Optimized liver resection range and perioperative safety in patients with high levels of indocyanine green R15
2020-10-23RuiTngXinJingZhngMengJioLioAngLiWenPingZhoQinLu
Rui Tng , Xin-Jing Zhng , Meng-Jio Lio , b , Ang Li , Wen-Ping Zho , Qin Lu , ∗
a Hepatopancreatobiliary Center, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Institute for Precision Medicine, Tsinghua University,Beijing 102218, China
b Department of General Surgery, the Fifth Affiliated Hospital of Zunyi Medical University, Zhuhai 519100, China
TotheEditor:
The indocyanine green (ICG) clearance test is an objective measurement of functional liver reserve (FLR) [1].The liver can preserve normal functions with a 70% −80% functional liver volume resection [2]and the remnant is capable of regeneration.However, liver regenerative properties are affected by hepatitis, fatty liver, cirrhosis and damage caused by chemotherapy [3].ICG combined with the Child-Pugh score are main criteria for evaluating FLR.A safe hepatectomy procedure requires the remnant liver to be 25% −30% of the normal volume.For patients with an indocyanine green retention rate at 15 min (ICG-R15)>20%, segment liver resection, limited hepatectomy or tumor enucleation is recommended, but there has been no clear clarification of the essential remnant liver volume [4].In China, the experts’ consensus of preoperative evaluation of liver reserve function incorporates ICGR15 tests.R SE [essential functional liver volume (EFLV)/standard liver volume (SLV)]is introduced to evaluate the safety of hepatectomy [5].For patients with ICG-R15 levels between 20% and 30%, R SE = 80% and those with an ICG-R15 level range of 30% −40%or>40%, safe surgeries like limited hepatectomy and tumorectomy are recommended [6].There is a paucity of studies that focus on surgical safety for patients with an ICG-R15>20%.Herein we aimed to evaluate safe liver resections in these patients.
Patients who underwent hepatectomy were enrolled and the inclusion criteria were: 1) pre-operation ICG-R15>20%; 2) had undergone hepatectomy; 3) had complete clinical data of the patient.Patients with obstructive jaundice were excluded.Clinical data of 11 hepatectomy cases from 10 patients who had high levels of ICG-R15 (>20%) were collected.Surgical procedures, changes in liver volume, postoperative complications and postoperative bilirubin levels were analyzed (1 patient underwent 2 hepatectomy treatments listed as case G/J in Table 1 ).We compared this case series with the criteria formulated by Makuuchi [4](Tokyo University criteria) and the Chinese experts’ consensus (2019 version) [6]on the association between functional liver reserve and liver resection volume.The parameters analyzed included: preoperative value of ICG-R15, grade of liver cirrhosis, pre- and postoperative bilirubin levels, postoperative complications, and mortality.SLV (cm3) = 706.2 ×body surface area (BSA) (m2) + 2.4 [7], with the functional liver volume remnant in surgical planning (RFLV) and non-neoplastic liver volume (nNLV) evaluated by 3-dimentional(3D) reconstruction using Iqqa-Liver software (EDDA technology,Princeton, NJ, USA) based on CT scans.The actual functional liver volume remnant (AFLV) was evaluated based on the first CT scan after surgery.Liver failure was defined as a postoperative total bilirubin level>171 μmol/L, bile leakage as the bilirubin concentration in drainage fluid ≥3 times serum levels on or after postoperative day 3, and ascites as drainage>10 mL/kg · d.The median age of the patients was 61 (33-74) years with a median body surface of 1.85 (1.77-2.33) m2.The median length of hospital stay after surgery was 12 (6-33) days, while no mortality during perioperative period occurred.Postoperative complications occurred after 5 hepatectomies (case A, B, C, F, I) as ascites, in 1 (case A)as bile leakage accompanied by pleural fluid and pulmonary infection, in 1 (case F) as poor incision healing and in 1 (case J) grade-I left portal vein thrombosis with stage-I hepatic encephalopathy.The postoperative mortality rate was 40% (4/10), which occurred 2 months after surgery (case B after recurrence 1 month after operation treated with radiologic interventions 2 times and case F after abdominal lymph node recurrence 1 month after surgery),6 months after first surgery (case J after recurrence 3 months after the first operation treated with a second resection) and 27 months after surgery (case K after recurrence 9 months after operation treated with radiofrequency ablation at the same time followed by radiologic interventions), respectively.Two patients survived up to now after recurrence 15 months after operation treated with radiologic interventions (case C, 41 months) and lung metastasis 11 months after surgery treated with sorafenib (case I, 31 months).Four patients (case A 28 month, case D 52 months, case E 21 months and case H 33 months) survived up to now without recurrences and post- surgical interventions.
Among the 11 hepatectomies, 8 were for hepatocellular carcinoma (HCC) and 3 for hepatic alveolar echinococcosis, high-grade mucinous cystic adenoma and liver cirrhosis nodule with highgrade heterotypic hyperplasia.The ICG-R15 values ranged from 20.1% to 61.0%, among which 6 were between 20% and 30% (case A-F), 4 between 30% and 40% (case G-J) and 1>60% (case K).
In HCC patients, the tumor sizes ranged from 1.5 to 17 cm.Three patients received transcatheter arterial chemoembolization (TACE)treatment before surgery (case F, I, K), resulting in large necrosis of the main HCC lesion; residual tumor lesions were found in 2 cases(case F, K).One patient (case A) underwentexvivohepatectomy and autologous graft re-transplantation, 1 (case B) right posterior lobectomy with removal of portal vein tumor thrombus, 1 (case C) right posterior lobectomy, 1 (case I) right hemi-hepatectomy and 1 (case E) left hemi-hepatectomy.Six treatments (case D, F,G, H, J, K) comprised local resections.Preoperative bilirubin levels ranged from 8.4 to 33.4 μmol/L and postoperatively from 24.2 to 133.3 μmol/L ( Table 1 ).
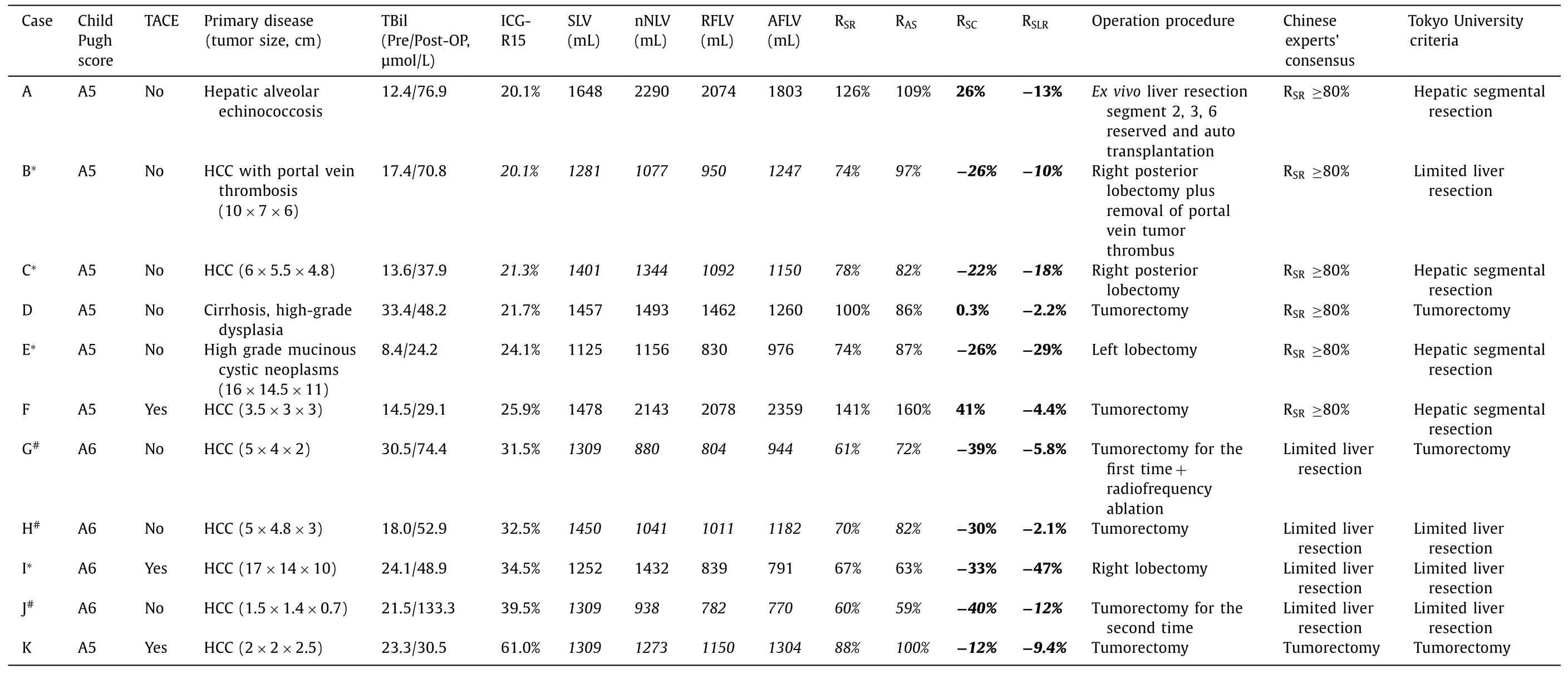
Table 1Functional liver volume index, operationp rocedures andsituations of surpassing standard.
SLV ranged from 1125 to 1648 mL, and the RFLVs were 782-2078 mL; the standardized ratio of the functional liver volume remnant (R SR = RFLV/SLV) ranged from 60% to 141%.While the AFLV after surgery ranged from 770 to 2359 mL, the standardized ratio of AFLV (R AS = AFLV/SLV) ranged from 59% to 160%, with no difference between R SR and R AS (P= 0.325).The standardized ratio of standard liver volume changes [R SC = (RFLV-SLV)/SLV]ranged from −40%to 41% and for the standardized ratio of functional liver volume resection expected [R SLR = (RFLV- nNLV)/SLV]from −47% to −2.1%.In the hepatectomy subgroup with nNLV Four patients exceeded both criteria sets (case B, C, E, I), and 3 had liver fibrosis but no obvious cirrhotic nodules.Among other hepatectomy cases, R SR was ≤70% in 3 cases with local liver resection (case G, H, J).The hepatectomy case J was with the lowest RSRvalue (60%) and the patient suffered the most serious postoperative complications. Most patients with HCC suffered chronic hepatic virus infection,followed by hepatic fibrosis and liver cirrhosis, elevated serum bilirubin levels and ascites postoperatively.The results of ICG-R15 can be influenced by many factors.For large tumors, it could affect ICG-R15 through decreased liver blood flow, compressed adjacent liver parenchyma or a deficiency in normal liver remnant.In case I, liver fibrosis, but no cirrhotic nodule was found during operation, but the patient had a higher ICG-R15 level than patients with liver cirrhosis.The surgical borderline was in accordance with the pre-operative results of 3D surgical planning.In the Chinese experts’ consensus, for patients with ICG-R15 between 20% and 30%,an R SR ≥80% is required for a safe hepatectomy procedure, while segmentectomy was recommended by Tokyo University criteria.We believe that limited hepatectomy is a controllable small-scale surgery procedure with maximal functional liver parenchyma reserved based on tumor volume and surrounding infiltration properties, including anatomical resection (AR) and non-anatomical resection (NAR). There was no difference in prognosis after AR and NAR resection for HCC with a tumor size smaller than 2 cm or larger than 5 cm, while AR resection had a better prognosis for a HCC range from 2 to 5 cm.NAR was applied to hepatectomy case J because the tumor size was smaller than 2 cm.There were 4 hepatectomies(case F-H, K) for tumors ranging from 2 to 5 cm who underwent NAR.Hepatectomies G and H included pseudo-capsules and cases F and K received TACE treatment before their operations and underwent NAR.Cases B, C and I, with tumor sizes>5 cm, underwent AR because the tumor occupied almost the whole hepatic lobes or was close to the main pedicle. There were no perioperative deaths in patients who surpassed both sets of criteria.For patients with liver cirrhosis and atrophy,the preoperative functional liver volume was<80% of the standard(nNLV/SLV We found that R SR was low even for limited liver resections when nNLV was small, especially in patients whose nNLV was Among the 4 cases surpassing both sets of criteria, obvious cirrhotic nodules were found only in case C.It was different in patients (such as case H) with similar ICG-R15 ranges, but with obvious cirrhotic nodules, who received tumorectomy.The relationship between pathologically diagnosed liver damage and the ICG-R15 level needs to be studied further to evaluate the non-tumor regions functional liver volume.Most patients showed hepatic proliferation and some had a larger functional liver volume than preoperation.One patient suffered hepatic encephalopathy, accompanied by a portal vein thrombosis.The Pringle maneuver during hepatectomy decreased functional liver volume and fresh frozen plasma can prompt the formation of a portal vein thrombosis.Hepatectomy may be avoided if liver transplantation is an option.In addition, radiofrequency ablation, TACE and laparoscope operations are also options for decreasing operative trauma and accelerating patient recovery. We conclude that limited liver resection is a safe procedure for patients with high levels of ICG-R15.Future research should include postoperative ICG-R15 levels, which are helpful in assessing post-operation prognosis. Acknowledgments None. CRediT authorship contribution statement Rui Tang:Conceptualization, Data curation, Formal analysis,Writing - original draft.Xin-Jing Zhang:Conceptualization, Formal analysis, Writing - original draft.Meng-Jiao Liao:Data curation,Writing - original draft.Ang Li:Data curation.Wen-Ping Zhao:Data curation.Qian Lu:Conceptualization, Formal analysis, Funding acquisition, Writing - review & editing. Funding This study was supported by a grant from the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support ( ZYLX201712 ). Ethical approval This study was approved by the Ethics Committee of Beijing Tsinghua Changgung Hospital. Competing interest No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Fecal microbiota transplantation has therapeutic effects on chronic hepatits B patients via altering composition of gut microbiota
- The Janus of mIS in hepatobiliary surgery: Importance of maximally invasive surgery in an era of minimally invasive surgery
- Liver injury in COVID-19: What do we know now?
- Is the Bismuth-Corlette IIIb stage really an unfavorable situation for resectability of Klatskin tumors? A critical appraisal
- Hepatic abscess resulted from a toothpick piercing the gastric wall into the liver
- Pancreatoblastoma: A rare indication for liver transplantation in children