Pancreatoblastoma: A rare indication for liver transplantation in children
2020-10-23MriMerdlHllySuhetVidyHetorVilMelendezNigelHetonAnilDhwnTssosGrmmtikopoulos
Mri Merdl-Hlly , Suhet Vidy , Hetor Vil-Melendez , Nigel Heton ,Anil Dhwn , , Tssos Grmmtikopoulos , , ∗
a Paediatric Liver, GI, Nutrition Centre and MowatLabs, King’s College Hospital NHS Foundation Trust, Denmark Hill, London SE5 9RS, UK
b Department of Paediatric Oncology, The Royal Marsden Hospital, Sutton, London SE5 9RS, UK
c Institute of Liver studies, King’s College Hospital NHS Foundation Trust, Denmark Hill, London SE5 9RS, UK
TotheEditor:
Pancreatoblastoma (PB) is one of the exocrine pancreatic tumors and the most common malignant pancreatic tumor in young children.Patients can present with abdominal distension, pain, fatigue, vomiting and failure to thrive.Exocrine pancreatic tumors usually affect patients between 1 and 8 years, with a median age of 5 years.There is a slight preponderance in males and those of Asian descent [1].PB is considered to be embryonic in origin with moderately raised serum alpha-fetoprotein (AFP) levels [2].Axial imaging is necessary to assess other organ involvement, a common complication in adult patients, but diagnosis is confirmed on tissue histology [3].Complete surgical resection is the treatment of choice, if achievable.Indications for neoadjuvant systemic chemotherapy include large tumors that involve adjacent major blood vessels or other organs and metastatic disease [1].Herein we report a pediatric case of PB with liver metastases who underwent liver transplantation for metastatic liver disease.
A 7-year-old girl was referred to our center after presenting to her local hospital with a 3-week history of abdominal distension and pain.At the time of diagnosis abdominal computed tomography scan showed an irregular soft tissue mass with a calcified cystic component, occupying the pancreas and extending to the mesenteric root, portal vein (PV) and also with tumor involvement of the spleen ( Fig.1 A and B).AFP was 2275 ng/mL and diagnosis was confirmed on histology.The patient received six courses of preoperative chemotherapy with cisplatin and doxorubicin with dose modification due to drug toxicity (renal tubular leak and prolonged myelosuppression).She received a total cumulative dose of 330 mg/m2of doxorubicin and 540 mg/m2of cisplatin with intermittent granulocyte-colony stimulating factor (G-CSF) support.After receiving 2 cycles of chemotherapy she was re-evaluated and magnetic resonance imaging showed significant reduction in the tumor volume with development of PV cavernoma ( Fig.1 C and D)and normalization of AFP.At that point the tumor was deemed resectable with total or partial pancreatectomy but in view of unresectable liver metastases and PV infiltration, a liver transplant was inevitable.The child was listed as priority in the UK liver transplant registry.
One month after her last cycle of chemotherapy and while the child had residual liver metastases on axial imaging, a suitable donor liver became available.At laparotomy a large pancreatic tumor arising from the tail of the pancreas in conjunction with splenic vein thrombosis and segmental portal hypertension was evident.The pancreas and spleen were mobilized.The PV was mobilized to the junction of the superior mesenteric vein (SMV)and splenic vein (SV).The PV was thrombosed with cavernous transformation.The cavernoma was excised and a venous (cadaveric iliac vein) interpositional graft was anastomosed to the SMV and SV junction.The donor PV was anastomosed to the interpositional venous graft with interrupted stitches.Both top and bottom caval clamps were taken offrestoring caval flow with retrograde perfusion of the liver.Portal clamps were taken offwith good flow noted.The donor’s left hepatic artery was anastomosed to the recipient’s right hepatic artery.The left hepatic duct was anastomosed to a Roux-Y-loop hepaticojejunostomy.A left lateral segment liver graft [332 g, graft-to-recipient weight ratio<0.7, donor/recipient cytomegalovirus (CMV) + / + , Epstein-Barr virus(EBV) + / + , toxoplasma -/-]from a young female donation after brain death (DBD) was transplanted.The donor left hepatic vein was triangulated and anastomosed to the native inferior vena cava(IVC).The anterior sutures were interrupted and these were ligated after liver was flushed through the PV with normal saline.A distal pancreatectomy with splenectomy was performed.
Her postoperative period was unremarkable apart from a small right subphrenic hematoma (7.7 ×2.4 cm), which resolved spontaneously.She developed chylous ascites and was kept on a low fat diet for 4 weeks.Before and after liver transplant the glycemic control was achieved without insulin and standardized for body weight protein and carbohydrate intake.HbA1c levels remained normal.Histology showed the tumor to be necrotic tissue with an obliterative venopathy, no residual viable tumor and clear resection margins.
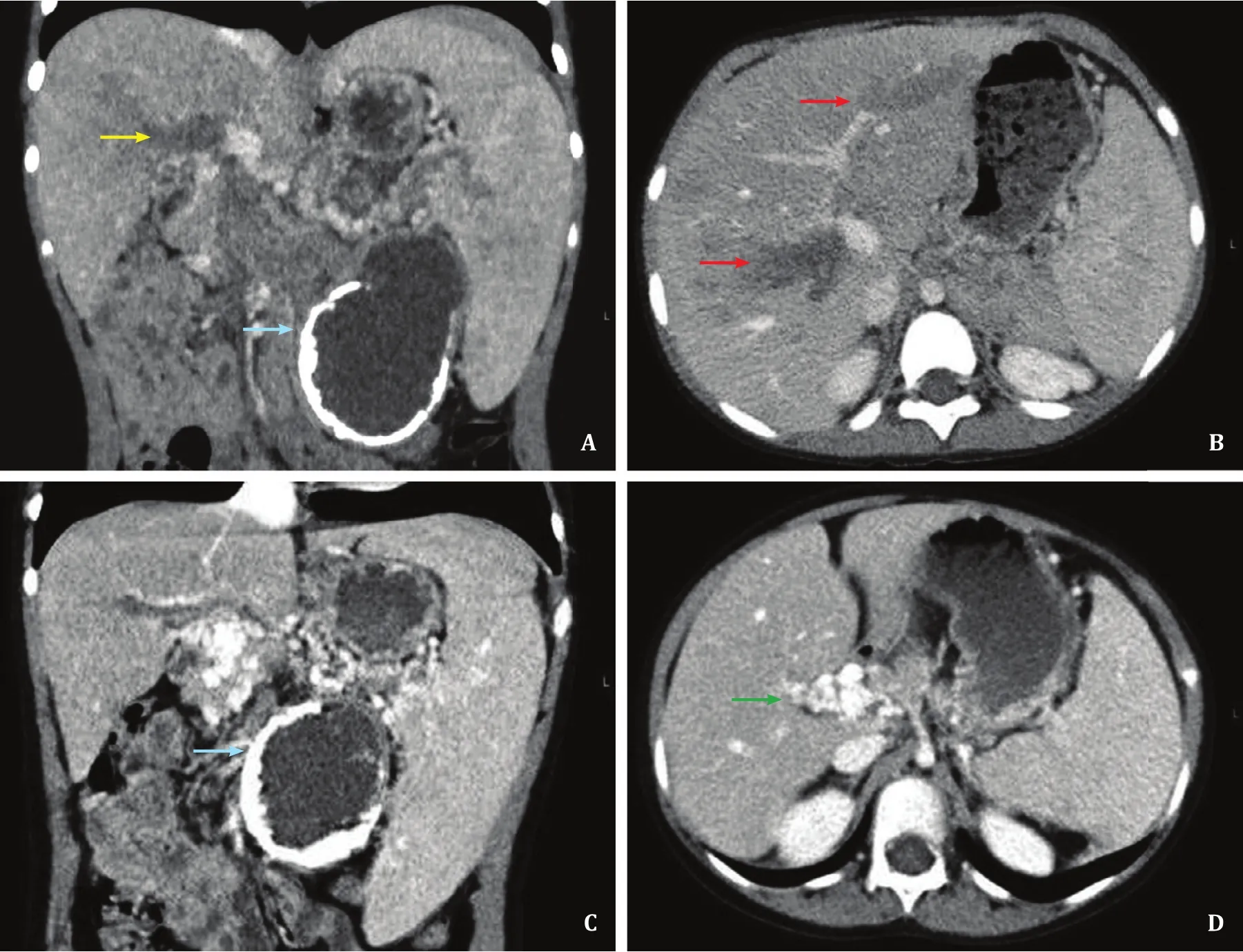
Fig.1.Abdominal computed tomography images at time of diagnosis showing irregular soft tissue mass with a calcified cystic component (blue arrow), occupying the pancreas and extending to the mesenteric root, portal vein (PV) infiltration (yellow arrow) with cavernous transformation and also with tumor involvement of the spleen and liver (red arrows) ( A and B).Following two cycles of chemotherapy magnetic resonance imaging showed significant reduction in the tumor volume with PV cavernoma(green arrow) ( C and D).
Immunosuppression was initiated on day 1 as per standardized protocol with 2 mg/kg methylprednisolone for 3 days weaned to 1 mg/day and oral tacrolimus with initial trough levels of 8-10 mg/dL and later of 4-6 mg/dL.She was given prophylactic antibiotics (tazocin and gentamicin), which were stopped after 8 days after liver transplantation.Penicillin prophylaxis as per post-splenectomy protocol was started.No further chemotherapy was deemed necessary.She was followed up with monthly AFP,abdominal ultrasound (US) every 3 months for the 1st year, 3 monthly AFP and abdominal US for the 2nd year, and 6 monthly AFP/abdominal US for the 3rd-5th years after LT, respectively.At four years after liver transplantation, the liver function tests, AFP and abdominal imaging have remained normal with no disease recurrence.
PB is a very rare tumor in childhood hence there is limited experience in its management within the pediatric setting.We reported a child with PB who underwent distal pancreatectomy,splenectomy and simultaneous liver transplant following six cycles of chemotherapy with significant tumor size reduction.The child remains well with no disease recurrence and is on stable immunosuppression 5 years after surgery.The combination of liver transplantation and partial pancreatic resection is a novel approach to PB treatment with liver metastases in children.The goal of PB treatment is complete surgical resection.Indications for neoadjuvant systemic chemotherapy in patients with PB include large tumors that involve adjacent major blood vessels or other organs and/or metastatic disease.Cisplatin and doxorubicin are the recommended treatment with four courses of both agents for fully resectable tumors and six courses for resection with microscopic residual or nodal involvement [ 4 , 5 ].A recent retrospective review from the European cooperative study group for pediatric rare tumors showed that the most preferred regimen was cisplatin 80 mg/m2in continuous 24-h intravenous infusions followed by doxorubicin 60 mg/m2over 48 h (the PLADO regimen), for 4-6 cycles [6].Postoperative chemotherapy for microscopic margin tumor involvement has also been used.Radiotherapy may have a role in the case of incomplete excision or unresectable disease [4]albeit with high morbidity [6].Another treatment option, reported in four adult cases, is auto-transplantation of peripheral blood stem cells (auto-PBSCT) after intensive chemotherapy [6-10].Yonekura et al.reported cases where the tumor had infiltrated the PV.The tumor was treated with neoadjuvant chemotherapy, pancreaticoduodenectomy with PV reconstruction, followed by auto-PBSCT [9].Tanaka et al.reported disease recurrence in the liver after 2 years and their case underwent a second laparotomy and resection followed with further chemotherapy and auto-PBSCT [11].This case remained disease free 10 months postoperatively.PBSCT has not been adopted by pediatric oncology for PB due to the limited evidence.Five-year disease-free survival and overall survival in children have been reported as 58.8% and 79.4%, respectively.Our patient has just completed the five-year follow-up and is well with no complications or recurrence.
To our knowledge liver transplantation has only been reported in five other patients with PB ( Table 1 ).Varkey et al.presented a child with PB involving the PV and SMV in addition to multiple jejunal venous branches [12].The patient was treated with chemotherapy with a 50% reduction in tumor size.Following chemotherapy, the patient received a multivisceral trans-plant, which included the liver, but subsequently died of infectious causes 2 years after transplant (personal communication).Benetatos et al.reported a 7-year-old girl with PB and multiple liver metastases [13], who received 6 cycles of chemotherapy with an excellent clinical response and then underwent a distal pancreatectomy and splenectomy before the liver transplantation.The outcome was not clear.The latest report by Namgoong et al.described a 4-year-old boy with advanced PB infiltrating the PV and SMV after chemotherapy who underwent a total pancreatectomy and living related liver transplant (LRLT) from the mother [14].
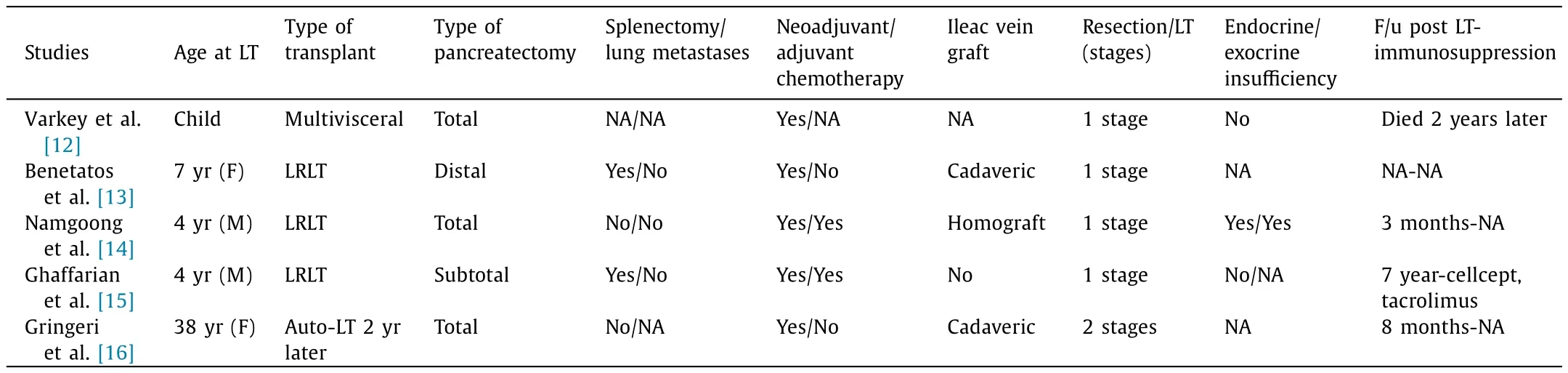
Table 1List of previously reported cases of PB with liver metastases and liver transplantation.
Ghaffarian et al.described a 4-year-old boy with PB and multiple liver metastases who had a single stage surgical treatment with subtotal pancreatectomy 2 days after hepatectomy and LRLT.No disease recurrence was reported seven years on [15].Lastly,Gringeri et al.reported that a 38-year-old female patient with the diagnosis of an unresectable PB had radiotherapy by CyberKnife and adjuvant chemotherapy.Two years later, bilobar metastatic liver lesions were identified and she eventually underwent anexsituexvivoliver resection with simultaneous caval resection.The resected IVC was replaced by an interpositional graft previously anastomosed to a cadaveric saphenous vein to perform a portocaval shunt for the anhepatic phase.Anexsituexvivohepatic wedge resection was performed including the lesion in segments 1-5-7-8, as previously identified and the liver was reimplanted [16].
This case suggests that liver transplantation may have a favorable outcome in children with metastatic liver involvement from PB and could be considered as part of a treatment regime in a pediatric liver transplant center.
Acknowledgments
None.
CRediT authorship contribution statement
Maria Mercadal-Hally:Data curation, Writing - original draft.Sucheta Vaidya:Writing - review & editing.Hector Vilca-Melendez:Writing - review & editing.Nigel Heaton:Writing - review & editing.Anil Dhawan:Writing - review & editing.Tassos Grammatikopoulos:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
The consent was obtained from the patient for publication of this report.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Fecal microbiota transplantation has therapeutic effects on chronic hepatits B patients via altering composition of gut microbiota
- The Janus of mIS in hepatobiliary surgery: Importance of maximally invasive surgery in an era of minimally invasive surgery
- Liver injury in COVID-19: What do we know now?
- Is the Bismuth-Corlette IIIb stage really an unfavorable situation for resectability of Klatskin tumors? A critical appraisal
- Hepatic abscess resulted from a toothpick piercing the gastric wall into the liver
- Optimized liver resection range and perioperative safety in patients with high levels of indocyanine green R15