Clinical effect of preventive nursing on the rate of deep vein thrombosis in patients with lung cancer: A meta-analysis
2020-07-04MiaoGaoNaFengXiuPingZuoMeiXiaZhangPengBoZhangMengXu
Miao Gao, Na Feng✉, Xiu-Ping Zuo, Mei-Xia Zhang, Peng-Bo Zhang, Meng Xu
1. The First Affiliated Hospital of Air Force Medical University (XiJing Hospital), Respiratory and Critical Care Medicine, Xi’an, Shaanxi, 710032, China
2. The First Affiliated Hospital of Air Force Medical University (XiJing Hospital), Department of Nursing, Xi’an, Shaanxi, 710032, China
Keywords:Preventive nursing intervention Lung cancer The formation rate of deep vein thrombosis Meta-analysis
ABSTRACT Objective: To explore the clinical effect of preventive nursing intervention on deep venous thrombosis rate, nursing satisfaction and average hospitalization time after treatment of lung cancer. Methods: Chinese databases (Wanfang, Weipu and China Knowledge Network) and English databases (Pubmed, Cochrane and Scopus) were searched and read references for relevant research. Statistical analysis was performed using Review Manager 5.3. The odds ratio (OR) and the mean difference (MD) were used as the combined effect values of the comparison groups. Sensitivity analysis was performed by changing the effect model or excluding the literature with a large weight ratio, and the symmetry of the funnel plot was observed for publication bias test. Results: A total of 14 Chinese studies included. Compared with routine nursing intervention, preventive nursing intervention could significantly reduce the rate of deep vein thrombosis after lung cancer treatment [OR=0.16 (0.10, 0.23)], improve nursing satisfaction [OR=6.42 (3.32, 12.41)] and shorten the average hospital stay [MD=-7.41 (-8.16, - 6.65)], without heterogeneous existing. And regardless of whether the lung cancer patient was undergoing resection or chemotherapy, the effect of preventive nursing intervention to reduce the rate of deep vein thrombosis was very significant. Conclusion: Preventive nursing intervention is beneficial to patients with lung cancer, which can significantly reduce the formation rate of deep vein thrombosis, which is worthy of clinical promotion.✉Corresponding author: Na Feng.
1. Introduction
Lung cancer is the most common malignancy in China, and statistically, the new cases in 2014 have reached 0.78 million
[1] and its mortality during 2004-2010 accounted for 24.41% of all malignancy deaths [2]. Vein thrombosis (VT), a common complication with 4%-10% incidence in lung cancer, poses great menace to health [3]. The formation of VT is closely associated with lung cancer patients own hypercoagulability [4]. In addition, surgical resection or chemotherapy to lung cancer could cause body release a large amount of coagulant, further facilitating VT formation as well [5]. Therefore, the prevention of VT is of great importance to lung cancer, which puts forward higher requirements to the clinical nursing work. Many researches have explored the effect of the preventive nursing intervention on deep vein thrombosis (DVT) of lung cancer after surgery and chemotherapy, in order to reduce the DVT incidence by many measures such as health education, risk assessment, psychological care and targeted thrombolytic anticoagulant treatment. However, due to small samples and inconsistent conclusions and so on, the ability of the preventive nursing intervention to decrease DVT is still a highly debated issue. Thus, we conducted this study to make an evaluation systematically, expecting to provide evidence to clinical nursing work.
2. Materials and methods
2.1 Literature retrieval
To ensure a higher comprehensive searching, Meshes including “Lung Neoplasms”, “Venous Thrombosis” and “Nursing” were used to search English database(Pubmed, Cochrane and Scopus),and Chinese Meshes including “Fei Ai”, “Jing mai xue shuan” and “Hu li” were used to search Chinese database(Weipu, Wangfang and CNKI). The retrieval time is up to 2019.05. The retrieval style adopts the combination of Mesh and free words. Pubmed retrieval strategy is as follows: ((((care[Title/Abstract] OR Nursing[Title/Abstract])) OR "Nursing"[Mesh])) AND (((((Deep Vein Thrombosis[Title/Abstract] OR Phlebothrombosis[Title/Abstract] OR Phlebothromboses[Title/Abstract] OR Deep Vein Thrombosis[Title/Abstract] OR Vein Thrombosis[Title/Abstract])) OR "Venous Thrombosis"[Mesh])) AND ((((Pulmonary Neoplasms[Title/Abstract] OR lung cancer[Title/Abstract]))) OR "Lung Neoplasms"[Mesh])). Finally, references were also screened to include more eligible studies.
2.2 Inclusion and exclusion criteria
Inclusion criteria:(1) Diagnosis of lung cancer pathologically;(2) Preventive nursing intervention;(3) Conventional nursing in control group;(4) Main outcome is DVT rate;(5) Study design includes cohort study, case-control study or cross-sectional study. Exclusion criteria:(1) Not lung cancer ;(2) Other nursing measures, such as comprehensive care;(3)Not conventional nursing in control group;(4)Outcomes without DVT rate;(5) review or case report.
2.3 Data extraction and quality evaluation
The quality evaluation of data extraction and included literature was completed by two people independently, and in case of disagreement, discussion was conducted and third-party assistance was requested. Data extraction consists of the following items: first author, year of publication, country of origin, grouping method, number of study groups and control groups, etc. The quality assessment was scored with reference to the newcastle-ottawa scale (NOS), with scores ranging from 0 to 9 and ≥7 indicating high-quality articles.
2.4 Statistical analysis
Review Manager 5.3 was utilized to conduct Statistical analysis,and odds ratio (OR)and mean difference (MD) were used to calculate pooled effect values and their corresponding 95% confidence intervals (95%CI) between every comparison. Heterogeneity among studies was assessed by I2 statistic. I2> 50% indicated evidence of heterogeneity. If heterogeneity existed among the studies, the random effects model was used to estimate the pooled effect size. Otherwise, the fixed effects model was adopted. Subgroup analysis was conducted to explore the source of heterogeneity. Sensitivity analysis was performed by eliminating the studies with heavy weight and changing the effect model. The potential publication bias was investigated using funnel plot.
3. Results
3.1 Results of included literature
A preliminary search included 283 articles, 65 in English and 218 in Chinese. Duplicate and further read the titles and abstracts to exclude 191, leaving 27. Through reading the full text, we found that there were 4 studies on comprehensive nursing measures, 3 on palliative nursing measures, and 6 on outcome indicators that did not meet the requirements. There is no English literature reported about the effect of preventive care on deep vein thrombosis of posttreatment lung cancer,finally a total of 14 Chinese articles [6-19] were included. Among them, the publication years were nearly 4 years, mostly in 2018 and 2017. There were 11 studies [6-16] on subjects receiving surgical resection, 4 studies [7, 17-19] on subjects receiving chemotherapy, 3 studies [17-19] on patients receiving PICC catheter chemotherapy, and 2 studies [18-19] on elderly patients. Nine studies [6-7, 9-12, 14, 16,19] were randomized, while five studies [8, 13, 15, 17-18] were not randomized. The total number of patients receiving preventive nursing intervention was 622 in the experimental group and 624 in the control group. The primary outcome measures were the rate of deep vein thrombosis, and the secondary outcome measures were nursing satisfaction and mean hospital stay. NOS scores indicate Literature of high and low quality is evenly distributed. The basic characteristics of each included study are shown in table 1.

Table 1 Characteristics of included studies
3.2 Meta-analysis
3.2.1 Clinical effect of preventive nursing on the rate of deep vein thrombosis in patients with lung cancer post-treatment
A total of 14 studies [6-19] mentioned the incidence of deep vein thrombosis, and the results of meta-analysis are shown in figure 1. I2=0, P=1, so there was no heterogeneity among the studies, and the fixed model was adopted. The results of meta-analysis showed that compared with conventional nursing intervention, preventive nursing intervention significantly reduced the rate of deep vein thrombosis in lung cancer patients after treatment [OR=0.16(0.10,0.23)]. To explore more significance of clinical application, we conducted subgroup analysis, and the results are shown in table 2. Preventive care intervention also significantly reduced the rate of deep vein thrombosis in patients with lung cancer after treatment (e.g., postresection, chemotherapy, and PICC catheter chemotherapy) and grouping (randomized and non-randomized), and there was still no heterogeneity between studies. The sensitivity analysis found that after changing the effect model and excluding Wang et al.
[10] (with the largest weight ratio), the meta-analysis results were [OR=0.16(0.11,0.24)] and [OR=0.16(0.10,0.25)], respectively, without significant changes
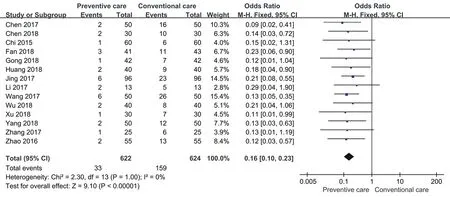
Figure 1. Clinical effect of preventive nursing on the rate of deep vein thrombosis in patients with lung cancer post-treatment
3.2.2 Clinical effect of preventive nursing on nursing satisfactions in patients with lung cancer post-treatment
A total of 7 studies [6, 11-14, 16, 18] reported nursing satisfaction, and the results of meta-analysis were shown in figure 2. I2=0, P=0.93, so there was no heterogeneity among the studies, and the fixed model was adopted. The results of meta-analysis showed that compared with conventional nursing intervention, preventive nursing intervention could significantly improve the nursing satisfaction of lung cancer patients [OR=6.85(3.58,13.11)]. The same conclusion was reached in subgroups of lung cancer resection, and no heterogeneity was found. According to the sensitivity analysis, the meta-analysis results were [OR=6.42(3.32,12.41)] and [OR=6.41(3.29,12.49)] after changing the effect model and excluding Zhang et al. [14] (with the largest weight ratio), and there was no significant change.
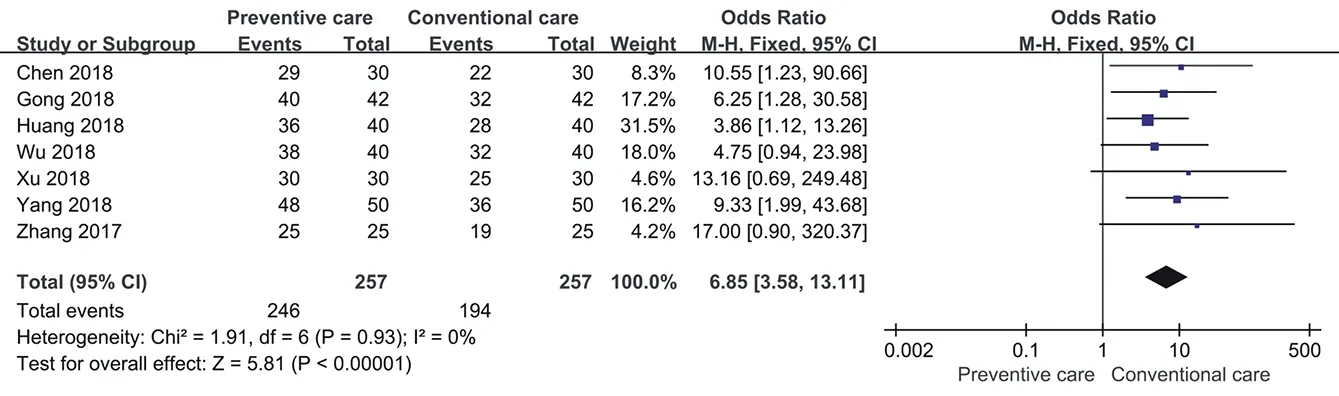
Figure 2. Clinical effect of preventive nursing on nursing satisfactions in patients with lung cancer post-treatment
3.2.3 Clinical effect of preventive nursing on average stay in patients with lung cancer post-treatment
A total of 5 studies [6, 9, 12, 14-15] reported the average length of hospital stay of patients, and the results of meta-analysis were shown in figure 3. I2=18%, P=0.30, therefore, there was no heterogeneity among the studies and a fixed model was adopted. The results of meta-analysis showed that compared with conventional nursing intervention, preventive nursing intervention could significantly reduce the mean hospital stay of lung cancer patients [MD=-7.41(-8.16, -6.65)]. According to the sensitivity analysis, the meta-analysis results were [MD=-7.41(-8.26, -6.55)] and [MD=-7.06(-7.97, -6.15)] after changing the effect model and excluding Xu et al. [12] (with the largest weight ratio), and there was no significant change.

Figure 3. Clinical effect of preventive nursing on average stay in patients with lung cancer post-treatment
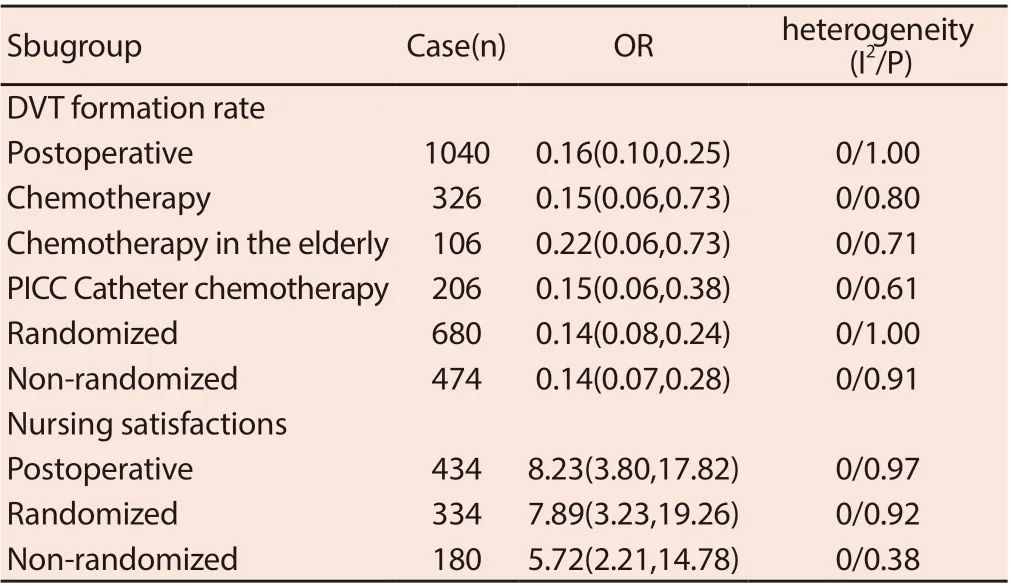
Table 2. Subgroup analysis
3.3 Publication bias
The funnel plots of the rate of deep vein thrombosis, nursing satisfaction and mean length of stay in patients with lung cancer treated by preventive care are shown in figure 4, figure 5 and figure 6, respectively. The graphs show approximate symmetry, but linguistic bias is unavoidable.

Figure 4. Funnel plot of preventive nursing on the rate of deep vein thrombosis in patients with lung cancer post-treatment

Figure 5. Funnel plot of preventive nursing on nursing satisfactions in patients with lung cancer post-treatment

Figure 6. Funnel plot of preventive nursing on average stay in patients with lung cancer post-treatment
4. Discussion
Our study found that preventive care intervention after treatment of lung cancer patients could not only significantly reduce the formation rate of DVT and improve nursing satisfaction, but also shorten the average hospitalization time of patients by about 1 week. There was no heterogeneity among the studies, and sensitivity analysis showed that our results were very stable.
Our subjects underwent surgery or chemotherapy, both of which are risk factors for venous thrombosis. The activation of coagulation system stress in patients with lung cancer by surgery and the postoperative braking of patients themselves are prone to lead to thrombosis [20]. Chemotherapy drugs can directly damage the vascular endothelium and start the coagulation mechanism, and the damaged tumor cells can also release a large amount of inflammatory substances and pro-coagulation factors [5]. In addition, some patients need multiple rounds of chemotherapy, so peripheral central venous catheter (PICC) will be used for infusion, which will also lead to severe vascular endothelial injury, phlebitis and thrombosis [21]. However, conventional nursing care is not effective in the prevention of deep vein thrombosis in lung cancer patients, so it is particularly important to explore new nursing methods.
The content of preventive nursing intervention mainly includes: (1) Health education, nursing staff to tell patients in detail the cause of deep vein thrombosis, harm and prevention and treatment methods, to increase patients' cognition of deep vein thrombosis. (2) Risk assessment. After treatment (surgery or chemotherapy), patients were evaluated by deep vein thrombosis risk assessment scale, which was divided into low risk, medium risk and high risk. For low-risk patients (unilateral limb swelling), nurses should strengthen the monitoring of patients' swollen limbs, and implement thrombolysis and anticoagulant treatment strictly in accordance with the doctor's advice. For patients with moderate risk (limb swelling, compression pain and other phenomena, and visible thrombosis), nursing staff should instruct the patients to ensure absolute bed rest, as advised by the doctor to use LMWH sodium for anticoagulant treatment; For high-risk patients (limb swelling is obvious, and deep vein thrombosis is severe), nurses should strengthen the continuous monitoring of central venous pressure, blood routine and biochemical indicators, and make detailed records of patients' hourly urine volume and access volume, and then conduct risk assessment for patients after 4 hours of medication. (3) Psychological nursing, alleviating the negative psychological effect of patients. (4) Drug guidance, mainly including post-treatment analgesic drugs. Our subgroup analysis found that in a variety of treatment methods, such as lung cancer resection, lung cancer chemotherapy, elderly lung cancer chemotherapy and lung cancer PICC catheter chemotherapy, preventive nursing intervention can effectively reduce the formation rate of DVT, without heterogeneity. Moreover, nursing satisfaction is also guaranteed, so the clinical application scope of preventive nursing intervention to prevent DVT formation in lung cancer patients after treatment is expanded. In addition, long-term hospitalization and its costs are also an important source of great psychological stress for patients. The preventive nursing intervention can reduce the hospitalization time of patients by about a week, which undoubtedly also reduces the psychological burden of patients.
Of course, our research has certain limitations. First, although we searched the English database, no qualified English studies were included, so language bias was inevitable. Second, DVT has subtype differences in the occurrence of lung cancer, such as a high incidence of non-small cell lung cancer [23], and whether the effect of preventive nursing intervention also has subtype differences is unknown. Finally, due to limited data, it is not clear whether there is any difference between different lung cancer resection methods. Despite certain limitations, there was no heterogeneity between our studies and the results of sensitivity analysis were stable. Therefore, preventive nursing intervention may be of great benefit to the prevention of DVT formation in patients with lung cancer after treatment, and it may also shorten the average hospitalization time of patients and get patients' satisfaction. Therefore, further promotion can be attempted in clinical practice.
杂志排行
Journal of Hainan Medical College的其它文章
- A network pharmacology approach to explore action mechanisms of Bi xie and Tu fuling for treating gouty arthritis
- Study on the value of parecoxib sodium preemptive analgesia for laparoscopic surgery based on postoperative pain and stress mediator secretion
- Changes of serum β2-MG, Cys C and urine mAlb levels in patients with ureteral calculi before and after extracorporeal shock wave lithotripsy and their clinical significance
- Study on the effect of Baiban Ointment on the whole gene expression profile of vulvar sclerosing lichen
- To investigate the effects of butylphthalide on reducing neuronal apoptosis in rats with cerebral infarction by inhibiting the JNK / P38 MAPK signaling pathway
- Study of KAP status and influencing factors of Protective Behaviour on COVID-19 among Hainan Mobile Phone Users
