Is the Bismuth-Corlette IIIb stage really an unfavorable situation for resectability of Klatskin tumors? A critical appraisal
2020-10-23MarcelloDonatiMichelaZanattaFrancescoBasile
Marcello Donati , Michela Zanatta, Francesco Basile
Department of Surgery and Medical Surgical Specialties, Surgical Clinic Unit, University Hospital of Catania, 95123 Catania, Italy
TotheEditor:
We read with considerable interest the paper from Passeri et al.[1]questioning how the IIIb preoperative determination of a Klatskin tumor could be considered a risk factor for unresectability,and we could not refrain from making some critical recommendations about it.
Although the paper was nicely written, in our opinion, no meaningful conclusion should however be drawn from it, due to the small sample size of the reported series.
As outlined in the introduction, only type IIIa and IIIb can be considered for resection and not Bismuth-Corlette IV [2];in our opinion, this is questionable because Klatskin tumors can be resected depending on surgical skills and on dissection/reconstruction ability of the surgeon [3].Therefore, “resectability”judgement of Klatskin tumors is largely depending on experience and ability of the surgeon, and it can be precisely finally assessed only after a careful dissection of hilar structures.Passeri et al.[1]also stated that IIIb tumors would result in a higher likelihood of unresectability because of right artery crossing under left hepatic duct.On the contrary, it could be argued that IIIb tumors are more likely to be resectable for three main reasons:left hepatic duct is longer than the right one (and so more likely to be derived even inside the hilar plaque through a biliodigestive anastomosis) ( Fig.1 ); for the same reason, the left hepatic artery is longer than the right one and more prone to be switched on the right side to reconstruct the right one.The left artery could be completely resected without any reconstruction when an accessory left hepatic artery is present.Furthermore, an arterial reconstruction, especially if involving left artery, is easier with the Dokmak’s patch [4], introduced firstly for venous reconstructions but even suitable for arterial ones [5].However, we must underline that arterial resection has considerable mortality rate and not all centers are capable of performing arterial resection and reconstruction.
The third reason is that very often the IIIb can result in a higher chance of resectability due to greater volumetry of future liver remnant: this condition is strongly affecting resectability judgement due to cholestatic conditions.
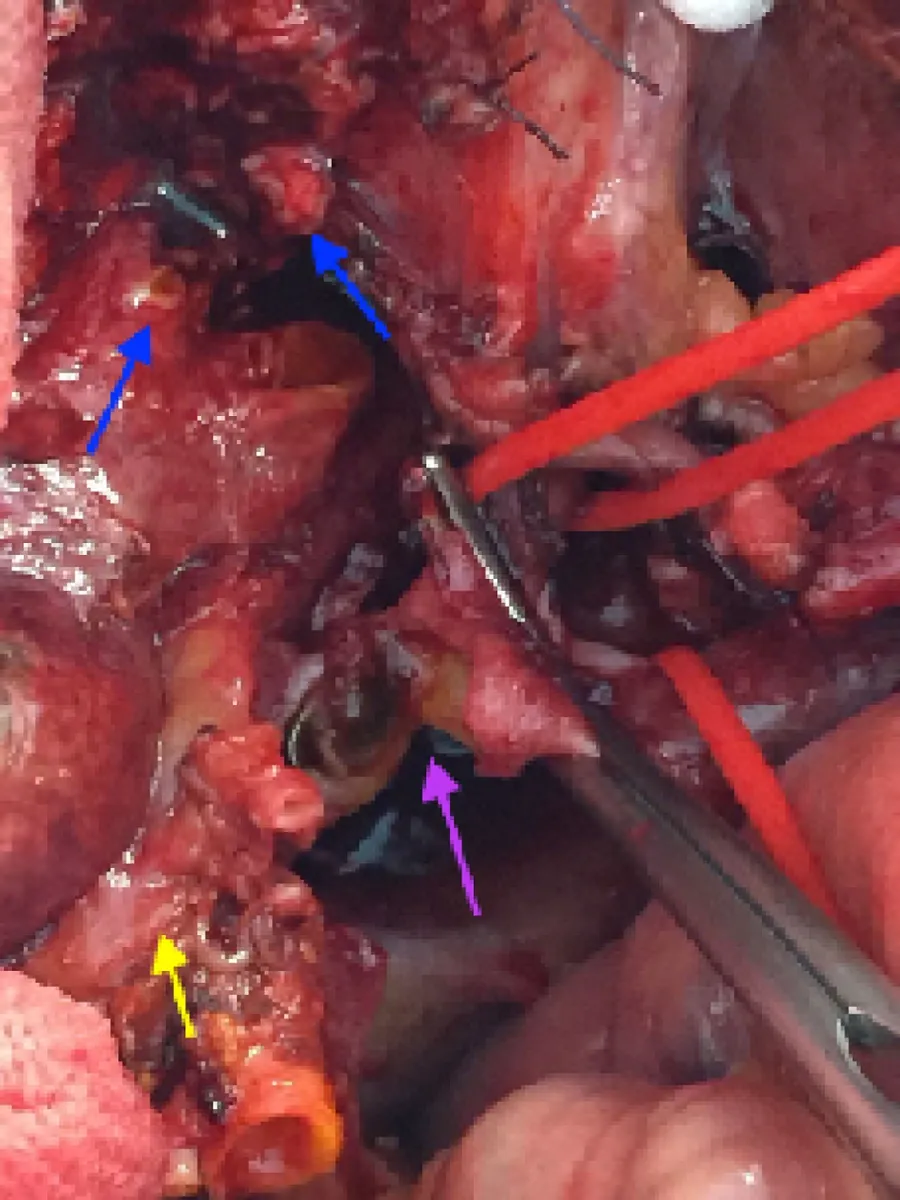
Fig.1.Example of fine dissection of hilar structures of a Klatskin tumor type IIIa(yellow arrow) with long left hepatic duct.The tumor is infiltrating the portal bifurcation; the portal bifurcation (violet arrow) is resected.The left hepatic duct is resected en-block with the right hepatectomy specimen (blue arrows show 2nd order branches after complete resection of left hepatic duct to be derived in a biliodigestive anastomosis).
Moreover, no clear definition of “unreseactable disease” has been given in the paper by the authors (again confirming that resectability judgement for Klatskin tumors largely depends on surgical skills), so no R0, R1 and R2 data among resected patients were reported.Additionally, 21% of resected patients did not receive an oncologically radical resection, given that no liver resection was associated [3].
On the other side, Klatskin type IIIa with the involvement of right side more often could become unresectable: in those cases, a concomitant liver resection becomes a “must”of this surgery, but cholestatic conditions frequently hinder a radical resection of those tumors due to the high loss of volume of right trisectionectomies [2].
In summary, the data are not supporting the conclusions of the paper; despite that, on the other side, we can agree with the authors when they state that a IIIb type should induce surgeons to consider a more likelihood of arterial reconstruction.
Acknowledgments
None.
CRediT authorship contribution statement
Marcello Donati:Conceptualization, Writing - original draft.Michela Zanatta:Resources, Writing - review & editing.Francesco Basile:Supervision, Writing - review & editing.
Funding
None.
Ethical approval
Not needed.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Fecal microbiota transplantation has therapeutic effects on chronic hepatits B patients via altering composition of gut microbiota
- The Janus of mIS in hepatobiliary surgery: Importance of maximally invasive surgery in an era of minimally invasive surgery
- Liver injury in COVID-19: What do we know now?
- Hepatic abscess resulted from a toothpick piercing the gastric wall into the liver
- Pancreatoblastoma: A rare indication for liver transplantation in children
- Optimized liver resection range and perioperative safety in patients with high levels of indocyanine green R15