低频电刺激联合膀胱功能训练治疗脊髓损伤诱发的神经源性膀胱的效果评价
2020-11-16娄菊红程凤敏吴秀玲郑彬彬
娄菊红 程凤敏 吴秀玲 郑彬彬


[摘要] 目的 評价低频电刺激联合膀胱功能训练治疗脊髓损伤(SCI)诱发的神经源性膀胱(NB)的效果。 方法 选取2017年5月~2019年2月我院骨科门诊就诊的SCI诱发NB患者90例,随机分为观察组与单纯组,每组各45例。观察组予以低频电刺激联合膀胱功能训练治疗,单纯组予以单纯的膀胱功能训练,两组均治疗6周。评估两组治疗前后排尿情况及尿动力学指标的变化,并比较其临床疗效。 结果 治疗6周后,两组日均单次排尿量和日单次最大排尿量较治疗前明显增加,日均排尿次数较治疗前明显下降(P<0.05或P<0.01),且观察组变化幅度较单纯组更显著(P<0.05);两组膀胱内压力和Qmax较治疗前明显上升,RU较治疗前明显下降(P<0.05或P<0.01),且观察组变化幅度较单纯组更显著(P<0.05);同时观察组临床总有效率(95.56%)明显高于单纯组(82.22%)(χ2=4.053,P<0.05)。 结论 低频电刺激联合膀胱功能训练用于治疗SCI诱发NB患者的效果确切,能更明显改善患者的排尿情况及尿动力学状态。
[关键词] 脊髓损伤;神经源性膀胱;低频电刺激;膀胱功能训练;排尿情况;尿动力学
[中图分类号] R651.2;R694.5 [文献标识码] A [文章编号] 1673-9701(2020)25-0011-04
Evaluation on the effects of low-frequency electrical stimulation combined with bladder function training in the treatment of neurogenic bladder induced by spinal cord injury
LOU Juhong CHENG Fengmin WU Xiuling ZHENG Binbin
Department of Orthopedics, Zhejiang Taizhou Hospital, Taizhou 317000, China
[Abstract] Objective To evaluate the effect of low-frequency electrical stimulation combined with bladder function training in the treatment of neurogenic bladder (NB) induced by spinal cord injury (SCI). Methods A total of 90 patients with SCI-induced NB who visited the outpatient clinic of orthopaedics in our hospital from May 2017 to February 2019 were selected and randomly divided into observation group and simple group, with 45 cases in each group. The observation group was given low frequency electrical stimulation combined with bladder function training. The simple group was given bladder function training alone. Both groups were treated for 6 weeks. The changes in urination and urodynamic parameters before and after treatment were evaluated in both groups, and their clinical effects were compared. Results After 6 weeks of treatment, the average daily single urination volume and maximum single urination volume in both groups were increased significantly compared with those before treatment. The average daily urination frequency was significantly lower than that before treatment(P<0.05 or P<0.01), and the change in the observation group was more significant than that in the simple group(P<0.05); the intra-bladder pressure and Qmax in both groups were increased significantly compared with those before treatment, and the RU was decreased significantly(P<0.05 or P<0.01). The change in the observation group was more significant than that in the simple group(P<0.05); at the same time, the total clinical effective rate in the observation group(95.56%) was significantly higher than that in the simple group(82.22%)(χ2=4.053, P<0.05). Conclusion Low-frequency electrical stimulation combined with bladder function training is effective in the treatment of patients with SCI-induced NB, which can significantly improve patients' urination and urodynamic conditions.
[Key words] Spinal cord injury(SCI); Neurogenic bladder(NB); Low frequency electrical stimulation; Bladder function training; Urination; Urodynamics
神经源性膀胱(Neurogenic bladder,NB)是由于中枢或周围神经受损引起膀胱尿道功能障碍性疾病,是脊髓损伤(Spinal cord injury,SCI)诱发的常见并发症之一,主要表现有尿潴留、尿失禁及膀胱刺激症等,易诱发尿道感染及肾功能异常等并发症,严重时可发生肾衰竭,危及患者生命[1-2]。膀胱功能训练是目前公认的治疗SCI诱发NB的最有效手段,主要通过建立反射性膀胱,使得膀胱逼尿肌发生收缩引起排尿功能的恢复[3-4]。低频电刺激疗法是近年来兴起的用于治疗SCI诱发NB患者的治疗措施,但其联合膀胱功能训练用于SCI诱发NB患者国内报道较少[5-6]。近年来我院采用低频电刺激联合膀胱功能训练用于治疗SCI诱发NB患者,疗效较满意,现报道如下。
1 资料与方法
1.1 一般资料
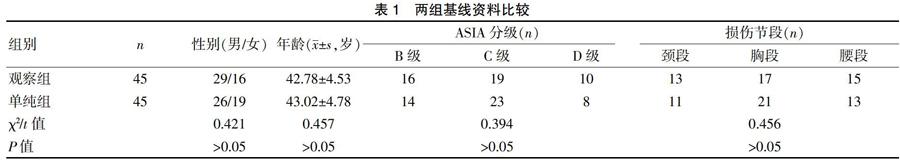
选取2017年5月~2019年2月我院骨科门诊就诊的SCI诱发NB患者90例。纳入标准[7]:①符合美国脊柱损伤学会2010年制定的SCI相关标准[8],且经临床证实为NB患者;②患者病情稳定且留置尿管已拔除;③年龄18~70岁,美国脊柱损伤委员会脊髓损伤神经学分类标准(American Spinal Injury Association impairment scale,ASIA)分级为B~D级。排除标准[9]:①以往存在尿道或膀胱损伤、狭窄或畸形者;②SCI急性期;③意识不清或生命体征不稳定,或有神经精神系统疾病及不配合治疗者。采用随机数字表法分为观察组与单纯组,每组各45例。两组患者的性别、年龄、ASIA分级及损伤节段等基线资料比较,差异无统计学意义(P>0.05),具有可比性。见表1。
1.2 方法
观察组予以低频电刺激联合膀胱功能训练治疗,其中膀胱功能训练采用耻骨上区轻叩法,用指尖轻叩患者下腹部膀胱区10~20次,后练习屏气,指导患者身体前倾,快速呼吸3~4次,延长屏气增加腹压时间,进行1次深呼吸,后屏住呼吸,并向下用力做排尿动作,重复3~5次,至无尿液排出;其中低频电刺激方法,选取爱生NMT-9系列神经肌肉治疗仪进行低频电刺激治疗,将两个电极片贴在膀胱近顶部两侧壁,另两个贴在耻骨和肚脐连线的膀胱顶端下缘部与骶尾关节上2~3 cm处。电流强度以能适应并能观测到适量的肌肉收缩为最佳,且不超过50 mA,频率为1次/d,20 min/次,5 d/周。单纯组予以单纯的膀胱功能训练,具体方法同观察组。两组均治疗6周。
1.3 观察指标
评估两组治疗前后排尿情况及尿动力学指标的变化,并比较其临床疗效。
1.3.1 排尿情况及尿动力学指标 排尿情况包括日均单次排尿量、日单次最大排尿量和日均排尿次数。尿动力学指标包括膀胱内压力、最大尿流率(Qmax)和残余尿量(Residual urine,RU),采用尿流动力学检查测定。
1.3.2 临床疗效评估标准[10] 显效:治疗后患者有尿意时可自控≥2 min,无遗尿或滴尿现象,平均排尿间隔≥2 h;有效:治疗后患者有尿意时可自控1~2 min,偶有遗尿及滴尿现象,平均排尿时间间隔1~2 h;无效:未达上述标准。除无效均为总有效。
1.4 统计学处理
应用SPSS18.0统计学软件进行数据分析。计量资料以均数±标准差(x±s)表示,采用t检验;计数资料以[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组治疗前后排尿情况指标比较
治疗前两组日均单次排尿量、日单次最大排尿量和日均排尿次数比较相接近(P>0.05);治疗6周后,两组日均单次排尿量和日单次最大排尿量较治疗前明显增加,日均排尿次數较治疗前明显下降(P<0.05或P<0.01),且观察组变化幅度较单纯组更显著(P<0.05)。见表2。
2.2 两组治疗前后膀胱内压力、Qmax和RU的比较
治疗前两组膀胱内压力、Qmax和RU比较相接近(P>0.05);治疗6周后,两组膀胱内压力和Qmax较治疗前明显上升,RU较治疗前明显下降(P<0.05或P<0.01),且观察组变化幅度较单纯组更显著(P<0.05)。见表3。
2.3 两组临床疗效比较
治疗6周后,观察组临床总有效率(95.56%)明显高于单纯组(82.22%),差异有统计学意义(χ2=4.053,P<0.05)。见表4。
3 讨论
SCI是一种临床较常见的外伤性中枢神经损伤,除可引起四肢瘫痪或截瘫外,还常影响患者膀胱的神经支配,诱发NB[11-12]。NB可因慢性尿液潴留导致膀胱过度充盈,使得膀胱黏膜慢性充血和水肿,引起膀胱黏膜的防御力下降,加之尿液长时间在膀胱内潴留易继发尿路感染,常导致患者发生脓毒血症、肾积水及肾功能不全等严重并发症,是引起SCI患者病情恶化或死亡的主要原因[13-14]。膀胱功能训练是根据学习理论和条件反射原理,通过患者主观意识活动及功能锻炼以改善膀胱的储尿排尿功能,可以改善膀胱排尿功能的一种锻炼方法。膀胱功能训练可通过使膀胱及尿道括约肌处于周期性扩张和收缩状态,使患者膀胱内的尿液得以排空,使膀胱能维持近似正常的生理状态,有利于膀胱功能和尿道括约肌的残存功能逐渐得到恢复,有助于维护膀胱顺应性,减轻肾功能受损,而且可反射性调节大脑和脊髓神经系统相应神经细胞的功能,有利于建立正常的膀胱自主排尿功能[15-16]。
低频电刺激在SCI诱发NB患者中的应用价值在近年来逐渐得到临床重视。低频电刺激可刺激患者骶神经根内支配膀胱逼尿肌的副交感神经,激活兴奋性或一致性神经通路,从而调节逼尿肌、括约肌及盆底肌的运动功能,进而建立起膀胱反射功能促进排尿的作用,改善膀胱的储尿和排尿功能,缓解患者的下尿路症状[17-18];同時在排尿期予以电刺激冲动可激活膀胱正常的感觉功能,使感觉障碍患者重新获取感知膀胱容量能力,并将信息向高级神经中枢传递,指导患者于膀胱安全容量期及时排空膀胱,减少尿液反流,有利于保护患者的上尿路功能;在储尿期还可抑制膀胱逼尿肌的异常反射,使得尿道括约肌发生闭合,减少尿液外溢,提高控尿功能[19-20];并能改善膀胱壁的局部血液循环,减少局部炎症物质的渗出,促进膀胱功能的恢复[21-22]。本研究结果发现,治疗6周后观察组患者日均单次排尿量、日单次最大排尿量增加幅度及日均排尿次数下降幅度与单纯组治疗后比较更显著,且观察组患者治疗后膀胱内压力和Qmax上升幅度及RU下降幅度亦与单纯组治疗后比较更显著,其临床总有效率亦明显高于单纯组,表明低频电刺激联合膀胱功能训练用于治疗SCI诱发NB患者的效果明显优于单纯膀胱功能训练治疗,能更明显改善排尿情况及尿动力学状态。推测认为低频电刺激和膀胱功能训练用于SCI诱发NB患者具有良好协同增效作用,能刺激膀胱逼尿肌的收缩,增加膀胱内压力,促进膀胱功能的恢复,促进尿液排出,减少残余尿量。
总之,低频电刺激联合膀胱功能训练用于治疗SCI诱发NB患者的效果确切,能更明显改善排尿情况及尿动力学状态。但本研究纳入的病例数偏少及观察时间偏短,其实验结果有待大样本及长时间研究进一步分析探讨。
[参考文献]
[1] Ginsberg D. Optimizing therapy and management of neurogenic bladder[J]. Am J Manag Care,2013,19(Suppl 10):197-204.
[2] Nevedal A,Kratz AL,Tate DG. Women's experiences of living with neurogenic bladder and bowel after spinal cord injury:Life controlled by bladder and bowel[J]. Disabil Rehabil,2016,38(6):573-581.
[3] 邢晓红,杜莹,常淑娟,等. 膀胱功能训练治疗脊髓损伤患者神经源性膀胧的疗效观察[J]. 中华物理医学与康复杂志,2014,28(11):773-775.
[4] 王晶,焦永波,刘春茹,等. 电针结合膀胱功能训练治疗脊髓损伤后神经源性膀胱的效果[J]. 中国医药导报,2016,13(7):87-89.
[5] 郝丽霞,张琰,刘帅,等. 低频电刺激结合康复训练治疗脊髓损伤神经源性膀胱患者疗效观察[J]. 中国临床研究,2017,30(1):116-119.
[6] Wang Z,Liao LM,Deng H,et al. The inhibitory effect of sacral dorsal root gangl ion st imulat ion on nocicept ive and nonnocicept ive bladder ref lexes in cats[J]. World J Urol,2018,36(5):829-836.
[7] Peyronnet B,Roumiguié M,Castel-Lacanal E,et al. Efficacy and safety of the first and repeated intradetrusor injections of abobotulinum toxin A 750 U for treating neurological detrusor overactivity[J]. World J Urol,2016,34(5):755-761.
[8] 李建军,周红俊,孙迎春. 脊髓损伤神经学分类国际标准(第6版,2006)[J]. 中国康复理论与实践,2007,10(1):25-26.
[9] 吴娟,廖利民,万里,等. 电刺激对治疗神经源性膀胱感觉障碍的疗效观察[J]. 中国脊椎脊髓杂志,2012,22(12):1059-1062.
[10] 周天健,李建军. 脊柱脊髓损伤现代康复与治疗[M]. 北京:人民卫生出版社,2006:880-881.
[11] Zeng FS,Zhang L,Cui BJ,et al. Expression of autophagy in different stages of neurogenic bladder after spinal cord injury in rats[J]. Spinal Cord,2017,55(9):834.
[12] Hamid R,Averbeck MA,Chiang H,et al. Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury[J]. World J Urol,2018,(6):1-11.
[13] Han JH,Kim SE,Ko IG,et al. Afferent pathway-mediated effect of α1 adrenergic antagonist,tamsulosin,on the neurogenic bladder after spinal cord injury[J]. Int Neurourol J,2017,21(3):178-188.
[14] Lavelle JP. Correlating spinal cord injur ies with neurogenic bladder pathophysiology[J]. BJU Int,2017,119(2):197-199.
[15] 康玉闻,金中华,沈楚龙,等. 电针疗法联合膀胱功能训练对脊髓损伤后神经源性膀胱尿动力学的影响[J]. 医学与哲学,2017,38(16):50-52.
[16] 沈雅萍,金剑,王爱娟,等. 个体化膀胱功能训练治疗脊髓损伤后神经源性膀胱患者的疗效观察[J]. 中华物理医学与康复杂志,2015,37(1):48-51.
[17] 刘奕,漆伟,徐贞杰,等. 间歇导尿联合神经电刺激治疗脊髓损伤后神经源性膀胱的疗效[J]. 国际泌尿系统杂志,2015,35(5):641-643.
[18] Holtermann A,Mork PJ,Andersen LL,et al. The use of EMG biofeedback for learning of selective activation of intra-muscular parts within the serratus anterior muscle:A novel approach for rehabilitation of scapular muscle imbalance[J]. J Electromyogr Kinesiol,2010,20(2):359- 365.
[19] 陳立霞,张杨,岳寿伟. 低频电刺激治疗脊髓损伤后神经源性膀胱尿潴留疗效观察[J]. 山东医药,2014,54(28):55-57.
[20] Chen G,Liao L,Wang Z,et al. Increasing bladder capacity by foot stimulation in rats with spinal cord injuries[J].BMC Urol,2017,17(1):85-87.
[21] Paradella AC,Musegante AF,Brites CR. Comparison of different ant ibiot ic protocols for asymptomatic bacteriuria in patients with neurogenic bladder treated with botul inum toxin A[J]. Braz J Infect Dis,2016,97(10):82-83.
[22] Mizoguchi S,Mori Kenichi,Wang Z,et al. Effects of estrogen receptor β stimulation in a rat model of non-bacterial prostatic inflammation[J]. Prostate,2017,77(7):803-811.
(收稿日期:2019-10-21)
