腹腔镜结直肠癌根治术对患者围术期机体代谢及胃肠功能的影响分析
2020-05-25徐众
徐众
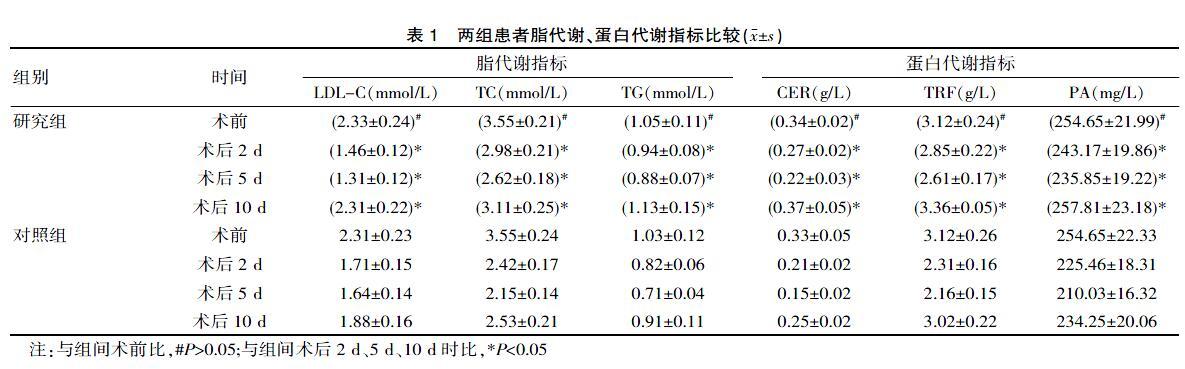
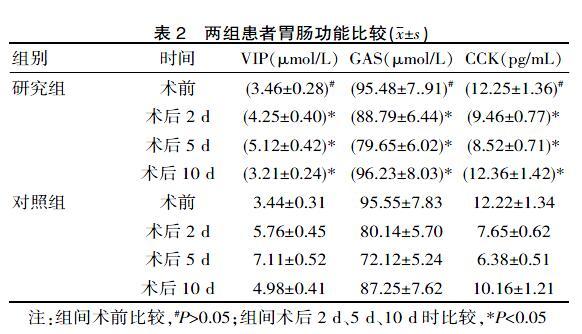
[摘要] 目的 分析研讨腹腔镜结直肠癌根治术对患者围术期机体代谢及胃肠功能的影响。方法 从该院2018年1月—2019年1月期间收治的结直肠癌患者中随机抽取92例进行讨论,按治疗方式分组研究组(46例腹腔镜结直肠癌根治术治疗)和对照组(46例开腹手术治疗),观察比较治疗状况,如围术期胃肠功能、脂代谢、蛋白代谢等。结果 术前脂代谢、蛋白代谢指标差异无统计学意义(P>0.05);研究组LDL-C术后2 d(1.46±0.12)mmol/L、5 d(1.31±0.12)mmol/L、10 d(2.31±0.22)mmol/L时优于对照组(1.71±0.15)mmol/L、(1.64±0.14)mmol/L、(1.88±0.16)mmol/L,术后2 d TC(2.98±0.21)mmol/L、TG(0.94±0.08)mmol/L、术后5 d TC(2.62±0.18)mmol/L、TG(0.88±0.07)mmol/L高于对照组2 d TC(2.42±0.17)mmol/L、TG(0.82±0.06)mmol/L、5 d TC(2.15±0.14)mmol/L、TG(0.71±0.04)mmol/L,术后2 d、5 d、10 d CER[(0.27±0.02)g/L、(0.22±0.03)g/L、(0.37±0.05)g/L)]、TRF[(2.85±0.22)g/L、(2.61±0.17)g/L、(3.36±0.05)g/L)]、PA[(243.17±19.86)mg/L、(235.85±19.22)mg/L、(257.81±23.18)mg/L)]高于對照组2 d、5 d、10 d CER[(0.21±0.02)g/L、(0.15±0.02)g/L、(0.25±0.02)g/L)]、TRF[(2.31±0.16)g/L、(2.16±0.15)g/L、(3.02±0.22)g/L)]、PA[(225.46±18.31)mg/L、(210.03±16.32)mg/L、(234.25±20.06)mg/L)](P<0.05)。组间术前胃肠功能指标差异无统计学意义(P>0.05),研究组术后2 d、5 d、10 d VIP低于对照组,GAS、CCK高于对照组(P<0.05)。结论 与开腹手术比较,腹腔镜结直肠癌根治术治疗结直肠癌疾病更为适合,此方式对患者围术期脂代谢、胃肠功能、蛋白代谢等指标的影响较小,有利于术后康复。
[关键词] 结直肠癌;腹腔镜;开腹手术;结直肠癌根治术;围术期
[中图分类号] R735.3 [文献标识码] A [文章编号] 1674-0742(2020)01(c)-0016-04
Effect of Laparoscopic Radical Resection of Colorectal Cancer on Body Metabolism and Gastrointestinal Function during Perioperative Period
XU Zhong
Department of General Surgery, Haixiya Hospital of Shanxian County, Heze, Shandong Province, 274300, China
[Abstract] Objective To analyze and discuss the effect of laparoscopic radical resection of colorectal cancer on metabolism and gastrointestinal function during perioperative period. Methods 92 patients with colorectal cancer admitted to the hospital from January 2018 to January 2019 were randomly selected for discussion. They were divided into study group (46 cases of laparoscopic radical resection of colorectal cancer) and control group (46 cases of open surgery). The treatment status, such as perioperative gastrointestinal function, lipid metabolism and protein metabolism, were observed and compared. Results There was not statistically signifiant difference in preoperative lipid metabolism and protein metabolism indexes before surgery(P>0.05). The LDL-C of the study group was lower at 2 d (1.46±0.12) mmol/L, 5 d (1.31±0.12) mmol/L, and 10 d (2.31±0.22) mmol/L better than the control group (1.71±0.15) mmol/L, (1.64±0.14) mmol/L, and (1.88±0.16) mmol/L. At 2 d, TC (2.98±0.21) mmol/L, TG (0.94±0.08) mmol/L, 5 d, TC (2.62±0.18) mmol/L, TG (0.88±0.07) mmol/L, TG (0.82±0.06) mmol/L, 5 d, TC (2.15±0.14) mmol/L, TG (0.71±0.04) mmol/L, Postoperative CER[ (0.27±0.02) g/L, (0.22±0.03) g/L, (0.37±0.05)g/L], TRF [(2.85±0.22) g/L, TRF (2.61±0.17) g/L, (3.36±0.05) g/L], PA[ (243.17±19.86) mg/L, (235.85±19.22) mg/L, (257.81±23.18) mg/L] at 2 d, 5 d and 10 d were higher than those in the control group[ CER(0.21±0.02) g/L, (0.15±0.02) g/L, (0.25±0.02) g/L)], TRF[(2.31±0.16) g/L, (2.16±0.15) g/L, (3.02±0.22) g/L], PA [(225.46±18.31) mg/L, (210.03±16.32) mg/L, (234.25 ±20.06) mg/L](P<0.05). There was not statistically significant difference in preoperative gastrointestinal function indexes between groups(P>0.05). At 2 d, 5 d and 10 d after surgery, the VIP of the study group was lower than that of the control group, and GAS and CCK were higher than that of the control group (P<0.05). Conclusion Compared with open surgery, laparoscopic radical resection of colorectal cancer is more suitable for the treatment of colorectal cancer. This method has less influence on perioperative lipid metabolism, gastrointestinal function, protein metabolism and other indicators
综上所述,与开腹手术比较,腹腔镜结直肠癌根治术治疗结直肠癌疾病更为适合,此方式对患者围术期脂代谢、胃肠功能、蛋白代谢等指标的影响较小,有利于术后康复。
[参考文献]
[1] 吴涛, 陆春雷, 葛晨,等. 腹腔镜用于结直肠癌根治术对患者围术期机体代谢及胃肠功能的影响[J].广西医科大学学报, 2017, 34(10):1498-1499.
[2] 许正国, 郭世伟, 金鹏程. 腹腔镜结直肠癌根治术患者围术期机体代谢及胃肠功能的变化观察[J]. 中国医师杂志, 2018, 20(3):391-393.
[3] 余启松, 黄合超,丁峰,等.腹腔镜结直肠癌根治术对结直肠癌患者胃肠功能和生存质量的影响[J].中国临床医生杂志, 2017, 45(8):76-79.
[4] 吳文生. 腔镜结直肠癌根治术对结直肠癌患者临床疗效及胃肠功能的影响[J].检验医学与临床,2017,14(Z1):300-302.
[5] 高王军, 李福广.腹腔镜结直肠癌根治术对结直肠癌患者临床疗效及胃肠功能的影响[J]. 癌症进展,2016,14(9):910-912.
[6] 丁海涛, 帕尔哈提·阿布都热衣木,韩智君,等.结直肠癌NOSE术对患者氧化应激、免疫功能及机体微炎症的影响[J]. 中国现代手术学杂志, 2017, 21(1):9-13.
[7] 胡子龙, 吴有军, 胡时栋,等. 腹腔镜与开腹结直肠癌手术对机体免疫功能影响及其疗效分析[J].中国病案,2018, 19(4):82-85.
[8] 莫琳, 刘保荣. 腹腔镜与开腹直肠癌根治术对直肠癌患者机体炎症和免疫功能的影响[J].解放军医药杂志,2017, 29(12):28-31.
[9] 闫军, 李亮,陈曦.腹腔镜直肠癌根治术与开腹手术近期疗效及对机体免疫的影响[J].中国现代普通外科进展, 2016, 19(8):592-595.
[10] 王亮,田洁,许跃军,等.后腹腔镜肾癌根治术患者围术期机体代谢与创伤应激的变化观察[J].实用癌症杂志, 2017, 32(7):1189-1191.
[11] 王建锋, 王耿泽, 张海洋,等.腹腔镜结直肠癌根治术患者围术期机体代谢及胃肠功能的变化观察[J].实用癌症杂志, 2018, 33(9):1499-1501.
(收稿日期:2019-10-23)
