急性胃肠损伤分级联合多因素评估对危重患者死亡的预测价值
2020-11-06潘朝勇曾汇霞吴家圣廖梅嫣吴海宾钟友娣罗永杰
潘朝勇 曾汇霞 吴家圣 廖梅嫣 吴海宾 钟友娣 罗永杰

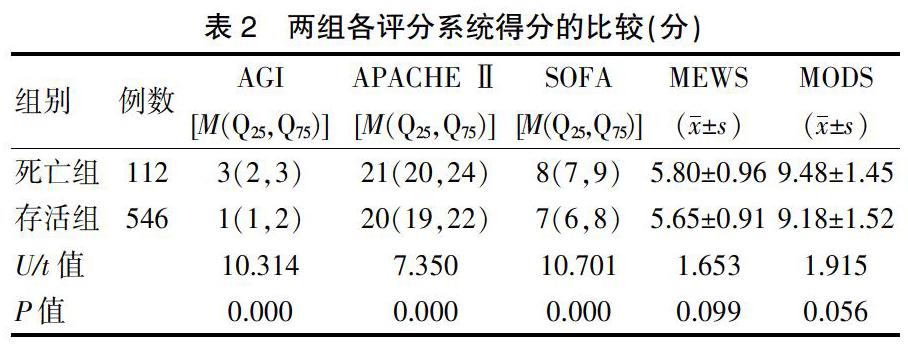
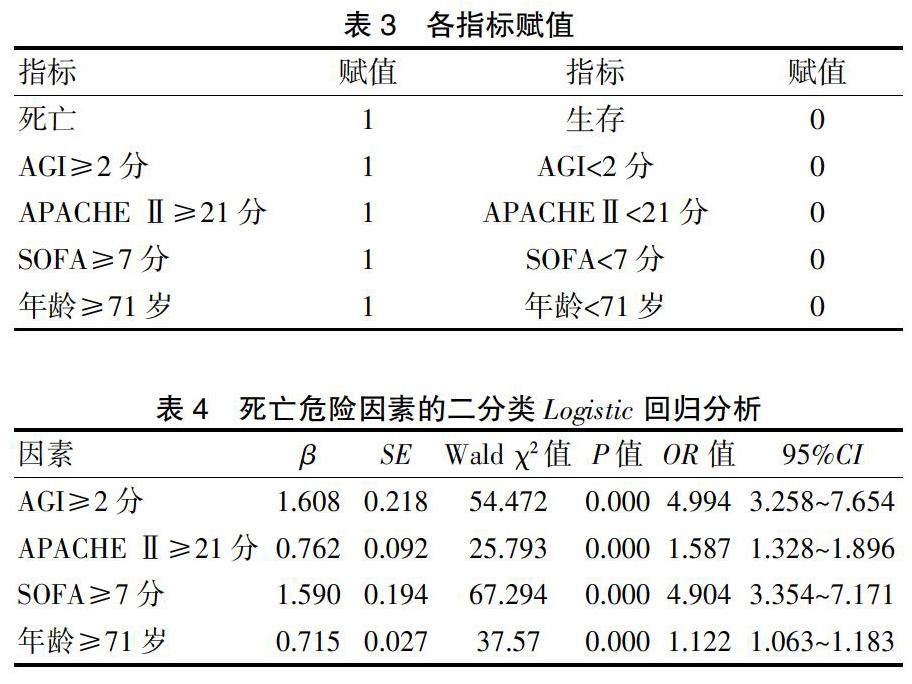
[摘要]目的 探讨急性胃肠损伤(AGI)分级联合多因素组成的新评分系统对危重症患者死亡的预测价值。方法 回顾性分析2016年1月~2020年3月肇庆市第二人民医院ICU收治的危重患者658例,根据28 d的存活情况分为死亡组(112例)和存活组(546例)。评估两组患者入院1周内AGI的最高分级,依据AGI最高分级,赋予相应分值(0~4分),得出AGI评分;记录患者入院24 h内急性生理慢性健康评分(APACHE Ⅱ)、序贯器官功能衰竭(SOFA)评分、多器官功能障碍综合征(MODS)评分、改良早期预警评分(MEWS)。两组资料进行单因素分析,对具有统计学意义的相关因素进一步行Logistic回归分析,筛选危重患者死亡的独立危险因素,绘制受试者工作特征(ROC)曲线,对比各评分的曲线下面积(AUC),评价AGI分级联合多因素评估组成的新评分系统对危重患者死亡的预测价值。结果 死亡组患者年龄、第1周内AGI得分、24 h内APACHE Ⅱ、SOFA评分高于存活组,差异有统计学意义(P<0.05);依据ROC曲线判别出AGI、APACHE Ⅱ、SOFA、AGE的最佳诊断临界值分别为AGI≥2分、APACHE Ⅱ≥21分、SOFA≥7分、年龄≥71岁。以患者生存状态为因变量,多因素分析结果显示:AGI≥2分(β=1.608,OR=4.994,95%CI=3.258~7.654)、APACHE Ⅱ≥21分(β=0.762,OR=1.587,95%CI=1.328~1.896)、SOFA≥7分(β=1.590,OR=4.904,95%CI=3.354~7.171)、年齡≥71岁(β=0.715,OR=1.122,95%CI=1.063~1.183)均是危重症患者不良预后的独立危险因素(P<0.05)。死亡预警评分、AGI、APACHE Ⅱ、SOFA评分再绘制ROC曲线,死亡预警评分AUC值为0.909,高于单用AGI评分、APACHEⅡ评分、SOFA评分的AUC值(0.796、0.715、0.805),差异有统计学意义(P<0.05)。结论 AGI分级评分联合多因素评估组成的新评分系统能够预警危重症患者的死亡风险,对危重患者死亡的预测价值优于单独使用任何一种评分。
[关键词]危重症;急性胃肠损伤;急性胃肠功能障碍;死亡预警评分;预测;预后
[中图分类号] R44 [文献标识码] A [文章编号] 1674-4721(2020)9(b)-0008-04
Prediction value of acute gastrointestinal injury grade combined with multifactorial evaluation on death in critical patients
PAN Chao-yong ZENG Hui-xia WU Jia-sheng LIAO Mei-yan WU Hai-bin ZHONG You-di LUO Yong-jie
Department of Critical Care Medicine, the Second People′s Hospital of Zhaoqing, Guangdong Province, Zhaoqing 526060, China
[Abstract] Objective To explore the value of a new rating system for acute gastrointestinal injury (AGI) grade combined with multiple factors to predict death in critically ill patients. Methods A single-center retrospective cohort study was used, 658 critically ill patients admitted to ICU at the Second People′s Hospital of Zhaoqing from January 2016 to March 2020 were enrolled. They were divided into death group (112 cases) and survival group (546 cases) according to 28 days survival. The highest grade of AGI within 1 week of admission was evaluated, according to the highest grade to give the score (0-4 points), as the AGI score. Physiological chronic health score (APACHE Ⅱ), sequential organ failure (SOFA) score, MODS score, and MEWS score which of within 24 h of admission in both groups were recorded. Data of two groups were analyzed by one-way analysis, and further Logistic regression analysis was performed factors, screening independent risk factors of death in critically ill patients, and drawing the receiver operating characteristic (ROC) curve of subjects to evaluate the predictive value of a new rating system for acute gastrointestinal injury grading combined with multifactorial critical patient death. Results The age, the AGI score in the first week, APACHE Ⅱ, SOFA score in the death group were higher than those in the survival group, and the differences were statistically significant (P<0.05). According to the ROC curve, the best diagnostic thresholds for AGI, APACHE Ⅱ, SOFA, and AGE were AGI ≥ 2 points, APACHE Ⅱ ≥ 21 points, SOFA ≥ 7 points, and age ≥ 71 years old. Results of multivariate analysis showed that AGI≥2 points (β=1.608, OR=4.994, 95%CI=3.258-7.654),APACHE Ⅱ≥21 points (β=0.762, OR=1.587, 95%CI=1.328-1.896), SOFA≥7 points (β=1.590, OR=4.904, 95%CI=3.354-7.171), age≥71 years (β=0.715, OR=1.122, 95%CI=1.063-1.183) were independent risk factors for poor prognosis in critically ill patients (P<0.05). The ROC curve was drawn for the death warning score, AGI, APACHE Ⅱ, and SOFA score, the death warning score AUC value was 0.909, which was higher than the AUC value of the AGI score, APACHE Ⅱscore and SOFA score alone (0.796, 0.715, 0.805), the differences were statistically significant (P<0.05). Conclusion The new scoring system of acute gastrointestinal injury rating combined with multi-factor evaluation can warn the death risk of critically ill patients, and the predictive value of critical patients′ death is better than that of any single score.
2.4死亡预警评分、AGI评分、APACHEⅡ评分、SOFA评分对危重患者的死亡预测价值的效能评估的比较
在Logistic回归方程中求得AGI≥2分、APACHE Ⅱ≥21分、SOFA≥7分、年龄≥71岁的β值分别为1.608,0.762,1.590,0.715;取β值的近似值分别对AGI、APACHEⅡ、SOFA、平均年龄重新赋分:AGI≥2分(2分),AGI<2分(0分)。APACHE Ⅱ≥21分(1分)、APACHE Ⅱ<21分(0分);SOFA≥7(2分)、SOFA<7分(0分);年龄≥71岁(1分)、年龄<71岁(0分)。重新评定两组患者的AGI、APACHE Ⅱ、SOFA、年龄得分,每个患者所得分值全部相加为该患者的死亡预警评分。以死亡预警评分、AGI、APACHE Ⅱ、SOFA评分为检验变量,死亡或存活为状态变量,绘制ROC曲线(图2,封三),结果提示:死亡预警评分的AUC值高于AGI评分、APACHE Ⅱ评分和SOFA评分,差异均有统计学意义(P<0.05)(表5)。
3讨论
危重症病情相对复杂,患者的基础健康状态、原发病的严重程度、治疗过程中是否发生脏器功能衰竭均能影响危重症患者的预后。危重症患者受创伤和感染的影响,发生全身应激反应,血管收缩、胃肠道供血减少、缺血缺氧导致胃肠黏膜屏障受损,从而引发肠腔内的菌群紊乱及其毒性产物移位,促发全身炎症反应,加重多器官功能障碍[7-8],最终发生脓毒症,脓毒症是危重症患者病情严重的表现。ICU重症患者中约59%存在胃肠功能障碍[2,9]。因此对危重症患者的胃肠功能进行针对性的评估以指导临床实施优化的治疗干预成为当前亟待研究的目标[10],得到临床医生的高度重视。在重症医学领域,“胃肠功能障碍”被称为“AGI”[11]。2012年欧洲重症医学会制定了《关于AGI的定义和处理指南》,来规范AGI的诊治。近年来,多项研究表明重症患者的AGI与不良预后密切相关[12-14]。本研究结果显示,出现AGI的占总例数的74.47%(490/658)。死亡组患者7 d内AGI分级达到2级及以上的占死亡患者的89.29%,与既往研究相符[15]。证实AGI普遍存于危重症患者中,可以作为危重症患者疾病严重程度和转归的评估工具之一。本研究中死亡组患者1周内AGI评分的ROC曲线的AUC为0.796,>0.7,证实AGI能较好地预测危重症患者的不良预后,与既往研究一致[16]。
危重症患者的病情评估工具常用的有APACHE Ⅱ评分、SOFA评分、MODS评分、MEWS系统。其中APACHE Ⅱ应用最广,在危重症入院24 h内完成,包含年龄、急性生理指标、慢性健康状况,对患者病情评估全面,不含AGI项目。而SOFA只有胆红素指标一项不能把胃肠道的评估全部概括,而MEWS仅含有心率、呼吸频率、血压,神志等项目,完全无胃肠道的评估。为此研究一种包含AGI在内的新评分系统来更全面地评估危重症的预后意义重大。但过于繁琐的评估项目又不能广泛应用于临床,而AGI评分比较简单,实用性强。目前国内已有研究将胃肠功能评估与APACHE Ⅱ、SOFA等评分系统联合起来评估脓毒症患者的预后,结果显示可以获得更好的预测价值[17-18]。在本次研究中,APACHE Ⅱ、SOFA评分的AUC均>0.7,提示对重症患者的预后评估均有较好的价值。再将AGI联合APACHE Ⅱ、SOFA、MODS評分系统纳入研究,进入Logistic回归模型的有AGI评分≥2分、APACHE Ⅱ评分≥21分、SOFA评分≥7分、年龄≥71岁均是危重患者死亡的独立危险因素(P<0.05)。将包括上述4个指标在内的新评分系统定义为死亡预警评分,绘制ROC曲线,得出其预测危重症患者死亡的AUC为0.909,大于单用AGI、APACHE Ⅱ、SOFA评分的AUC值,差异均有统计学意义(P<0.05)。提示本研究的死亡预警评分在预测危重症患者死亡时具有较高的预测价值。本研究证实死亡预警评分综合了包括胃肠功能在内的多种因素,可以更加全面地评估危重症患者的预后,对死亡患者的预测价值高于单独使用一种评分。
综上所述,由AGI分级联合包括APACHEⅡ、SOFA评分等在内的新评分系统能更准确地预测危重症患者死亡的发生,临床推广应用后能指导早期的优化干预,从而降低危重症患者的病死率。
[参考文献]
[1]陈薇薇,陈尔真.重症病人胃肠功能评估的研究进展[J].外科理论与实践,2016,21(2):177-180.
[2]王艳,王建荣,唐晟.危重患者急性胃肠损伤现状及影响因素的调查研究[J].国际消化病杂志,2017,37(1):54-58.
[3]Singer P,Blaser AR,Berger MM,et al.ESPEN guideline on clinical nutrition in the intensive care unit[J].Clin Nutr,2019, 38(1):48-79.
[4]邹圣强,朱小芳,乔瑶.ICU脓毒症患者肠内营养喂养不耐受的危险因素调查[J].中华灾害救援医学,2017,5(9):498-501.
[5]邓云霞,徐正梅,孙志琴.肠内营养输注速度对呼吸衰竭机械通气病人腹内压和肺顺应性的影响[J].肠外与肠内营养,2016,23(4):254-256.
[6]姚洋,江航帅,许宣宣.ICU患者肠内营养喂养不足危险因素分析及预防措施[J].中国预防医学杂志,2019,20(8):699-702.
[7]李雯静,廖吕钊,王希,等.急性胃肠损伤状态下肠粘膜屏障的受损机制[J].浙江医学,2018,40(19):2194-2196.
[8]王慧芳,王方岩,常平.肠道微生态与脓毒症[J].中华危重症医学杂志(电子版),2018,11(6):415-419.
[9]雍陟,章美元,范志文,等.危重症患者急性胃肠损伤血清学评估的研究进展[J].内科急危重症杂志,2020,26(1):19-21.
[10]范雨恬,蒋钰,王欣君.危重病人胃肠功能评价及干预优化研究[J].中医临床研究,2019,11(26):146-148.
[11]李洪祥,王育珊.重症患者急性胃肠功能障碍诊断余治疗进展张[J].当代医学,2019,25(24):1-5.
[12]Chelakkot C,Ghim J,Ryu SH.Mechanisms regulating intestinal barrier integrity and its pathological implications[J].Exp Mol Med,2018,50(8):103.
[13]陈莹,陈蕾,李克清,等.ICU机械通气患者急性胃肠损伤的调查研究[J].实用医学临床杂志,2017,14(3):117-119.
[14]赵建,苏和.脓毒症急性胃肠功能损伤评估的研究进展[J].医学食疗与健康,2020,2(4):210-211.
[15]刘雪媛.预测危重创伤患者死亡的一种新评分系统:死亡预警评分的预测价值[D].遵义:遵义医学院,2016.
[16]董科奇,邓杰,潘景业,等.急性胃肠损伤分级联合序贯器官衰竭评估对严重脓毒症预后评估的价值[J].中国全科医学,2017,20(5):526-532.
[17]魏宜,陈蕊,胡英芳,等.脓毒症患者早期急性胃肠功能损伤2种分级标准评估的临床研究[J].汕头大学医学院学报,2019,32(1):31-33,40.
[18]王擂,刘淑丽,田翠,等.ICU住院患者急性胃肠损伤与APACHEⅡ评分的相关性分析[J].山东医药,2015,55(12):82-83.
(收稿日期:2020-06-15)
