Predicting common bile duct stones by non-invasive parameters
2020-07-07AnsKdhTwfikKhouryMhmudMhmidNimerAssyWismSeit
Ans Kdh Twfik Khoury Mhmud Mhmid Nimer Assy Wism Seit
a Department of Gastroenterology, Galilee Medical Center, Nahariya, Israel, Faculty of Medicine in the Galilee, Bar-Ilan University, Safed, Israel
b Gastroenterology and Endoscopy Units, The Nazareth Hospital, EMMS, Nazareth, Faculty of Medicine in the Galilee, Bar-Ilan University, Safed, Israel
c Department of Internal Medicine, Galilee Medical Center, Nahariya, Israel, Faculty of Medicine in the Galilee, Bar-Ilan University, Safed, Israel
Keywords:Stones Common bile duct Predictors
A B S T R A C T Background: Common bile duct (CBD) stone affect about 10% of patients with symptomatic cholelithiasis.The American Society for Gastrointestinal Endoscopy (ASGE) published a strategy in 2010 for managing patients with suspected choledocholithiasis. This study aimed to assess the performance of different clinical parameters in predicting CBD stones.Methods: A total of 344 patients suspected to suffer from CBD stone and referred to endoscopic ultrasound (EUS) were included. Parameters were collected and their prediction power for CBD stones was assessed.Results: One hundred and sixty-seven patients without CBD stone according to EUS (group A) were compared to 177 patients with CBD stones (group B). Several predictive factors for CBD stone were identified on univariate analysis. In multivariate regression analysis, CBD width by US (OR = 1.224, 95% CI:1.073-1.359; P = 0.0026), age (OR = 1.023, 95% CI: 1.011-1.035; P = 0.0 0 02) and gamma glutamyl transferase (GGT) level (OR = 1.001, 95% CI: 1.000-1.002; P = 0.0018) were significantly correlated with CBD stone, with receiver operator characteristics (ROC) of 0.7259. We generated a diagnostic equation [age(yr) ×0.1 + CBD width (mm) by US ×1 + GGT (U/L) ×0.005] to predict CBD stone with ROC of 0.7287.Conclusions: We suggest this score as a very strong predictor for CBD stones, and to reduce the strength of total bilirubin and transaminases as predictors.
Introduction
Gallstones are a major health problem in the developed countries. The overall prevalence among adult population in North American and Europe ranges between 10% −20% [1 , 2] . I t’s well known that the prevalence of common bile duct (CBD) stone increases with age [3] . The prevalence of CBD stone increases from 14% in patients less than 70 years old, to 32% in patients over 70 years in a group of patients referred for endoscopic ultrasound(EUS) [4] , and about 1% of the general population suffer from CBD stone. Before the era of EUS and magnetic retrograde cholangiopancreatography (MRCP), patients were referred to diagnostic endoscopic retrograde cholangiopancreatography (ERCP) which carries life threatening events such as: 1.3% −6.7% risk of pancreatitis, 0.6% −5% risk of infection, 0.3% −2% risk of hemorrhage, and 0.1% −1.1% perforation risk, in addition to the high cost of the procedure [5-7] . In over 50% of cases, no CBD stone was seen during ERCP, and therefore, these patients underwent unnecessary procedure [8 , 9] , making its risk-benefit profile unsatisfactory. Since the introduction of EUS in 1990 [10 , 11] , the need for ERCP was obviated in about 67% of cases [12] .
Although no single parameter consistently predicts CBD stone strongly, many investigators have noted that the combination of multiple predictors improves diagnostic accuracy of CBD [3 , 4 , 13] .
The American Society for Gastrointestinal Endoscopy (ASGE)published a proposed strategy in 2010 to assign patients with suspected CBD stone to undergo either a diagnostic modality (EUS,MRCP, laparoscopic intra-operative cholangiography or laparoscopic ultrasound) or therapeutic ERCP. This strategy was based on clinical, laboratory and ultrasonography predictors, and the patients were categorized according to the strength of these predictors into low (<10%), intermediate (10% −50%) and high (>50%) probability for CBD stone. Only patients with high probability for stones should be referred to ERCP, while those with intermediate probability should have confirmatory diagnostic examination, before therapeutic decision making [14] .
The present study aimed to develop a simple non-invasive scoring system to stratify patients presenting with suspected CBD stone into high- and low-risk groups using routinely determined and easily available clinical, laboratory and radiological variables.
Methods
Patients
The study cohort consisted of all patients above 18 years old referred to EUS with a presumptive diagnosis of CBD stone from January 2012 to January 2016 at Galilee Medical Center, Israel. All patients had the data of pre-EUS laboratory tests and trans-abdominal US. In our medical center, EUS is the procedure of choice for suspected CBD stone. Recent review article has found that EUS has high sensitivity of 84% −100% and specificity of 94% −100% in detecting CBD stone [15] and EUS has recently been proposed as the new gold standard in the diagnosis of CBD stone [16] . Our exclusion criteria were: (1) patients suffering from cholangitis who were proceeded to ERCP without performing EUS; (2) patients with definite CBD stone diagnosed by US or CT; (3) patients suffering from chronic liver diseases whose liver function tests could be disturbed as a result of these diseases; and (4) patients with elevated liver enzymes secondary to different causes other than CBD stone, including alcoholic liver disease, drug-induced liver injury, autoimmune hepatitis, viral hepatitis, cholestatic liver diseases and metabolic/genetic liver disease.Furthermore, we excluded patients with unclear CBD dilation, CBD stricture and malignancy.
All medical records of eligible patients were reviewed, and the following parameters were collected: demographic data [age and sex, laboratory tests (alanine aminotransferase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), total bilirubin (TBil), white blood cells (WBC)],and radiologic findings [CBD stone, CBD width as assessed by US].CBD width up to 6 mm was considered normal; while greater values were considered dilatation of the duct. The statistical comparison was performed between patients with confirmed CBD stone to patients without CBD stone as assessed by EUS. The parameters included in the univariate and multivariate analysis were laboratory and CBD width by trans-abdominal US.
All EUS examinations throughout the study were performed by an experienced endoscopist (SW) with high volume examinations and an over 15 years’ experience in the field of advanced endoscopy.
Statisticalanalysis
The main endpoint of the study was to predict the presence or absence of CBD stone by a combination of simple available clinical,radiological and laboratory relevant variables. Univariate descriptive statistics was used to compare patients with and without CBD stone. Data was reported as mean ±standard deviation for quantitative continuous variables, and frequencies (percentages) for categorical variables. Univariate and multivariate logistic regression were used to estimate odds ratio (OR). Factors were selected for the multivariate model, based on clinical knowledge and effect sizes. Backward selection was used to select variables for the final model; a cut-off point for CBD width by US was performed using receiver operating characteristics (ROC) analysis with the Youden index reported. In order to generate a new regression equation that included all parameters that were statistically significant in multivariate analysis (age, CBD width by US and GGT level), we attributed weights to each of the factors according to rounded coeffi-cient estimates in the multiple logistic regression model. The overall diagnostic accuracy of the scoring system was determined byROC curve. Finally, we determined the diagnostic accuracy of the cut-off points generated using this formula by calculating sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). A significance level ofPvalue of<0.05 was considered significant. All analyses were performed by an experienced statistician and were carried out using the statistical analysis software (SAS Vs 9.4 Copyright©2016 by SAS Institute Inc., Cary, NC,USA.)
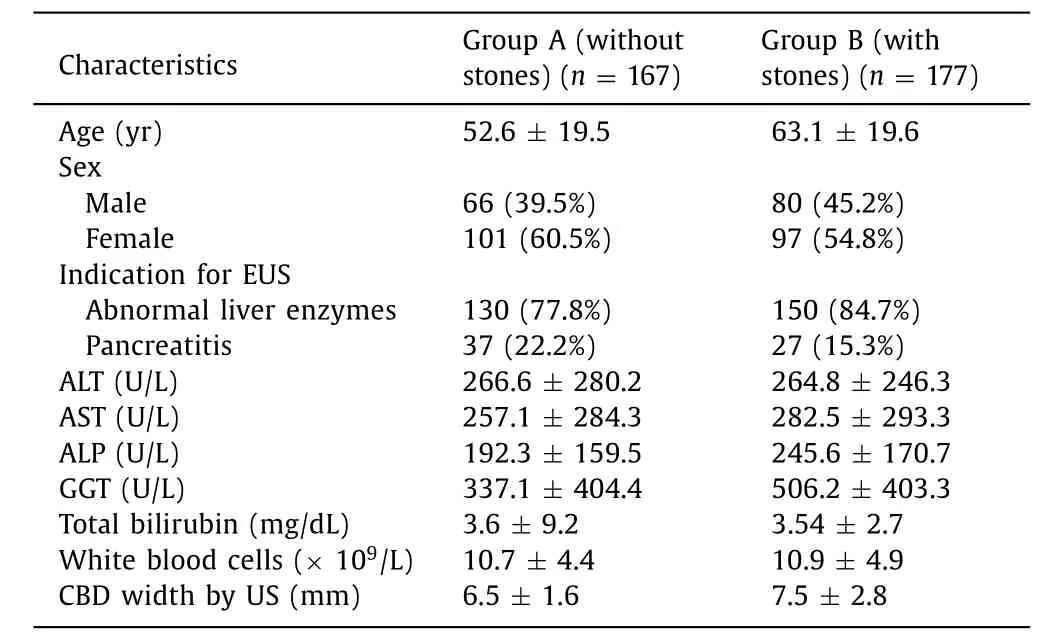
Table 1 Demographics, clinical and laboratory characteristics of study cohort.
Results
Baselinedemographics,clinicalandlaboratorycharacteristics
A total of 344 patients referred to EUS for suspected CBD stone were included in the study. One-hundred and sixty-seven patients without CBD stone according to EUS (group A) were compared to 177 patients with CBD stones (group B). The mean age in groups A and B was 52.6 ±19.5 years and 63.1 ±19.6 years, respectively. One hundred and one patients in group A and 97 in group B were female. The most common clinical presentation was abnormal cholestatic liver enzymes that was found in 116 patients(69.5%) in group A vs. 136 patients (76.8%) in group B. Hepatocellular liver enzymes (ALT and AST) were not different among the two groups. Clinical and laboratory characteristics are shown in Table 1 .
ClinicalandlaboratoryfactorsassociatedwithCBDstonesdiagnosis onunivariateanalysis
We identified several predictors for CBD stone as confirmed by EUS. Age ( OR = 1.027,P<0.0 0 01), ALP (OR = 1.002,P= 0.005),GGT (OR = 1.001,P<0.001) and CBD width by US (OR = 1.245,P<0.001) were statistically significant in a univariate model analysis. On the other hand, TBil level (P= 0.931), hepatocellular liver enzymes [ALT (P= 0.949) and AST (P= 0.414)] and sex (P= 0.290)were not associated with CBD stone ( Table 2 ). In multivariate regression analysis, CBD width by US (OR = 1.224,P= 0.0026), age(OR = 1.023,P= 0.0 0 02) and GGT level (OR = 1.001,P= 0.0018)were significantly correlated with CBD stone, with ROC of 0.7259( Fig. 1 ).
Modelbuildingofdiagnosticscore
To generate a diagnostic score, we assigned weights for each continuous variable that was shown to be statistically significant in the multiple logistic regression analysis, according to rounded coefficient estimates ( Table 3 ). We generated a diagnostic equation[age (yr) ×0.1 + CBD width (mm) by US ×1 + GGT (U/L) ×0.005]that aimed to define several cut-off points according to the values of age, GGT level of CBD width by US, inserted into the equation with their corresponding sensitivity, specificity, PPV and NPV. The ROC curve for this diagnostic model is 0.7287 (OR = 1.244, 95%CI: 1.155-1.338;P<0.001, likelihood ratio = 43.785) ( Fig. 2 ). The Youden J index for this equation is 13.57 that is associated with sensitivity of 81.7%, specificity of 57.6%, PPV of 66.8% and NPV of 75.0%. Table 4 demonstrates the equation cut-off points with their corresponding diagnostic statistics. For example, score that ranges from 17.6 to 26.7 has very high specificity (90.0% −99.3%) for CBD stones, as those patients might be referred directly to ERCP. On the other hand, cut-off point less than 11.4 has very low specificity of up to 28.0%, as those patients might be followed up without further endoscopic intervention.

Table 2 Univariate analysis of parameters associated with CBD stone.
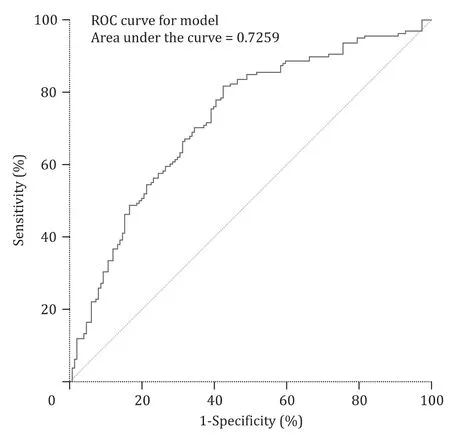
Fig. 1. ROC curve analysis for age, GGT level and dilated CBD on multivariate regression analysis.
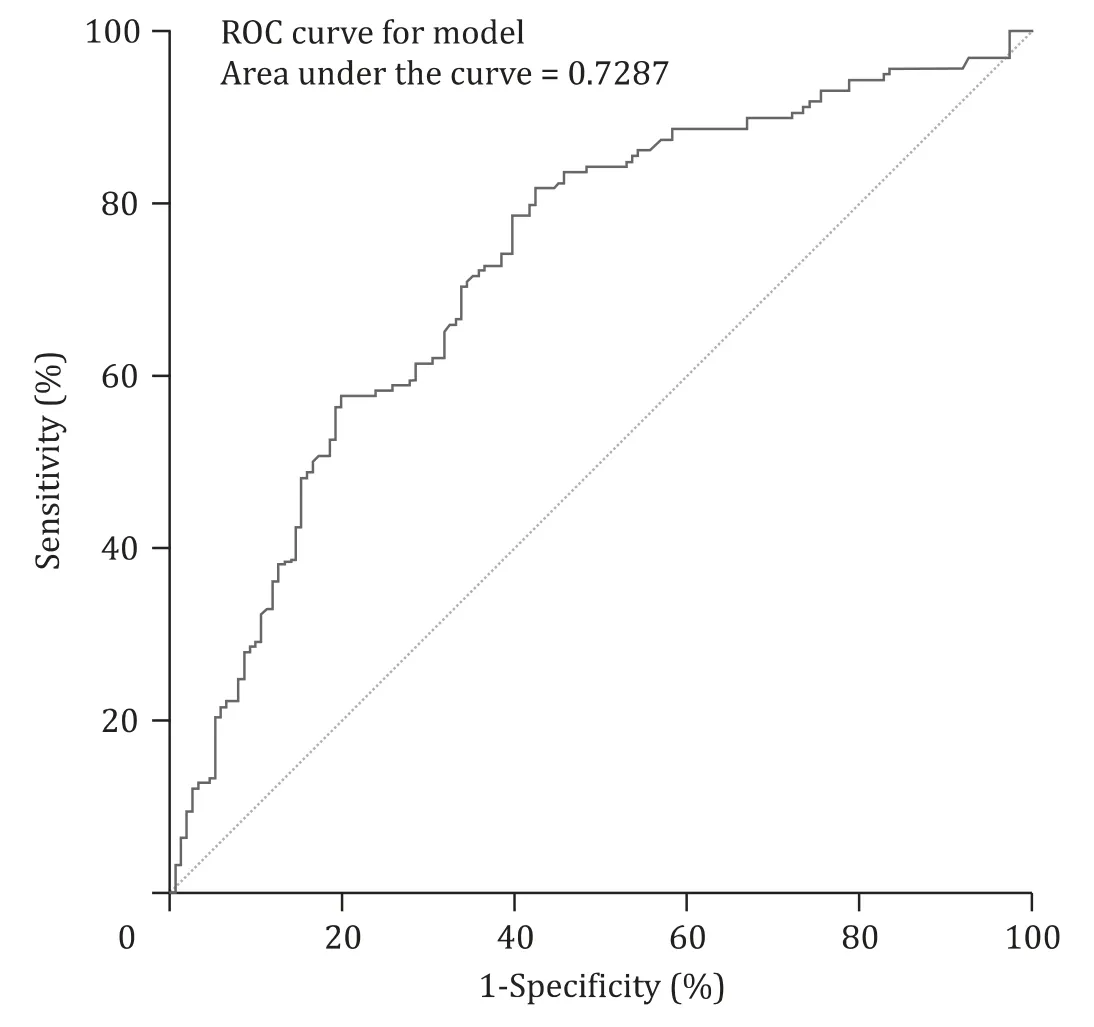
Fig. 2. ROC curve analysis of the score generated [age (yr) ×0.1 + CBD width (mm)by US ×1 + GGT (U/L) ×0.005].

Table 4 Equation generated cut-off points with their corresponding diagnostic statistics [age(yr) ×0.1 + CBD width (mm) by US ×1 + GGT (U/L) ×0.005].
TheperformanceoftheASGEcriteriaonourcohort
The ASGE published guideline for the management of suspected CBD stone [14] . According to this guideline, very strong predictors [CBD stone on transabdominal ultrasonography (US), clinical ascending cholangitis or TBil>4 mg/dL] and strong predictors (dilated CBD>6 mm on US with and TBil level of 1.8-4.0 mg/dL) indicate more than 50% probability for CBD stone and those patient are recommended to be transferred immediately for ERCP. In our cohort, we excluded patients with diagnosed CBD stone on US and patients with ascending cholangitis since those patients were referred immediately for ERCP. Implementing these guidelines in our cohort, we found out that TBil level of>4 mg/dL (a very strong predictor) has a sensitivity of 31.6%, specificity of 80.8%, PPV of 63.6%, NPV of 52.7% and accuracy of 55.5% for CBD stones. While by application of the strong predictors, we found that dilated CBD>6 mm on US and TBil level of 1.8-4.0 mg/dL has a sensitivity of9.6%, specificity of 95.2%, PPV of 6 8.0%, NPV of 4 9.8% and accuracy of 51.2% for CBD stone. Comparing our new prediction formula to the stratification criteria of the ASGE guidelines, we reached a higher specificity for CBD stone with the higher values.
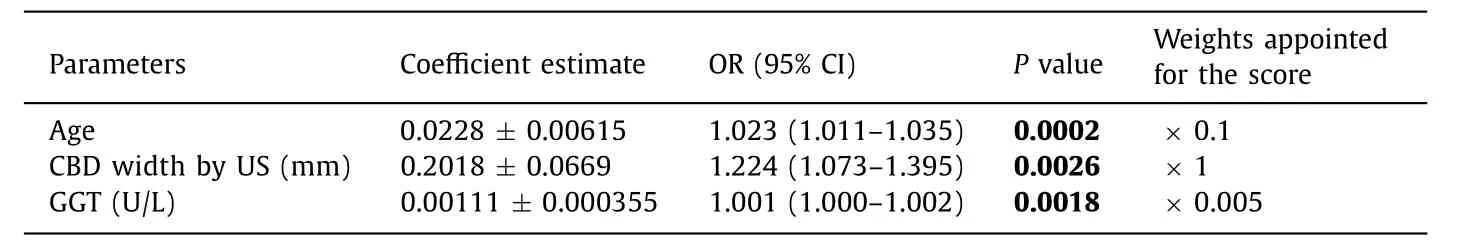
Table 3 Variables that were independently associated with CBD stones and their corresponding weight points given.
Discussion
The ASGE stratification criteria for the prediction of CBD stone are a working tool for the practitioners. However, their performance in cases other than cholangitis is less than optimal and lacks accuracy. Patients are categorized into low (10%), intermediate (10% −50%) and high (>50%) probability choledocholithiasis [17] .
In an attempt to achieve a more reasonable and safer approach to patients suspected to suffer from CBD stone, and in conjunction with our clinical practice and in accordance with results from recent studies [17 , 18] , we retrospectively evaluated the performance of different parameters in the prediction of CBD stone in our population including the parameters of the ASGE criteria.
Our first major finding was that age, GGT elevation and CBD width by US were the only parameters with clearly strong performance in predicting CBD stone as demonstrated by multivariate regression analysis. By generating a diagnostic equation [age(yr) ×0.1 + CBD width (mm) by US ×1 + GGT (U/L) ×0.005],the ROC curve for this diagnostic model is 0.7287 (OR = 1.244, 95%CI: 1.155-1.338;P<0.001, likelihood ratio 43.785), which is similar to the ROC obtained in the multivariate analysis. According to this equation, a score that ranges from 17.6 to 26.7 has very high specificity (90.0% −99.3%) for CBD stone, which is considered a very strong predictor according to the likelihood probabilities of the ASGE criteria, and can be a useful aid in stratifying these patients to ERCP. On the other hand, a score less than 11.4 has a very low specificity of up to 28.0%, and these patients might be followed up without further endoscopic intervention. Scores greater than 11.5 to 17.5 have a specificity ranging from 33.0% −89.5% and these patients may benefit from investigations like EUS or MRCP before therapeutic decision making.
It is well known that age plays a significant role in predicting CBD stone and the prevalence of gallstones increases with age [3] .As expected, gallstone diseases including CBD stone prevalence also increases with age. Patients’ age was identified as an essential determinant of increased risk of CBD stones [3 , 19] . The prevalence of CBD stone was shown to increase from 14% in patients less than 70 years old, to 32% in patients over 70 years old in a group of patients referred for EUS to rule out CBD stone [4] .
In accordance with our study, Nárvaez Rivera et al. [20] showed that among the strong predictors adopted by the ASGE, only CBD width above 6 mm showed a statistical significance between patients with and without CBD stone. Moreover, in different studies evaluating the performance of different noninvasive tests in the prediction of CBD stone, GGT was the most powerful predictor [21 , 22] . GGT also had the highest NPV for CBD stone [21] . The same study by Prat et al. [4] showed that the independent predictive variables for the presence of CBD stone in patients younger than 70 years were increased GGT (>7 ×normal), pathologic gallbladder and abnormal CBD (dilated or with intraluminal hyperechoic image), and in patients older than 70 years were increased GGT, fever and abnormal CBD.
The second major finding is that TBil did not show statistical significance in predicting CBD stone leading to the conclusion that it could not be a reliable parameter because it may lead to gratuitous ERCP. These results are in contrast to the ASGE guidelines from 2010; in which TBil is considered a strong or very strong predictor according to its values [14] .
In other prospective study, Sethi et al. [23] found no correlation between bilirubin value above 4 mg/dL and risk for CBD stone.Elevated bilirubin also did not show statistical significant difference between patients with and without CBD stone [20] . A recent study by Suarez et al. [18] showed that only 57% of patients who had TBil>4 mg/dL were found to have CBD stone while 37% of patients who had TBil ≤4 mg/dL did have stones in EUS, MRCP,ERCP or intra-operative cholangiography. Another study by Adams et al. [17] found only 56% of patients with TBil>4 mg/dL and 38% of patients with TBil<4 mg/dL have CBD stone or sludge in the above mentioned modalities. Both studies reach the conclusion that the existing guidelines lack accuracy.
Another important major finding is that the other biochemical liver tests cannot be relied on as predictors, including ALP which showed significance in univariate analysis but lost its significance in multivariate analysis, and both transaminases (AST and ALT)which showed no significance in univariate analysis as CBD stone predictors leading us to conclude that they have a minor role if ever, as predictors. Evaluating different biochemical predictors for CBD stone, Yang et al. [21] showed by multivariate analysis that the transaminases had no power to predict CBD stone. Interestingly, patients known to suffer from gallbladder stones presenting to the emergency room with symptomatic cholelithiasis can be stratified on place, using our bedside equation with more than 90%specificity for CBD stone if a score is more than 17.6, and these patients should be advanced to therapeutic ERCP. This finding is very important because life expectancy is increasing; the prevalence of cholelithiasis increases with age, and more elderly patients are being referred to hospital because of gallstones diseases. This equation can obviate the unnecessary investigations like EUS especially in the elderly high-risk patients in cases the score exceeds 17.6.
The limitations of our study are that we chose the maximal values of the laboratory tests obtained before EUS without considering laboratory trends over time. Although these trends may have impact on the performance of the above-mentioned criteria, a recent study by Adams et al. [17] concluded that laboratory trends did not improve the performance of the ASGE stratification criteria. The second limitation was considering the CBD width to be identical among patients with gallbladderinsituand patient after cholecystectomy despite the belief that the CBD width is increased after cholecystectomy. We did not discriminate between the two groups because there is no firm data regarding the accurate width after cholecystectomy. The last limitation is that we did not validate our findings in an independent validation cohort.
In conclusion, our study showed that revising the ASGE criteria could result in reduction of unnecessary ERCP in treating patients with high probability of CBD stone. Thus, we suggest the addition of the above-mentioned equation of age, CBD width and GGT value to the criteria. This addition means to upgrade the strength of these predictors which could augment the CBD stone predictors. To make it clear, among the different liver enzymes, only GGT showed statistical significance in CBD stone prediction, and therefore, we suggest revising the other liver biochemical tests significance as a predictor in the ASGE criteria. Also, we suggest downgrading the strength of bilirubin value as a strong predictor of CBD stone due to its low sensitivity and its potential to lead to unnecessary ERCP.
CRediT authorship contribution statement
Anas Kadah:Conceptualization, Data curation, Formal analysis,Writing - original draft.Tawfik Khoury:Conceptualization, Data curation, Formal analysis, Writing - review & editing.Mahmud Mahamid:Data curation, Formal analysis.Nimer Assy:Data curation, Formal analysis.Wisam Sbeit:Data curation, Formal analysis,Writing - review & editing.
Funding
None.
Ethical approval
The study protocol conforms to the ethical guidelines of the1975DeclarationofHelsinkiand was approved by the Institution Human Research Committee (0115-16-NHR). Written informed consent was waived by the local Ethical Committee due to the retrospective non-interventional nature of the study.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Transjugular intrahepatic portosystemic shunt for a patient with chylothorax in cryptogenic/metabolic cirrhosis
- Differential methylation landscape of pancreatic ductal adenocarcinoma and its precancerous lesions
- Hepatobiliary&Pancreatic Diseases International
- MicroRNAs and long non-coding RNAs in liver surgery: Diagnostic and therapeutic merits
- Alpha-fetoprotein and 18 F-FDG standard uptake value predict tumor recurrence after liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis: Preliminary experience
- Translationally controlled tumor protein exerts a proinflammatory role in acute rejection after liver transplantation