Novel insight into perirenal adipose tissue: A neglected adipose depot linking cardiovascular and chronic kidney disease
2020-05-12NaHuangEnWenMaoNingNingHouYongPingLiuFangHanXiaoDongSun
Na Huang, En-Wen Mao, Ning-Ning Hou, Yong-Ping Liu, Fang Han, Xiao-Dong Sun
Na Huang, En-Wen Mao, Ning-Ning Hou, Yong-Ping Liu, Xiao-Dong Sun, Department of Endocrinology, Affiliated Hospital of Weifang Medical University, Weifang 261031,Shandong Province, China
Fang Han, Department of Pathology, Affiliated Hospital of Weifang Medical University,Weifang 261031, Shandong Province, China
Abstract
Obesity is associated with adverse metabolic diseases including cardiovascular disease (CVD) and chronic kidney disease (CKD). These obesity-related diseases are highly associated with excess fat accumulation in adipose tissue. However,emerging evidence indicates that visceral adiposity associates more with metabolic and cardiovascular risk factors. Perirenal adipose tissue, surrounding the kidney, is originally thought to provides only mechanical support for kidney.However, more studies demonstrated perirenal adipose tissue have a closer association with renal disease than other visceral fat deposits in obesity.Additionally, perirenal adipose tissue is also an independent risk factor for CKD and even associated more with CVD. Thus, perirenal adipose tissue may be a connection of CVD with CKD. Here, we will provide an overview of the perirenal adipose tissue, a neglected visceral adipose tissue, and the roles of perirenal adipose tissue linking with CVD and CKD and highlight the perirenal adipose tissue as a potential strategy for future therapeutics against obesity-related disease.
Key words: Adipose tissue; Cardiovascular diseases; Kidney diseases; Obesity;Abdominal fat; Endothelium
INTRODUCTION
Obesity is regarded as a risk factor for adverse metabolic diseases including hypertension, type 2 diabetes, and dyslipidemia[1-3]. These metabolic disorders cause vascular complications that primarily manifest as cardiovascular disease (CVD) and chronic kidney disease (CKD)[4,5]. Moreover, these obesity-related diseases are strongly associated with the prevalence and severity of overweight/obesity. During the development of obesity, impaired glucose homeostasis, hypertension, dyslipidemia,and changes in blood hemodynamics may contribute to the pathogenesis of obesityrelated diseases[6]; these abnormal metabolic changes are mainly caused by excess fat accumulation in adipose tissue[7,8]. However, there is emerging evidence that,compared with obesity itself, body fat distribution is more closely related to the pathogeneses and development of obesity-related diseases (including CVD and obesity-related CKD)[9-11].
Adipose tissue mainly comprises a large number of adipocytes. As the main energy storage and endocrine organ, adipose tissue can maintain lipid metabolism homeostasis and energy balance by contributing to several physiological processes through secretion of various adipokines/cytokines[12,13]. Adipose tissue is traditionally classified into visceral adipose tissue (in the trunk cavity) and subcutaneous adipose tissue (under the skin), based on morphological appearance and location[14].Compared with subcutaneous adipose tissue, visceral adipose tissue is reportedly more closely associated with metabolic and cardiovascular risk factors, such as insulin resistance, dyslipidemia, hypertension, and atherosclerosis[15,16]. Perirenal adipose tissue (PRAT) is a component of visceral adipose tissue that surrounds the kidney,which was originally presumed to only provide mechanical support for the kidney.However, PRAT has been shown to demonstrate a closer relationship to renal disease among individuals with obesity, compared with other visceral fat deposits[17]. In addition, the presence of excess PRAT has been identified as an independent risk factor for CKD and a factor associated with the development of CVD[18-22]. Thus, PRAT may serve to connect CVD with CKD among individuals with obesity. This review will provide an overview of PRAT, a neglected visceral adipose tissue, as well as the roles of PRAT in linking CVD and CKD. Moreover, it will highlight the potential for PRAT as a therapeutic target in the treatment of obesity-related diseases.
GENERAL BACKGROUND OF PERIRENAL ADIPOSE TISSUE
PRAT is a fat pad located in the retroperitoneal space surrounding the kidney, which fills the space between the kidney and neighboring retroperitoneal tissues, renal parenchyma, and adrenal gland; the PRAT is supported by renal fascia[23]. Fat around the renal sinus is also regarded as a component of PRAT. Notably, PRAT is the only adipose tissue that is surrounded by a multilayered fibrous membrane. Because PRAT is surrounded by fascia tissue, excess PRAT can tightly encapsulate the kidney and cause excessive renal compression. Despite its origination from preadipocytes, PRAT undergoes an unusual progressive transition from brown adipose tissue into white adipose tissue after birth[24]. Brown adipocytes form the majority of PRAT in fetuses and newborn infants (1-11 mo), while white adipocytes comprise the outermost thin layer[25]. With increasing age, only a small proportion of brown adipocyte areas remains within perirenal white adipose tissue in adults; thus, PRAT constitutes a combination of white adipose tissue and brown adipose tissue[26]. One study in Siberia showed that approximately 40% of PRAT exhibited morphology typical of brown adipocytes, while approximately 30% expressed uncoupling protein 1; these findings suggest that PRAT can be converted to brown adipose tissue in cold conditions[27].
Despite its atypical nature, PRAT has been reported to synthesize and secrete adipokines and pro-inflammatory cytokines, including adiponectin, leptin, visfatin,resistin, tumor necrosis factor-α, interleukin-6 (IL-6), and IL-1β[22]. These cytokines enter nearby kidneys and serve to regulate renal function through endocrine or paracrine pathways[28].
Anatomically, PRAT exhibits extensive vascularization, innervation, and lymph fluid drainage. The PRAT artery originates from branches of the abdominal aorta,include branches of the inferior adrenal, dorsal, and gonadal arteries[29]. Perirenal nerve fibers originate from the celiac superior mesenteric, ipsilateral inferior mesenteric, adrenal, aorticorenal, ovarian, testicular, and ipsilateral sympathetic chain ganglia[30]. Perirenal lymphatic vessels communicate with renal subcapsular lymphatic vessels and then drain into para-aortic lymph nodes[31]. These features allow interrelationships between kidney and PRAT, as well as between body function and PRAT,viasecretion of adipokines and cytokines.
ASSESSMENT OF OBESITY AND PERIRENAL ADIPOSE TISSUE
Because of the increasing prevalence of obesity, accurate quantification of obesity has become necessary. Traditional simple indicators (e.g., body mass index, waist circumference, and waist/hip ratio) have been widely used in clinical practice.Although these indicators are convenient and noninvasive for patients, they have obvious limitations. In particular, they are ethnicity specific and cannot accurately differentiate between visceral and subcutaneous fat, between muscle and adipose tissue; moreover, they cannot determine the regional distribution of adiposity throughout the body[8,32]. Advanced imaging techniques (e.g., computed tomography,magnetic resonance imaging, and positron emission tomography) have been utilized to evaluate body fat distribution, including PRAT thickness[33-35]. Although these techniques are more accurate, widespread clinical use of computed tomography and magnetic resonance imaging for evaluation of obesity is unsuitable because of the cost and time involved, as well as the exposure to ionizing radiation. Some noninvasive ultra-sonographic methods have been reported for assessment of fat distribution[20,36].Armelliniet al[37]first described the use of ultrasonography for direct evaluation of intra-abdominal fat deposits. Subsequently, Kawasakiet al[38]reported a more convenient method for quantification of visceral fat by measuring PRAT thickness on abdominal sonography. Measurement of PRAT can be performed as following: keep the patient in the supine position; place the ultrasound probe vertically to the abdominal lateral surface skin above the kidney; obtain the ultrasound longitudinal scan of the kidney which is almost parallel to the skin. Gender pressure of the probe should be noticed during image obtaining in order not to cause extra adipose tissue pressing. PRAT thickness was then measured from the kidney surface to inner side of abdominal musculature. Average measurement of the maximum thickness values of both sides by three times was regarded as ultrasound measure. Kawasakiet al[38]showed that PRAT thickness was positively correlated with visceral adipose tissue area and that PRAT thickness > 10 mm could be regarded as visceral fat accumulation(area > 100 cm2). In a separate analysis, our research group found that the average of PRAT thickness in healthy people was 7.95 mm and that in obese patients was 26.54 mm[17]. And PRAT was positively associated with body mass index and waist circumference; thus, sonographic evaluation of PRAT thickness could be used to assess visceral fat and predict early renal injury in patients with obesity[17]. Lamacchiaet al[21]measured PRAT thickness in normal subjects (8 mm ± 2 mm for men and 5 mm± 2 mm for women), which were validated by computed tomography measurements.With the same method, De pergolaet al[39]found an average value of PRAT in obese patients with body mass index above 30 kg/m2was 25.0 mm. Ricciet al[40]verified that PRAT was statistically different between hypertensive and nonhypertensive patients,with average value of 13.6 and 11.6 mm, respectively.
PERIRENAL ADIPOSE TISSUE AND CHRONIC KIDNEY DISEASE
Relationship between PRAT and CKD
The association of obesity with CKD was first reported in 1974; obesity was linked with massive proteinuria[41]. Thereafter, many epidemiologic studies have demonstrated that kidney disease is an independent complication of obesity; these manifestations are regarded as obesity-related glomerulopathy or obesity-related kidney disease[42,43]. Klausenet al[44]screened 2696 volunteers over a period of 10 years and found that obesity was strongly associated with proteinuria. Ejerbladet al[45]observed that patients with a body mass index > 25 kg/m2had a nearly three-fold increased risk of CKD, compared with lean patients; this risk was not affected by age.Furthermore, urinary albumin excretion was significantly greater among patients with obesity who did not have hypertension or diabetes, compared with healthy controls[17]. Compared with overall obesity, abdominal obesity was found to be more strongly associated with kidney injury[46,47]; notably, a retrospective study of 7676 patients without diabetes showed that lean patients who had abdominal obesity were at higher risk of CKD[47]. As mentioned above, PRAT has been used in measurement of visceral fat deposition. PRAT thickness was found to be markedly higher among patients with obesity who exhibited microalbuminuria, compared with healthy controls and patients with obesity who did not exhibit albuminuria[17]. The presence of excess PRAT was related to a 2.3-fold increased risk of CKD, following adjustments for body mass index and the presence of excess visceral adipose tissue[48]. Lamacchiaet al[21]found that PRAT thickness could predict reduced glomerular filtration rate in patients with type 2 diabetes. Furthermore, PRAT thickness was positively associated with microalbuminuria in patients with obesity[17,49]. Based on these findings, the presence of excess PRAT is considered an independent predictor of renal injury in patients with obesity or diabetes.
Potential mechanism for participation of PRAT in CKD
The detailed mechanisms by which PRAT initiates and exacerbates chronic renal injury remain elusive (Table 1). First, excess PRAT surrounded by renal fascia penetrates the renal sinus, obstructing renal parenchyma and vessels, promoting sodium reabsorption, and raising blood pressure. Excess PRAT encapsulates the kidney, further increasing interstitial hydrostatic pressure and reducing renal blood flow; these effects lead to hemodynamic changes, including altered renin secretion and glomerular filtration[50-53].
Second, hallmarks of obesity include overproduction of free fatty acids (FFAs) and chronic inflammation. Our previous study verified that PRAT thickness is positively associated with urine albumin excretion and circulating FFAs[17]. Notably, circulating FFAs levels were found to be significantly higher in renal venous blood than in jugular venous blood, indicating that FFAs released by PRAT participate in kidney damage as direct or indirect mediators through intercellular signaling pathways[54].Excess FFAs produced by PRAT could escape into the kidney directly orviarenal vascular system based on its extensive vascularization. Adeosunet al[55]verified that FFAs from PRAT cause renal lipotoxicity through uptake of FFA metabolites, such as ceramides. Then FFAs-induced renal lipotoxicity could exacerbate chronic inflammation by increasing the metabolism of intracellular fatty acids. Furthermore,our physiology-based analysis showed that FFAs could directly impair endothelial function by enhancing oxidation of tetrahydrobiopterin; this leads to L-arginineinduced production of superoxide, rather than nitric oxide (NO), by uncoupling of endothelial NO synthase[56]. The reduction in NO level could lead to a compensatory enhancement of vascular endothelial growth factor secretion by podocytes, thereby initiating endothelial cell proliferation and permeability, which causes greater albumin leakage from glomeruli[56]. This uncoupling of glomerular vascular endothelial growth factor-NO axis could be improved by reduction of FFAs and inflammation[56,57]. Besides, FFAs-induced lipotoxicity can also increase renal arterial resistance, indicated by the high interlobar artery resistance in patients with microalbuminuria[49].
Third, excess PRAT can affect kidneys by systemic or local secretion of inflammatory cytokines[53,58]. Endothelial/vasomotor dysfunction is an early sign of vascular damage. PRAT secretes tumor necrosis factor-α, which has been shown to directly impair renal arterial endothelial dysfunction in obese swine[59]. Potential mechanism may be due to its impairment on endothelial NO balance as mentioned before. Moreover, PRAT-related inflammation and extracellular-matrix protein can be reduced by blocking plasminogen activator inhibitor-1; this mechanism was able to attenuate renal injury in obese mice[60]. Liet al[61]found that leptin secreted by excess PRAT could exacerbate renal vascular remodeling and glomerular endothelial cell proliferation by activation of the p38 MAPK pathway. These inflammatory adipocytes/cytokines could modulate cellular functionviacertain signaling pathways while attracting infiltrating macrophages into deposited fat, further exacerbating oxidative stress and adipocyte dysfunction[62]. Interestingly, inhibiting the levels of inflammatory cytokines including IL-6, IL-1b and tumor necrosis factor-α in PRAT through upregulation of heme oxygenase system reduced renal inflammation and ameliorated diabetic nephropathy[63]. However, precise mechanism still warrants further studies.
Finally, excess PRAT can act in a synergistic manner with metabolic risk factors to exacerbate renal damage. Patients with metabolic syndrome have greater PRAT thickness, as well as increased oxidative stress and renal microvascularproliferation[64]. Greater PRAT thickness has been associated with abnormal insulin levels, impaired fasting glucose, insulin resistance, increased triglyceride levels, and abnormal uric acid levels in patients with CKD[19,65]. One possibility is that increased FFAs and inflammatory cytokines secreted from PRAT or visceral fat impair insulinrelated signaling way including PI3K/Akt inhibition and activation of protein kinase C. Insulin increases sodium retention in renal tubules, stimulates the sympathetic nervous system, and acts directly on vascular structures that contribute to kidney damage[66].
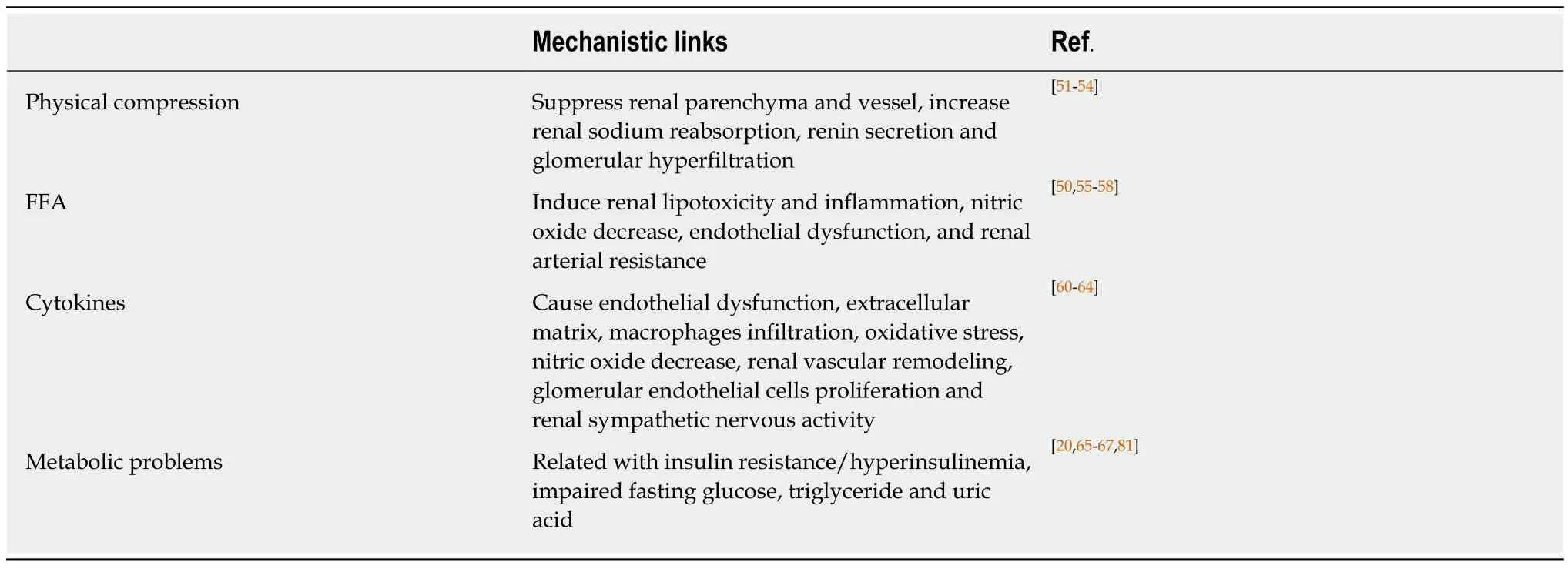
Table 1 Potential mechanism for participation of perirenal adipose tissue in chronic kidney disease
PERIRENAL ADIPOSE TISSUE AND CARDIOVASCULAR DISEASE
Relationship between CKD and CVD
Obesity is considered a strong risk factor for CVD. Since Yudkinet al[67]first reported relationships between CKD and atherosclerosis, as well as between CKD and coronary heart disease, many epidemiological studies have confirmed a close association between CKD and CVD. The LIFE[68]and PREVEND[69]studies demonstrated that the incidence and mortality of ischemic CVD increased significantly with increasing urine albumin excretion. Furthermore, an analysis of 21050 patients in 26 countries showed that microalbuminuria was closely related to cardiovascular hazards and CVD[70]. Among individuals without diabetes and hypertension, CVD-related mortality is significantly higher in those with microalbuminuria than in those without microalbuminuria[71]. In the general population, the presence of microalbuminuria is predictive of the risks of diabetes,hypertension, and CVD[72,73]. Therefore, patients with CKD have higher risks of cardiovascular events, such as hypertension, atherosclerosis, and coronary heart disease[74]. Consistent with these observations, patients with early CKD tend to die from CVD, rather than terminal end-stage renal disease.
Relationship between PRAT and CVD
Visceral fat reportedly has a close association with CVD. As a component of visceral fat, the presence of excess PRAT has been recently identified as an emerging risk factor for CVD, independent of common metabolic parameters[40]. De Pergolaet al[39]found that PRAT thickness was positively correlated with blood pressure in patients with overweight and obesity. Ricciet al[40]demonstrated a close association between PRAT and high blood pressure, such that PRAT can be regarded as a predictor of hypertension. Higher levels of PRAT thickness and carotid intima-media thickness were both found in HIV-infected patients with visceral adiposity, indicating that the presence of excess PRAT is associated with atherosclerosis[75]. Notably, the associations of PRAT with carotid intima-media thickness and diverse metabolic risk factors were present even in children[76].
As a metabolic risk factor related to CVD, PRAT associated with diabetes or dyslipidemia may also indirectly affect CVD. A cross-sectional study showed that the presence of excess PRAT was independently associated with hyperinsulinemia and insulin resistance in patients with obesity, independent of other anthropometric and metabolic parameters; this finding indicated that the presence of excess PRAT is a strong marker of insulin resistance[65,77]. PRAT development and remodeling have also been associated with metabolic syndrome[21,78]. In patients with CKD, the PRAT thickness was significantly correlated with metabolic risks, such as abnormal triglycerides and uric acid levels; patients with stages 4 and 5 CKD had the greatest PRAT thickness[19]. Excess PRAT is related to reductions in glomerular filtration rate,regardless of other indices of adiposity, in patients with hypertension[20]. Considering the above pathological processes, the presence of excess PRAT is believed to contribute to dysmetabolism-associated CVD. PRAT is potentially related to epicardial fat because both exhibit mesothelial layers similar to those of visceral organs, which are enriched in white adipose tissue progenitors that produce adipocytes[65]. This finding strengthens the hypothesis that excess PRAT is a predictor of the risk of CVD, because epicardial fat has been regarded as a risk factor for CVD that predicts the tendency of cardiac dysfunction.
Potential mechanism for participation of PRAT in CVD
Although there is a potential link between CKD and CVD, the mechanisms remain unclear (Figure 1). Potential mechanisms for perirenal fat-mediated CVD regulation are closely associated with anatomical, physiological, and localization features.
Importantly, efferent nerves have been found to innervate PRAT, while afferent nerves have been found in adipose tissue; the physiological functions of PRAT neural activity are presumably related to these anatomical characteristics. Afferent nerves of adipose tissue might control the sympathetic nervous system by forming a negative feedback loop (i.e., a reflex)[24]. Renal sympathetic outflow is increased by enhancement of afferent signals from fat deposits, followed by the elevation of arterial blood pressure; this reflex phenomenon is known as the “adipose afferent reflex”[24].Tanidaet al[79]injected leptin into PRAT; this resulted in activation of adipose afferent reflex without affecting the serum levels of sympathetic-activating substances,suggesting that PRAT may directly regulate the cardiovascular system. Excess PRAT is presumed to contribute to increased hydrostatic pressure and activation of reninangiotensin-aldosterone system through the compression of blood vessels, lymphatic vessels, and ureters; this may lead to the development of hypertension and atherosclerosis[80]. Additionally, adipokines/cytokines synthesized by excess PRAT could regulate functions of the cardiovascular systemviaautocrine, paracrine, and endocrine pathways using similar mechanisms to those described for CKD.
Moreover, endothelial injury is typically regarded as the main initiating event for atherosclerosis and CVD. The Danish Diabetes Center proposed the Steno hypothesis,in which the emergence of microalbuminuria indicates the existence of extensive systemic endothelial dysfunction and increased systemic vascular permeability[81].This may explain why CKD is an indicator of increased risk of CVD and can strongly predict the occurrence of CVD. Importantly, microalbuminuria reflects the presence of microvascular disease and early damage to renal function; it is also an independent risk factor for macrovascular disease and CVD, including the occurrence and development of cardiovascular events.
PROSPECTIVE THERAPEUTIC STRATEGIES
According to current literature, lifestyle intervention including diet control and suitable exercise should be the first line of treatment of obesity. Energyrestricted diets effectively reduce fat mass and impact cardiometabolic profiles[82]. Parrishet al[83]reported that a fish oil diet reduced PRAT and limited fat hypertrophy. Interestingly,altering meal frequency to twice a day has been demonstrated to combat obesity by reducing PRAT[84]. Additionally, intensity interval exercise (especially short time-high frequency) is proved to have beneficial effects on the body composition including reducing PRAT[85]. Bariatric surgery is another effective intervention for morbidly obese patients. Ricciet al[40]reported that PRAT in morbidly obese patients (body mass index > 35 kg/m2) significantly was reduced accompanied by a significant reduction in blood pressure after sleevegastrectomy.
As mentions above, PRAT is different from traditional visceral fat because it has characteristic of both brown- and white-fat. Jespersenet al[86]characterized the perirenal region of humans and identified the presence of dormant brown adipose tissue in the PRAT. This property suggests that reactivating dormant BAT into active BAT by cold exposure or β3-adrenoceptors stimulation may be an promising strategy for combatting obesity-related metabolic disease[27,87]. However, identifying specific drugs to induce white-to-brown adipocyte and delivering them locally or selectively to PRAT require technological advances and further research.
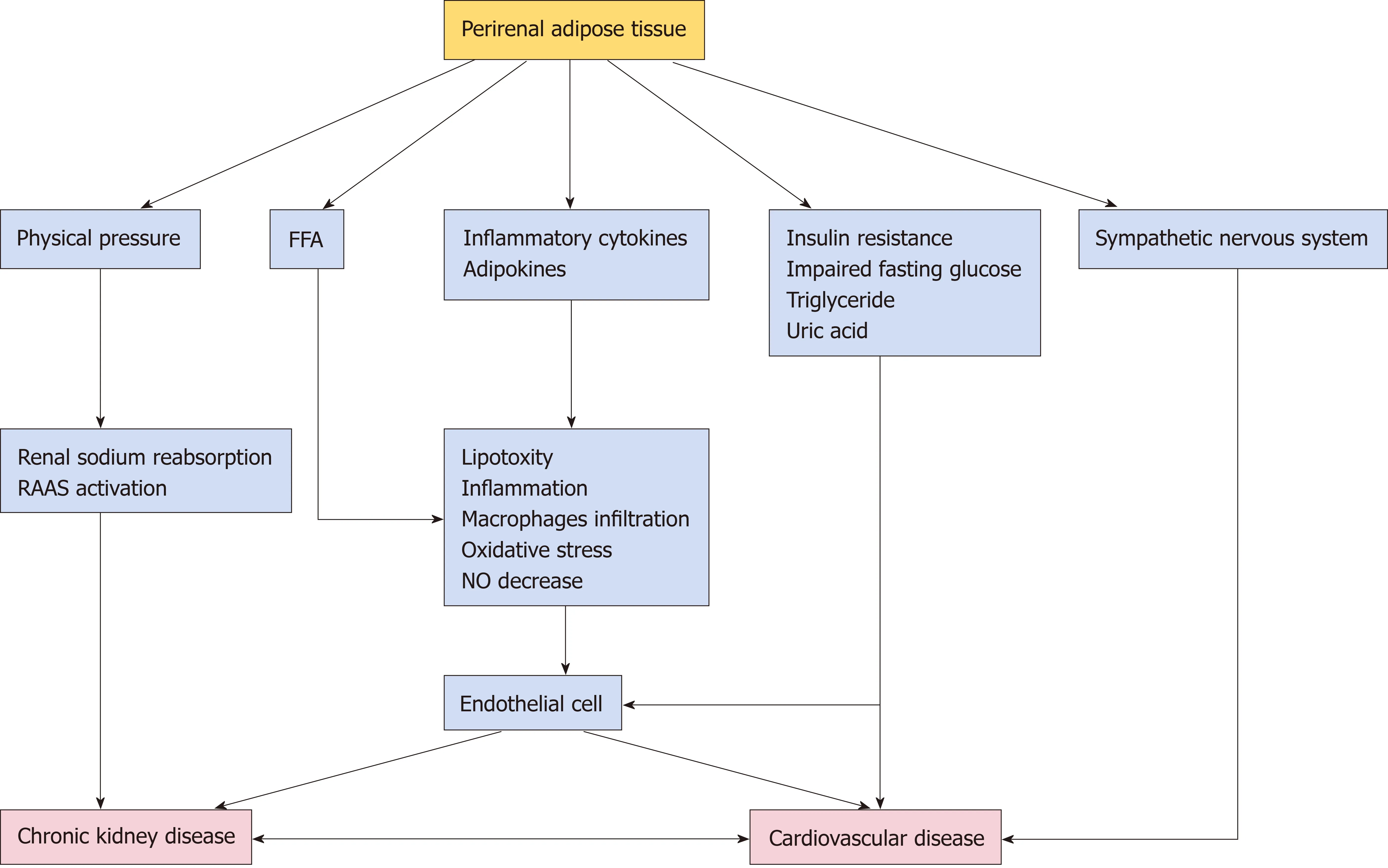
Figure 1 Potential mechanism for participation of perirenal adipose tissue in chronic kidney disease and cardiovascular disease. FFA: Free fatty acids; NO:Nitric oxide; RAAS: Renin-Angiotensin-Aldosterone System.
CONCLUSION
PRAT is a component of visceral fat that is strongly associated with adverse cardiometabolic risk factors for both CKD and CVD. Potential related mechanisms have been summarized in this review, with the aim of providing new insights and potential therapeutic targets for anti-obesity-related cardiovascular and kidney disease therapies. Further studies are needed to characterize the important roles of PRAT in the interactions between CKD and CVD. Drugs used to target CVD risk factors may influence PRAT in a manner that aids in disease prevention. The clinical implications of reducing PRAT accumulation by balanced diet, intermittent exercise,or other therapeutic interventions (e.g., burning excess energy through conversion of white adipose tissue to brown adipose tissue) with regard to CVD prevention remain unclear and should be established in future studies.
杂志排行
World Journal of Diabetes的其它文章
- Age of onset of diabetes and all-cause mortality
- Hydrocortisone, ascorbic acid and thiamine for sepsis: Is the jury out?
- Long-term effect of clopidogrel in patients with and without diabetes: A systematic review and metaanalysis of randomized controlled trials
- Lack of Syndecan-1 produces significant alterations in whole-body composition, metabolism and glucose homeostasis in mice
- Glargine-300: An updated literature review on randomized controlled trials and real-world studies
