Sequential transcatheter arterial chemoembolization and portal vein embolization before right hemihepatectomy in patients with hepatocellular carcinoma
2020-07-07GilChunPrkSungGyuLeeYoungInYoonKyuBoSungGiYoungKoDongIlGwonDongHwnJungYongKyuJung
Gil Chun Prk Sung Gyu Lee Young In Yoon Kyu Bo Sung Gi Young Ko Dong Il Gwon Dong Hwn Jung Yong Kyu Jung
a Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul,Korea
b Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
Keywords:Sequential selective transcatheter Arterial chemoembolization Portal vein embolization Hepatocellular carcinoma Future liver remnant
A B S T R A C T Background: Recent studies showed that sequential selective transcatheter arterial chemoembolization(TACE) and portal vein embolization (PVE) provided better future liver remnant (FLR) regeneration rate and disease-free survival following surgery compared with PVE alone. The present study aimed to clarify whether preoperative sequential TACE and PVE before right hemihepatectomy can reduce postoperative hepatocellular carcinoma (HCC) recurrence and improve long-term disease-free and overall survival.Methods: Recurrence and survival outcomes were retrospectively evaluated in 205 patients with HCC who underwent right hemihepatectomy by a single surgeon from November 1993 to November 2017. Patients were divided into four groups according to the procedure performed before the surgery: sequential TACE and PVE (TACE-PVE), PVE-only, TACE-only, or naïve control groups. The baseline patient and tumor characteristics, postoperative outcomes, recurrence-free survival and overall survival were analyzed.Results: Baseline patient and tumor characteristics upon diagnosis were similar in all four groups, while sequential TACE and PVE were well tolerated. The TACE-PVE group had a higher mean increase in percentage FLR volume compared with that of the PVE-only group (17.46% ±6.63% vs. 12.14% ±5.93%;P = 0.001). The TACE-PVE group had significantly better overall and disease-free survival rates compared with the other groups (both P < 0.001).Conclusions: Sequential TACE and PVE prior to surgery can be an effective therapeutic strategy for patients with HCC scheduled for major hepatic resection. The active application of preoperative sequential TACE and PVE for HCC would allow more patients with marginal FLR volume to become candidates for major hepatic resection by promoting compensatory FLR hypertrophy without the deterioration of basal hepatic functional reserve or tumor progression.
Introduction
Global statistics show that hepatocellular carcinoma (HCC)is the most frequently occurring primary liver cancer and the fourth most frequent cause of cancer-related death worldwide [1] .Although surgical resection and transplantation remain the cornerstone of therapy for early-stage HCC in chronic diseases,locoregional and systemic therapies have been beneficial for those with more advanced diseases or those who are not candidates for surgery [2] . Locoregional therapy has been proposed as a potential form of neoadjuvant therapy prior to liver resection for HCC. Transcatheter arterial chemoembolization (TACE), one of the most widely used locoregional therapies for HCC, has been performed as a preoperative neoadjuvant therapy for patients with resectable HCC in the hope of improving postoperative survival [2] . Preoperative TACE aims to reduce the size of associated microscopic lesions, as well as the primary nodule, thereby increasing resectability, preventing cancer cell dissemination during surgery, sterilizing undetected lesions, and ultimately improving survival rates [3-5] . TACE has sometimes been used prior to preoperative portal vein embolization (PVE) for major hepatectomy to prevent accelerated tumor growth from the buffering increase in ipsilateral hepatic arterial flow—a detrimental effect of PVE [6] .PVE can induce atrophy of the liver segments to be resected and hypertrophy of the future liver remnant (FLR) [7] . Sequential selective TACE and PVE has been introduced in an attempt to expand the indications for major hepatic resection and prevent postoperative liver failure. Previous studies have suggested that preoperative sequential selective TACE and PVE could increase FLR hypertrophy rates mainly by decreasing arterial flow to the liver, which already has no portal vein flow, and suppressing arterioportal shunts that may negatively affect regeneration [8-10] . In addition, this combined strategy has been speculated to have a strong and direct anticancer effect given its ability to induce HCC necrosis [9 , 11 , 12] .
Recent studies have demonstrated that sequential selective TACE and PVE promotes better FLR regeneration rates and diseasefree survival after surgery compared with PVE alone [8-13] . Therefore, the present study aimed to clarify whether sequential TACE and PVE before right hemihepatectomy can reduce postoperative HCC recurrence and improve long-term disease-free overall survival.
Methods
Patients
This retrospective analysis included patients with HCC who underwent right hemihepatectomy by a single experienced surgeon from November 1993 to November 2017. Patients were divided into four groups according to the procedure performed before the surgery: sequential TACE and PVE (TACE-PVE), PVE-only, TACE-only,or naïve control groups. All data related to TACE, PVE, surgical resection, preoperative status, pathology, and follow-up were obtained from patients’ medical and imaging records after approval from the Institutional Review Board of our institution (2019-0361).The requirement for informed consent was waived due to the retrospective nature of the study.
SelectioncriteriaforsequentialTACEandPVEbeforeright hemihepatectomy
The final decision to perform PVE was made only after careful evaluation of computed tomography (CT) volumetry. Theoretically,right PVE is indicated for patients with an estimated FLR of<40%in a cirrhotic liver who have no signs or symptoms of portal hypertension, such as ascites and gastro-esophageal varices by endoscopy. Some patients with significantly low platelet levels(i.e., below 10 0 0 0 0/μL) and splenomegaly were excluded from PVE. Sequential TACE and PVE before right hemihepatectomy were especially indicated for patients with (1) multiple right lobe lesions; (2) a solitary tumor located adjacent to the hilum; (3) a tumor with portal vein tumor thrombus on anterior or posterior portal vein; and (4) posterior segment tumors, provided that they are attached to the right hepatic vein.
SequentialTACEandPVE
TACE was performed before PVE. Conventional mesenteric arteriography was initially performed to assess patient anatomy, tumor burden, vascularity, and portal vein patency. Thereafter, the tip of the catheter was placed selectively into the right hepatic artery, after which 2 mg/kg body weight dose of cisplatin and an iodized oil emulsion (Lipiodol; Laboratoire Guerbet, Cedex, France) were injected under fluoroscopic control followed by embolization with absorbable gelatin-sponge particles (Gelfoam; Upjohn, Kalamazoo,Michigan, USA) until arterial flow stasis was achieved. PVE was subsequently performed once liver function test results had stabilized, usually 3-4 weeks after TACE. Details regarding the PVE procedure were similar to those described in previous studies [14 , 15] .For direct portal venography and PVE, percutaneous transhepatic or transsplenic portal vein access was used. If access was obtained via the transhepatic portal vein approach, puncture of the portal branch was either ipsilateral or contralateral according to the tumor location and size. In the case of advanced HCC, the portal vein was approached mainly by puncturing the left portal vein( Fig. 1 ). Embolization materials including coils, gel foams, liquid agents (i.e., polyvinyl acetate), and Amplatzer vascular plugs(AGA Medical, Golden Valley, MN) were used either alone or in combination depending on their availability and operator preference. All patients also underwent Doppler ultrasonography 1 day after embolization to evaluate the embolized portal venous branches and determine the patency of the nonembolized portal branch.
Preoperativeevaluationandsurgicalprocedure
HCC was diagnosed based on preoperative imaging, specifically,triphasic abdominal CT of the abdomen. Selected cases underwent magnetic resonance imaging (MRI) to detect additional intrahepatic lesions and 2-18F-fluoro-2-deoxy-d-glucose positron emission tomography to rule out extrahepatic metastasis. Preoperative assessments including blood analysis [complete blood count, chemistry, indocyanine green retention rate at 15 min (ICG-R15), and tumor markers: protein induced by vitamin K absence II (PIVKA-II)and/or alpha-fetoprotein (AFP)], Child-Pugh class and esophagogastroduodenoscopy were used for liver function assessment. Right hemihepatectomy was performed 4-8 weeks after PVE. All patients underwent liver resection by a single experienced hepatobiliary surgeon using the anterior approach for hilum division. Parenchymal transection was performed using either the Kelly clamp-crush technique or an ultrasound aspiration dissector (CUSA EXcelTM,USA) employing the Pringle maneuver at 15-min intervals with a rest period of 5 min between intervals during transection.
Computedtomographyvolumetry
Multidetector dynamic CT scanning was routinely performed before and 4-8 weeks after PVE to assess gross liver volume changes and tumor progression. All CT images were reconstructed as 3-mm thick sections and stored within a Picture Archiving and Communication System (Petavision; Asan Medical Center, Seoul,Korea) that enables image processing and various measurements,including volumetry. The total estimated liver and FLR volumes were determined, with the latter representing the volume of the left lobe and caudate. The middle hepatic vein and gallbladder were used as landmarks indicating the borders of the right and left lobes of the liver. The estimated percentage FLR volume was calculated as (left lobe volume ×100)/total liver volume.
PostoperativesurveillanceandtreatmentforHCCrecurrence
Follow-up ended on June 30, 2019. Postoperative follow-up,which included chest CT and either CT or MRI of the abdomen,was scheduled every 2 to 3 months for the first year and every 3-4 months thereafter. AFP and/or PIVKA-II were also measured together with imaging tests. Various treatment modalities were selected for tumor recurrence confined to the liver, including repeat hepatectomy, radiofrequency ablation, TACE, metastasectomy,sorafenib, or a combination of these methods. Details regarding the postoperative follow-up protocol have been presented in our previous study [16] .

Fig. 1. A: Pre-portal vein embolization computed tomography of a 51-year-old man with large hepatocellular carcinoma abutting the right portal vein. B: Right PVE via a contralateral approach in a patient with advanced hepatocellular carcinoma. Access to the left portal vein branch near the lumbrical portion was obtained. Prior to PVE,portal venography demonstrated fluent blood flow in the main portal vein and branches. C: Final portal venography demonstrated successful right PVE, with preserved blood flow to the left liver. PVE: portal vein embolization.
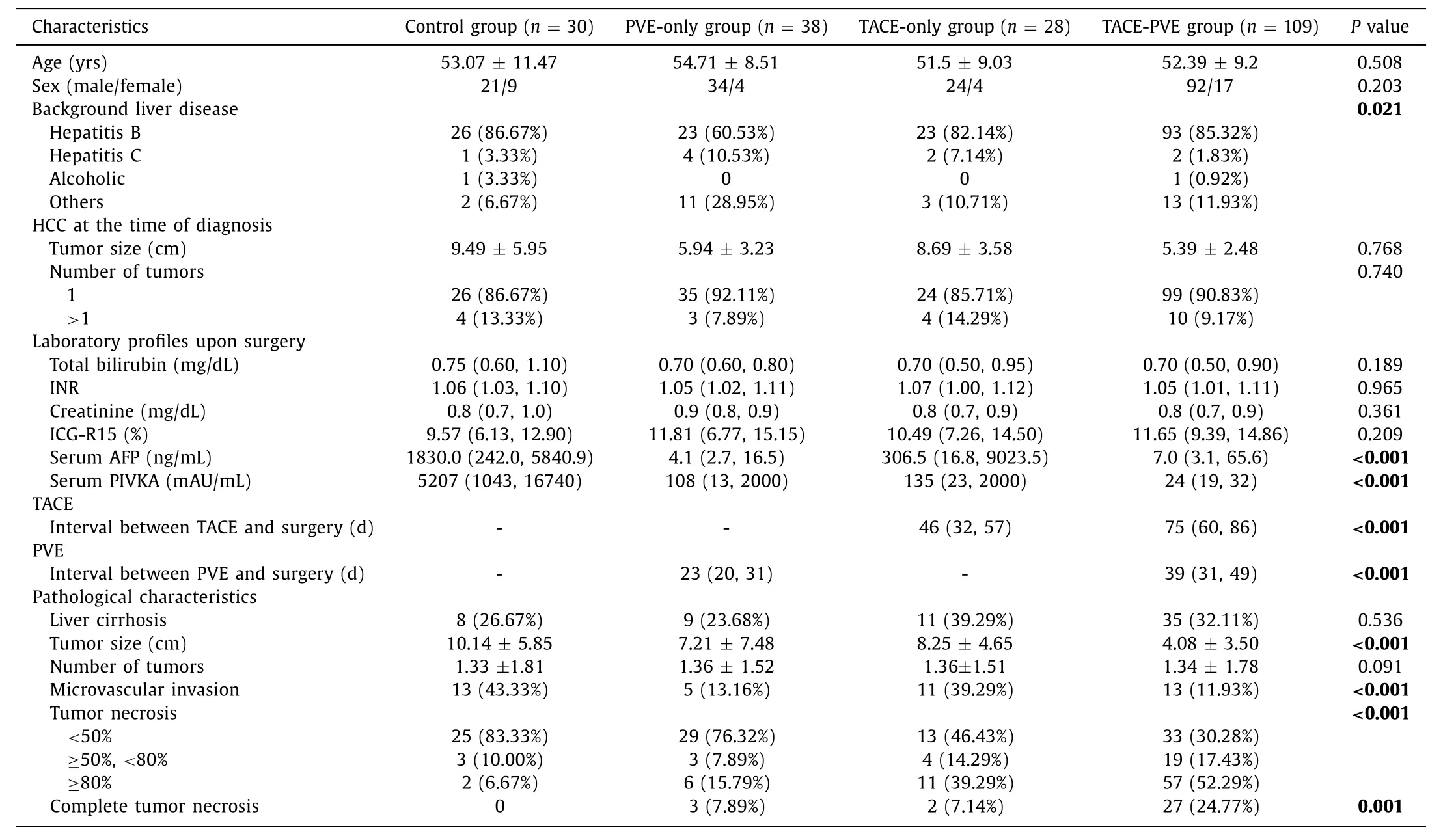
Table 1 Baseline patient characteristics.
Statisticalanalysis
Data were expressed as mean standard deviation or median(range) or number (percentage) as appropriate. Analysis of variance (ANOVA) or Kruskal-Wallis test was used to compare pairs of independent continuous variables, while the Chi-square test or Fisher’s exact test was used to compare categorical variables. Overall survival and recurrence-free survival were calculated using the Kaplan-Meier method and compared using the log-rank test. After the univariate analysis of the factors affecting survival, only the significant variables were used in the multivariate analysis using the Cox proportional hazard model. All statistical analyses were performed using SPSS (version 14.0, SPSS), with a two-sidedPvalue of<0.05 indicating statistical significance.
Results
Patientdemographics
Throughout the study period, 205 patients underwent right hemihepatectomy for HCC by a single surgeon. A comparison of the baseline patient and tumor characteristics in the TACE-only(n= 28), PVE-only (n= 38), TACE-PVE (n= 109), and control(n= 30) groups is presented in Table 1 . No significant difference in sex, age, tumor size and number upon diagnosis, and liver function test results before surgery was observed among the groups. Upon HCC diagnosis, the mean tumor diameters measured using imaging were 8.69, 5.94, 5.39, and 9.49 cm in the TACE-only, PVE-only,TACE-PVE, and control groups, respectively (P= 0.768).
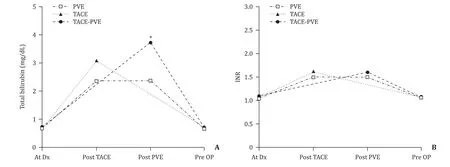
Fig. 2. Comparison of chronological alterations in serum total bilirubin ( A ) and international normalized ratio (INR) ( B ) between the three groups. ∗: P = 0.002, compared with the baseline. TACE: transcatheter arterial chemoembolization; PVE: portal vein embolization; Dx: diagnosis; OP: operation.
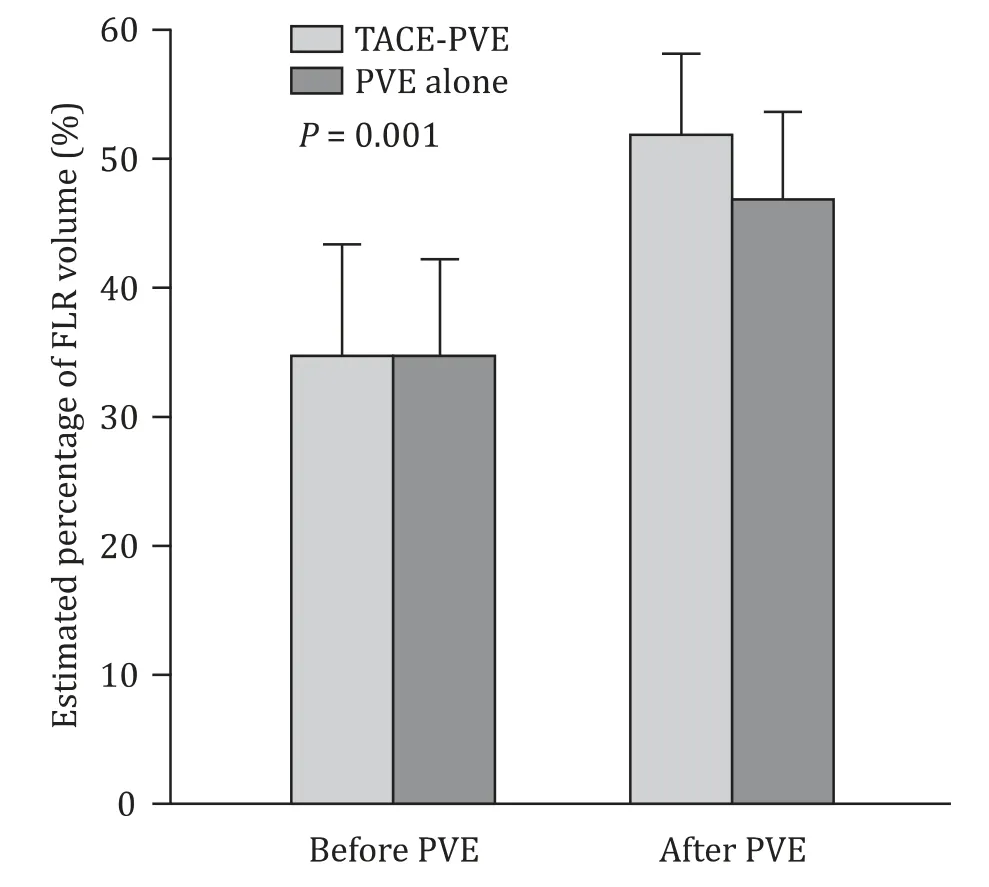
Fig. 3. Comparison of volumetric changes in the future remnant liver between the sequential transcatheter arterial chemoembolization (TACE) and portal vein embolization (PVE) group and PVE-only group. The TACE-PVE group had a significantly higher mean increase in percentage FLR volume than the PVE-only group(17.46% ±6.63% vs. 12.14% ±5.93%; P = 0.001)
ImpactofsequentialTACEandPVE
The TACE-PVE group had a longer median interval compared with the PVE-only group (39 vs 23 days,P<0.001). Liver function test results after sequential TACE and PVE showed peak total bilirubin levels and international normalized ratio (INR) that were significantly higher than baseline but returned to baseline before surgery ( Fig. 2 ). The TACE-PVE group had a significantly higher mean increase in percentage FLR volume than the PVE-only group(17.46% ±6.63% vs. 12.14% ±5.93%;P= 0.001) despite being similar before PVE ( Fig. 3 ).
The mean tumor diameters on pathological specimen were 8.25, 7.21, 4.08, and 10.14 cm in the TACE-only, PVE-only, TACEPVE, and control groups, respectively (P<0.001; Table 1 ), which was in contrast to those that did not exhibit significant differences in tumor size on preoperative imaging. The TACE-PVE group had a significantly higher median tumor necrosis rate (80.0%, range 30.0%-100%) than the TACE-only or PVE-only groups (P<0.001;Table 1 ). In addition, the proportion of patients who exhibited complete tumor necrosis was significantly larger in the TACE-PVE group (24.77%) than in the other groups (7.89%, 7.14%, and 0% for the PVE-only, TACE-only, TACE-PVE, and control groups, respectively;P= 0.001).
Postoperativemorbidityandmortality
The PVE-only, TACE-only, TACE-PVE, and control groups had a postoperative morbidity rate of 42.11%, 25.00%, 25.69%, and 20.00%,respectively (P= 0.162). As for developing major complications(Clavien-Dindo ≥IIIa), the PVE-only group had a higher risk (23.7%)than did the other three groups, albeit not significantly (P= 0.637).A significant difference was observed in the 90-day postoperative mortality rate among the four groups, with the PVE-only group having the highest mortality rate of 10.53% (P= 0.023; Table 2 ).Mortality in 4 patients in the PVE-only group occurred due to liver failure accompanied by sepsis, subdural hemorrhage, adult respiratory distress syndrome, and cardiogenic shock, respectively.
Tumorrecurrenceandoverallsurvivaloutcomes
From the follow-up period until the end of this study, 95 patients died, one was lost to follow-up, and 109 survived. The cumulative survival rates in the TACE-PVE group at 1, 3, 5, and 10 years were 94.5%, 85.7%, 75.6%, and 64.6%, respectively, significantly different from those in the other three groups (P<0.001) ( Fig. 4 A).In addition, the TACE-PVE group had a significantly higher cumulative recurrence-free survival rate than the other three groups(P<0.001). The TACE-PVE group had a 1-, 3-, 5-, and 10-year recurrence-free survival rates of 81.4%, 67.1%, 65.8%, and 60.0%, respectively ( Fig. 4 B). In addition, multivariate analysis confirmed that sequential TACE and PVE was significant and independent benefit factor associated with overall survival ( Table 3 ).
Discussion
Liver resection has been considered the first-line treatment for early-stage HCC among patients with well-preserved hepatic function given its acceptable mortality, morbidity, and long-term outcomes [17 , 18] . To achieve the best outcome with no postoperative in-hospital mortality and early recurrence for surgery in patients with HCC, perioperative strategies such as preoperative tumor downstaging, extended anatomical resection with lessmanipulation during surgery, and sufficient remnant liver volume after surgery are required. Although debatable, in theory, anatomical resection (i.e., tumor resection including tumor-bearing portal vein territories) has been regarded as an effective treatment to avoid intrahepatic metastasis and recurrence considering that HCC has a high tendency to invade intrahepatic vascular structures and spreads mainly through the portal venous system rather than through adjacent tumor diffusion [19-23] . However, anatomical resection, especially major liver resection, sacrifices a large amount of liver parenchyma with consideration of the Glisson’s pedicles and is therefore significantly unfavorable for treating livers with underlying chronic liver diseases. Although preoperative PVE in patients with chronic liver disease has broadened the indications for and safety of major hepatectomy, the degree of PVE-induced liver hypertrophy has been variable, with an insufficient or even absent hypertrophy being associated with unresectability or postoperative death after major hepatectomy [23-26] .Accordingly, additional strategies such as embolization of the ipsilateral hepatic artery and ipsilateral hepatic vein embolization have been proposed to induce FLR hypertrophy and achieve resectability among nonresponders to PVE [27-30] . Sequential TACE and PVE is also one of the proposed strategies in the same context.

Table 2 Perioperative results and postoperative complications.

Fig. 4. Comparison of overall survival rates ( A ) and disease-free survival rates ( B ) between the four groups. TACE: transcatheter arterial chemoembolization; PVE: portal vein embolization; OP: operation.
Although PVE has been the most commonly used strategy for increasing FLR, tumor progression while waiting for nonembolized liver segments to become hypertrophied has been an important issue. The rationale for sequential TACE and PVE is that the absence of arterial flow prevents tumor progression while waitingfor nonembolized liver segments to become hypertrophied. Indeed,the present study also demonstrated that the tumor size measured in the pathology specimen (7.21 ±7.48 cm) was larger than that in the image at the time of diagnosis (5.94 ±3.23 cm) in the PVE-only group, whereas the tumor size measured in the pathology specimen (4.08 ±3.50 cm) was smaller than that in the image at the time of diagnosis (5.39 ±2.48 cm) in the TACE-PVE group( Table 1 ). Moreover, previous studies have shown that this combined strategy provides a strong and direct anticancer effect, given its ability to induce HCC necrosis [9 , 11 , 12] . In fact, the present study showed that approximately 25% of the patients in the TACEPVE group achieved complete (100%) tumor necrosis, whereas only 7% of the patients in the PVE-only or TACE-only groups achieved the same. As an additional advantage, sequential TACE and PVE has been known to be more efficient than PVE alone in an increasing FLR volume among patients with chronic liver disease, possibly because TACE enhances the effects of PVE by suppressing any arterioportal shunts frequently observed in cirrhotic livers and HCC tumors [9 , 11-15] . Such an effect on the embolized liver could induce atrophy, resulting in an increased FLR volume.

Table 3 Univariate and multivariate analysis of risk factors for survival.
Until November 1993, we applied sequential TACE and PVE to patients with HCC with underlying cirrhosis for the first time worldwide [31] ; however, the application of this strategy to patients with cirrhosis has not been implemented as a risk concern and has been applied to patients with hilar cholangiocarcinoma after resolving jaundice through biliary drainage or colorectal cancer liver metastases in a normal liver. Based on theoretical background and practical experience associated with tumor progression with hypertrophy of the ipsilateral hepatic artery following PVE while awaiting the nonembolized liver segment to become hypertrophied, we now routinely perform TACE prior to PVE in patients with HCC requiring preoperative PVE.
One potential concern of sequential TACE and PVE has been potential damage of infarction or necrosis of the noncancerous liver parenchyma in the injured liver. However, the results obtained herein demonstrated very minimal injury of the noncancerous liver parenchyma among resected specimens, although a transient inflammatory reaction had occurred in the liver parenchyma considering the changes in blood tests after the procedure. Conversely, preoperative sequential TACE and PVE has the disadvantage of making the surgery technically difficult. First, care should be taken during hilar dissection to avoid dense inflammatory adhesion and choledochal varices around the right Glissonean pedicle following the sequential TACE and PVE. In addition, the use of intraoperative sonography is essential for finding the correct parenchymal resection line because the Cantlie’s line is distorted and deviated to the right side due to hypertrophy of the left lobe and atrophy of the right lobe.
While most of the patients underwent resection as planned,four patients who received sequential TACE and PVE did not undergo resection, achieving a resection rate higher than that reported in published studies. Surgery could not be performed in four patients because of the following three reasons: (1) failure to achieve adequate hypertrophy following PVE in one patient, (2) deterioration of liver function in one patient, and (3) complete tumor control via sequential TACE and PVE in two patients. Interestingly,none of the patients failed to achieve surgery due to tumor progression, whereas two patients acquired survival benefits without recurrence, given the direct anticancer effects of TACE and PVE.The reason for this high resection rate, as well as excellent outcomes, obtained herein could be attributed to our own PVE indication. While representative studies on the role of PVE before liver resection for HCCs had used FLR<40% in a cirrhotic liver as the indication for PVE, usually in combination with ICG-R15 (%) clearance [32-35] , the present study considered the severity of portal hypertension and FLR during the selection of patients for PVE.
Several limitations of the present study need to be considered.First, this was a retrospective data analysis study with all procedures performed by a single surgeon. Second, a relatively small number of patients had been included in our study. Finally, the study period of more than 24 years may have led to some historical bias considering the significant advances in perioperative assessment of underlying liver function and tumor extent, surgical techniques, and perioperative management that had occurred during that period. However, the protocols utilized by the aforementioned surgeon rarely changed throughout that period. Several strengths of the present study should also be highlighted. This has been the largest published series comparing long-term oncological outcomes after sequential TACE and PVE among patients who underwent right hemihepatectomy. A prospective randomized control trial will certainly be required to establish definite conclusions regarding the clinical efficacy of sequential TACE and PVE before surgery.
Over the past several decades, there have been debates regarding the effectiveness of sequential TACE and PVE before resection for improving surgical and oncological outcomes of HCC.The present study revealed that sequential TACE and PVE before scheduled right hemihepatectomy among patients with HCC can be safe and effective, even among those with chronic liver disease.Our results also showed that preoperative selective TACE and PVE might be associated with better overall and disease-free survival after right hepatectomy for HCC by effectively increasing FLR and inducing high complete tumor necrosis rates.
In conclusion, sequential TACE and PVE before major hepatic resection can be a valid therapeutic strategy among patients with HCC, even those with chronic liver injury. The active application of preoperative sequential TACE and PVE for HCC would allow more patients with marginal FLR volume to become candidates for major hepatic resection by promoting compensatory FLR hypertrophy without deterioration in basal hepatic functional reserve or tumor progression, through which better long-term survival can be achieved.
CRediT authorship contribution statement
Gil Chun Park:Writing - original draft.Sung Gyu Lee:Conceptualization, Writing - review & editing.Young In Yoon:Data curation, Writing - original draft.Kyu Bo Sung:Data curation, Investigation.Gi Young Ko:Data curation, Investigation.Dong Il Gwon:Data curation, Investigation.Dong Hwan Jung:Formal analysis.Yong Kyu Jung:Data curation.
Funding
None.
Ethical approval
This study was approved by the Institutional Review Board of Asan Medical Center, University of Ulsan College of Medicine(2019-0361).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Transjugular intrahepatic portosystemic shunt for a patient with chylothorax in cryptogenic/metabolic cirrhosis
- Differential methylation landscape of pancreatic ductal adenocarcinoma and its precancerous lesions
- Hepatobiliary&Pancreatic Diseases International
- MicroRNAs and long non-coding RNAs in liver surgery: Diagnostic and therapeutic merits
- Alpha-fetoprotein and 18 F-FDG standard uptake value predict tumor recurrence after liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis: Preliminary experience
- Translationally controlled tumor protein exerts a proinflammatory role in acute rejection after liver transplantation