局部进展期肾癌术前CRP/Alb比值对预后的价值
2020-07-04张大为张桂铭刘勇
张大为 张桂铭 刘勇
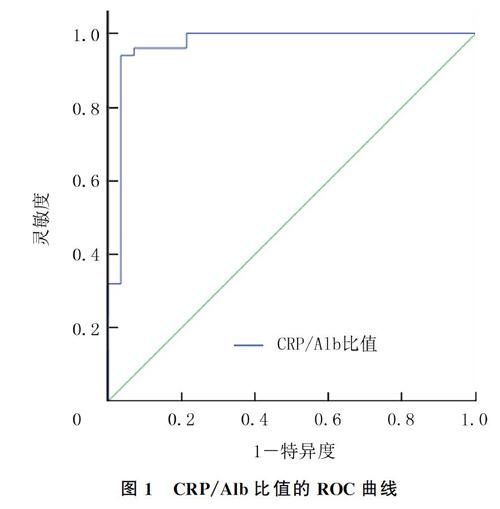

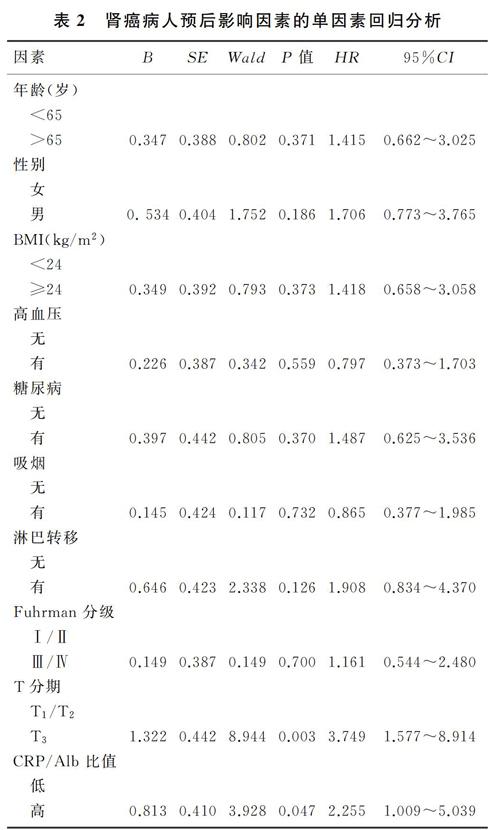
[摘要]目的 探討术前C-反应蛋白/清蛋白(CRP/Alb)的比值在预测局部进展期肾癌病人预后中的作用。方法 回顾性分析78例局部进展期肾癌病人的临床资料,所有病人病理类型均为透明细胞癌,根据受试者工作特征(ROC)曲线计算CRP/Alb最佳临界值,按最佳临界值将病人分为CRP/Alb高比值组和CRP/Alb低比值组,比较两组间临床病理特征的差异,并采用Kaplan-Meier生存分析、单变量和多变量Cox比例风险模型分析CRP/Alb比值预测肾癌病人预后的价值。结果 CRP/Alb比值与病人Fuhrman分级及T分期相关(χ2=6.159、11.496,P<0.05)。Kaplan-Meier生存分析显示,CRP/Alb高比值组总生存时间明显低于CRP/Alb低比值组(t=4.242,P<0.05)。单因素分析显示,肿瘤的T分期(P=0.003)、CRP/Alb比值(P=0.047)与预后相关;多因素回归分析显示,T分期(P=0.002)、CRP/Alb比值(P=0.026)与肾癌的总生存率相关,是独立的预后因素。结论 CRP/Alb比值升高是局部进展期肾癌病人总生存率的独立预后指标,可作为判断预后和术后辅助治疗的依据。
[关键词] 肾肿瘤;疾病恶化;C反应蛋白质;白蛋白类;预后
[中图分类号] R737.11[文献标志码] A[文章编号] 2096-5532(2020)04-0413-04
doi:10.11712/jms.2096-5532.2020.56.082
[网络出版] http://kns.cnki.net/kcms/detail/37.1517.R.20200417.0910.004.html;2020-04-17 17:14
VALUE OF PREOPERATIVE C-REACTIVE PROTEIN/ALBUMIN RATIO IN PREDICTING THE PROGNOSIS OF PATIENTS WITH LOCALLY ADVANCED RENAL CARCINOMA
ZHANG Dawei, ZHANG Guiming, LIU Yong
(Department of Urology, Affiliated Hospital of Qingdao University, Qingdao 266003, China)
[ABSTRACT]Objective To investigate the value of preoperative C-reactive protein/albumin (CRP/Alb) ratio in predicting the prognosis of patients with locally advanced renal carcinoma.Methods A retrospective analysis was performed for the clinical data of 78 patients with local advanced renal carcinoma, and all patients had a pathological type of clear cell carcinoma. According to the optimal cut-off value of CRP/Alb ratio calculated by the receiver operating characteristic (ROC) curve, the patients were divided into high CRP/Alb group and low CRP/Alb group, and clinicopathological features were compared between the two groups. Kaplan-Meier survival analysis and univariate and multivariate Cox proportional hazards model analyses were performed to investigate the value of CRP/Alb ratio in predicting the prognosis of patients with renal carcinoma. Results CRP/Alb ratio was correlated with Fuhrman grade and T stage (χ2=6.159,11.496;P<0.05). The Kaplan-Meier survival analysis showed that the high CRP/Alb group had a significantly shorter overall survival time than the low CRP/Alb group (t=4.242,P<0.05). The univariate analysis showed that tumor T stage (P=0.003) and CRP/Alb ratio (P=0.047) were associated with prognosis, and the multiva-riate regression analysis showed that T stage (P=0.002) and CRP/Alb ratio (P=0.026) were correlated with the overall survival rate of renal carcinoma and were independent prognostic factors.Conclusion Elevated CRP/Alb ratio is an independent prognostic indicator for overall survival rate in patients with locally advanced renal carcinoma and can thus be used as a basis for prognosis prediction and postoperative adjuvant therapy.
[KEY WORDS] kidney neoplasms; disease progression; C-reactive protein; albumins; prognosis
肾癌是泌尿系肿瘤中最常见的恶性肿瘤之一,其占全身恶性肿瘤的2%~3%[1]。由于健康查体的普及和影像学技术的广泛应用,尤其是腹部超声和CT检查,使得肾脏肿瘤的检出增加[2]。局限性肾癌病人通常接受治疗性全肾或部分肾切除术,高达40%的病人肿瘤最终会在远处复发[3-4]。此外,大约1/3的肾癌病人在初诊时即已出现转移。尽管采用了分子靶向治疗,但肾癌病人5年总生存率很少超过10%[5-6]。即使是肿瘤分期、分级等临床病理参数相似的局部进展期肾细胞癌的临床病程也难以预测[7-8]。因此,明确预后因素对指导手术后病人管理具有重要意义。越来越多的研究结果表明,炎症指标C-反应蛋白(CRP)在多种癌症,包括肾癌中
均有预后评估的作用[9-10]。也有研究表明,术前营养状况如低清蛋白(Alb)血症与肾癌根治性或部分切除术后预后较差有关[11-12];术前CRP/Alb比值为肝癌、胃癌和小细胞肺癌的独立预后标志物[13-15]。目前,CRP/Alb比值在肾癌中的作用研究较少[16],尤其在局部进展期肾癌预后中的作用未有报道。本文探讨CRP/Alb比值在局部进展期肾癌病人中的预后价值,为其术前治疗提供理论依据。
1 对象与方法
1.1 一般资料
收集2008—2017年我院收治、行肾癌根治性切除术的局部进展期肾癌病人的临床资料,并进行回顾性研究。病人入选标准:①经细胞学或组织学诊断为肾透明细胞癌;②有全血实验室检测数据,包括根治性切除术前1周内血清CRP和Alb;③术前影像学或术后病理学检查证实为局部进展期肾癌,2010年AJCC临床分期为Ⅲ期,其中包括T1N1M0、T2N1M0、T3N0M0、T3N1M0。排除标准:①手术切除前没有血液标本实验室检测结果的病人;②活动性炎症病人和其他恶性肿瘤病人。最终纳入符合标准病人78例,均有临床和病理资料,包括手术时年龄、性别、体质量指数(BMI)、高血压、糖尿病、吸烟、T分期、淋巴结转移以及Fuhrman 分级等。所有血标本均在首次治疗前1周内采集。
1.2 病人随访
手术后2年内每3个月、2~5年每6个月、5年后每1年进行1次CT检查。最后1次随访日期为2018年11月1日。总生存率(OS)从手术日期到死亡日期或最后1次随访计算。
1.3 统计学分析
应用SPSS 21.0软件进行统计学处理。采用χ2检验比较不同CRP/Alb比值组的临床病理特征之间的差异。通过受试者工作特征(ROC)曲线,结合灵敏度和特异度的结果,将曲线上Youden指数最大的切点作为确定炎症因子水平的最佳分界点,计算曲线下面积(AUC)。采用Kaplan-Meier法进行生存分析和曲线绘制,使用对数秩检验比较不同CRP/Alb比值组的差异。应用Cox比例风险模型分析单变量分析中具有显著意义的变量,变量与其他变量显著相关,则将其排除在最终的多变量分析之外,多变量分析计算95%置信区间(95%CI)的危险比(HR)。以P<0.05为差异有统计学意义。
2 结果
2.1 CRP/Alb比值与临床病理特征的相关性
根据ROC曲线计算得出CRP/Alb比值的最佳临界值为0.080(图1)。按最佳临界值将病人分为高比值组(CRP/Alb比值≥0.080)与低比值组(CRP/Alb比值<0.080),两组比较,Fuhrman分级、T分期差异有显著性(χ2=6.159、11.496,P<0.05),年龄、性别、BMI、高血压、糖尿病、吸烟、淋巴结转移等差异无显著性(P>0.05)。见表1。
2.2 肾癌病人预后影响因素单因素和多因素分析
单因素分析显示,肿瘤的T分期(P=0.003)、CRP/Alb比值(P=0.047)与预后相关;多因素分析结果显示,CRP/Alb比值(P=0.026)、T分期(P=0.002)與局部进展期肾癌的OS相关,是局部进展期肾癌病人的独立预后因素。见表2、3。
2.3 不同CRP/Alb比值组总生存期比较
Kaplan-Meier生存分析显示,CRP/Alb高比值组总生存期为(65.020±4.021)月,明显低于CRP/Alb低比值组的(74.683±3.532)月,差异有统计学意义(t=4.242,P<0.05)。见图2。
3 讨论
已有研究表明,全身免疫应答机制在肿瘤侵犯和进展中发挥了重要的作用[17]。在相关的炎症反应预后指标中,CRP在多种癌症包括肾癌中均已被证实是有效的系统性炎症评分指标[18]。还有研究表明,CRP是多种原发性恶性肿瘤炎症相关的预后指标[19-20]。其机制可能为:①肿瘤生长引起的周围组织炎症可能导致CRP水平升高[21];②CRP可能是机体免疫系统对肿瘤抗原反应的一种指示性标志物[22];③肿瘤伴随着炎症性细胞因子的释放和炎症微环境的形成,炎症细胞又促进了肿瘤的发展[23]。有研究指出,在恶性肿瘤病人体内血清CRP水平均有不同程度的增高,局部进展期肾癌病人血清CRP水平明显高于正常人群,CRP水平升高与肿瘤病人的预后较差有关,与肿瘤进展存在相关性[13,24]。低Alb水平是一种机体营养状态不良的表现,有研究表明Alb水平与不同肿瘤(如肺癌、胃癌和结肠癌)病人的预后相关,可导致肿瘤病人生存期缩短和肿瘤进展[24],故CRP/Alb比值可以预测肿瘤病人的生存期[13]。本文研究结果也表明,CRP/Alb比值升高与局部进展期肾癌病人OS较低有关,是一种潜在的肿瘤反应和预后的标志物。
本研究单因素分析结果显示,局部进展期肾癌病人CRP/Alb比值越高,预后越差;多因素分析表明,CRP/Alb比值是局部进展期肾癌病人的独立预后因素,可以独立预测局部进展期肾癌病人的术后生存;CRP/Alb高比值组的OS明显低于CRP/Alb低比值组,差异有显著性。提示CRP/Alb比值与局部进展期肾癌病人的生存期有关,高CRP/Alb比值建立在血清高CRP和低Alb水平的基礎上。以上结果表明,CRP/Alb比值作为系统性炎症评分指标,在预测局部进展期肾癌病人预后方面有明显作用。在后续研究中需扩大样本量继续深入分析。
本文研究结果提示术前抗炎治疗以及补充营养可能会使病人受益。首先,根据术前CRP/Alb比值可以选择高危病人进行进一步的管理和治疗;其次,本文结果可以用于未来临床试验中更有可能对生物标志物富集策略做出反应的病人进行分层;第三,术前使用CRP/Alb比值评估可能为确定哪些病人更有可能从治疗中获益提供有效信息。
综上所述,CRP/Alb比值与局部进展期肾癌病人的生存期有关,是局部进展期肾癌病人的独立预后因素,高CRP/Alb比值预示着预后较差。局部进展期肾癌病人术前降低CRP/Alb比值可能延长术后生存时间。本文存在以下局限性:本研究为单中心回顾性研究,评估的病人数量较少,CRP/Alb比值的预测价值还需要进行多中心、大样本量前瞻性研究来进一步验证。此外,本文研究还包括了选择偏差和不可测量的混杂因素。
[参考文献]
[1]SIEGEL R L, MILLER K D, JEMAL A. Cancer statistics, 2015[J]. CA: A Cancer Journal for Clinicians, 2015,65(1):5-29.
[2]PALSDOTTIR H B, HARDARSON S, PETURSDOTTIR V, et al. Incidental detection of renal cell carcinoma is an independent prognostic marker: results of a long-term, whole po-pulation study[J]. The Journal of Urology, 2012,187(1):48-53.
[3]PARK Y H, BAIK K D, LEE Y J, et al. Late recurrence of renal cell carcinoma >5 years after surgery: clinicopathological characteristics and prognosis[J]. BJU International, 2012,110(11 Pt B): E553-E558.
[4]LJUNGBERG B, BENSALAH K, CANFIELD S, et al. EAU guidelines on renal cell carcinoma:2014 update[J]. European Urology, 2015,67(5):913-924.
[5]BATTAGLIA M, LUCARELLI G. The role of renal surgery in the era of targeted therapy: the urologists perspective[J]. Urologia, 2015,82(3):137-138.
[6]LEE Y R, LESTER R, HENG D Y. Current management and future perspectives of metastatic renal cell carcinoma[J]. International Journal of Urology: Official Journal of the Japanese Urological Association, 2014,21(9):847-855.
[7]BILLIA M, VOLPE A, TERRONE C. The current TNM staging system of renal cell carcinoma: are further improvements needed[J]? Archivos Espanoles de Urologia, 2011,64(10):929-937.
[8]HAYES D F, ALLEN J, COMPTON C, et al. Breaking a vicious cycle[J]. Science Translational Medicine, 2013,196(5):196cm6.
[9]TAI C G, JOHNSON T V, ABBASI A, et al. External validation of the modified Glasgow prognostic score for renal can-cer[J]. Indian Journal of Urology (IJU): Journal of the Urological Society of India, 2014,30(1):33-37.
[10]MATHIAS T M, SILVA J F, SAPATA V M, et al. Evaluation of the effects of periodontal treatment on levels of ascorbic acid in smokers[J]. Journal of the International Academy of Periodontology, 2014,16(4):109-114.
[11]MORGAN T M, TANG D, STRATTON K L, et al. Preope-rative nutritional status is an important predictor of survival in patients undergoing surgery for renal cell carcinoma[J]. European Urology, 2011,59(6):923-928.
[12]CHOI Y, PARK B, JEONG B C, et al. Body mass index and survival in patients with renal cell carcinoma: a clinical-based cohort and meta-analysis[J]. International Journal of Cancer, 2013,132(3):625-634.
[13]KINOSHITA A, ONODA H, IMAI N, et al. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma[J]. Annals of Surgical Oncology, 2015,22(3):803-810.
[14]LIU Xuechao, SUN Xiaowei, LIU Jianjun, et al. Preoperative C-reactive protein/albumin ratio predicts prognosis of patients after curative resection for gastric cancer[J]. Translational Oncology, 2015,8(4):339-345.
[15]ZHOU Ting, ZHAN Jianhua, HONG Shaodong, et al. Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer[J]. Scientific Reports, 2015,5(6):10481.
[16]CHEN Zhen, SHAO Yingjie, FAN Min, et al. Prognostic significance of preoperative C-reactive protein: albumin ratio in patients with clear cell renal cell carcinoma[J]. International Journal of Clinical and Experimental Pathology, 2015,8(11):14893-14900.
[17]MANTOVANI A, ALLAVENA P, SICA A, et al. Cancer-related inflammation[J]. Nature, 2008,454:436-444.
[18]CHANG Y, AN H, XU L, et al. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma[J]. British Journal of Cancer, 2015,113(4):626-633.
[19]ISHINO Y, SAIGUSA S, OHI M, et al. Preoperative C-reactive protein and operative blood loss predict poor prognosis in patients with gastric cancer after laparoscopy-assisted gastrectomy[J]. Asian Journal of Endoscopic Surgery, 2014,7(4):287-294.
[20]INOUE Y, IWATA T, OKUGAWA Y, et al. Prognostic significance of a systemic inflammatory response in patients undergoing multimodality therapy for advanced colorectal cancer[J]. Oncology, 2013,84(2):1-7.
[21]MROCZKO B, GROBLEWSKA M, GRYKO M, et al. Diagnostic usefulness of serum interleukin 6 (IL-6) and C-reactive protein (CRP) in the differentiation between pancreatic cancer and chronic pancreatitis[J]. Journal of Clinical Laboratory Analysis, 2010,24(4):256-261.
[22]BALKWILL F, MANTOVANI A. Inflammation and cancer: back to Virchow[J]. Lancet, 2001,357(9255):39-45.
[23]WISASTRA R, DEKKER F J. Inflammation, cancer and oxidative lipoxygenase activity are intimately linked[J]. Cancers (Basel), 2014,6(3):15-21.
[24]曲卓慧,王躍辉,张静静. 血清C反应蛋白与白蛋白比值对晚期结直肠癌患者预后的判断价值[J]. 中国实用医药, 2017,12(30):9-11.
(本文编辑 黄建乡)
