentiation according to sex (the ratio was 1:1) or age (the range was large).Duodenal injury caused by HC is mostly secondary.There was only one case of a paraduodenal cyst; in the cases reported the duodenum was secondarily affected by hepatic (11/13: 85%), renal (1/13) and pancreatic (1/13) HC[4,6-16].In 90% of patients the injury is in the form of a fistula between the HC and the duodenum.The descriptions in the articles do not indicate which duodenal segment is the most affected.Three patients had previously undergone liver hydatidosis.
The most frequent clinical manifestations in the patients studied were abdominal pain, nausea and vomiting.The rest of the clinical data were very heterogeneous.Two cases presented hydatidemesis and/or hydatidenteria[14], but the condition may also be asymptomatic.Therefore, there is no typical clinical picture of HC affecting the duodenum.
The diagnosis of duodenal fistula due to HC is not always easy.Computed tomography was the most used diagnostic tool in the patients reviewed; it allows accurate location of the HC and its relationship with the digestive tract, but in our study only achieved preoperative diagnosis of fistula in four patients (40%).It should be noted that some reports do not specify whether oral contrast was used in the CT, and some of the older cases the CT techniques used are not comparable to the ones used today[4,6-16].The use of various radiological tests with contrast, especially in the first cases, allowed the diagnosis of fistula, although barium contrast studies are not currently used.Upper gastrointestinal endoscopy was used in six patients with a diagnostic capacity of 66% (4/6)[4,6-16].Therefore, we are unable to propose a definitive diagnostic algorithm, but the combination of CT with contrast and upper gastrointestinal endoscopy seems to be the most effective.
In the literature, there is no consensus on which treatment that should be applied.Surgery was performed in practically all patients (12/13), using a wide variety of procedures to treat both HC and duodenal fistula, adapting to intraoperative findings.Conservative techniques were used in 75% of HC, while in the duodenum the most frequent technique (50%) was the closure of the fistula associated with various types of intestinal bypass; partial duodenal resection was performed in only one case.The operative morbidity rate was 7% (1/14), and postoperative mortality 7% (1/14).We believe that the estimation of morbidity is excessively low, because in many articles it is not reported or it is simply stated that the postoperative period was uneventful; in addition, duodenal surgery usually presents a much higher complication rate than that reported in these patients.Furthermore, in the cases in which data on postoperative stays are given, these stays are much longer than one would expect in uncomplicated patients.The follow-up carried out in patients is not usually specified, so we cannot draw any conclusions about disease recurrence or long-term evolution.
Our intention in carrying out this systematic review was to provide a therapeutic algorithm for hydatidosis that affects the duodenum, but especially the surgical strategy to be performed.As we have summarized, no conclusion can be drawn from the literature.Our group thinks that radical surgery is the best approach in hydatidosis, but we also believe that surgical procdures should be tailored to every patient.Our non Evidence Based Medicine supported recommendation is: If the surgeon thinks that radical surgery is technically feasible, should be performed in the liver and duodenum.But if an unacceptable risk is to be assumed to carry it out, conservative procedures can be useful in the most bizarre cases.Duodenal surgery is not simple, nor is it free of complications, and techniques can range from a simple closure, duodenal exclusion to duodenectomies.The decision of which technique to perform in the duodenum will depend on the amount of circumference affected, the duodenal segment to be treated, and anatomical relationship with the Vater´s ampulla.
The following conclusions can be drawn from this systematic review.The reports of duodenal damage by HC are based on isolated clinical cases with very low scientific evidence; the most common clinical findings are abdominal pain, nausea and vomiting; the combination of computed tomography plus endoscopy seems to be the best diagnostic option; finally, the most frequently recommended treatment is surgery to treat the HC and to close the fistula.
ARTICLE HIGHLIGHTS
Research background
The duodenum is an organ that is very rarely affected by hydatid cysts, either primarily or secondarily.
Research motivation
Duodenal involvement by hydatidosis is an exceptional finding and this study aimed to characterize epidemiological, clinical and diagnostic features and options of treatments.
Research objectives
Our aim is to characterize epidemiological, clinical and pathological features and options of treatment in hydatidosis with duodenal involvement.
Research methods
We perform a system review including all patients with hydatidosis and duodenal involvement following PRISMA guidelines.
Research results
This review shows that the most frequent symptoms were abdominal pain, nausea and vomiting.Computed tomography was the most used diagnostic imaging technique, and hydatid cyst drainage and fistula closurevialaparotomy was the most frequent treatment.
Research conclusions
Literature on hydatidosis with duodenal involvement is scarce, only case reports, so the evidence is low.
猜你喜欢
杂志排行
World Journal of Meta-Analysis的其它文章
- COVID-19: Off-label therapies based on mechanism of action while waiting for evidence-based medicine recommendations
- Learning and competence development via clinical cases – what elements should be investigated to best train good medical doctors?
- Immunotherapy in hepatocellular carcinoma: Combination strategies
- Combined endoscopy/laparoscopy/percutaneous transhepatic biliary drainage, hybrid techniques in gastrointestinal and biliary diseases
- Thrombopoietin-receptor agonists in perioperative treatment of patients with chronic liver disease
- Role of non-coding RNAs in pathogenesis of gastrointestinal stromal tumors
