NF-κB在一线抗结核药物诱导小鼠肝损伤中的作用
2020-04-20吴冬雪王雪张咪
吴冬雪 王雪 张咪
摘要 目的:研究一线抗结核药物诱导小鼠肝损伤发生过程中NF-κB变化情况。方法:48只昆明小鼠随机分为基线组和HRZ组(INH+RFP+PZA),于灌胃3d、5d、7d、10d、15d后处死。ELISA检测血清中ALT、AST含量。ELISA和RT-PCR检测肝组织中NF-κB、IκB mRNA及蛋白表达水平。结果:肝组织病理学及ALT、AST水平发生改变,提示肝损伤发生。与基线组相比,HRZ组NF-κB mRNA和蛋白水平呈上升趋势,IκB mRNA和蛋白水平逐渐下降。结论:NF-κB通路在抗结核药物性肝损伤小鼠模型中被激活。
关键词 抗结核药物;肝损伤;NF-κB;小鼠
中图分类号 R285 文献标识码 B 文章编号 1671-0223(2020)02-026-03
Abstract Objective To investigate the changes of NF-κB in liver injury induced by first-line antituberculosis drugs in mice. Methods Forty-eight Kunming mice were randomly divided into the baseline group and the HRZ group (INH + RFP + PZA), and were sacrificed after gavage on 3d, 5d, 7d, 10d, and 15d. The levels of ALT and AST in serum were detected by ELISA. ELISA and RT-PCR were used to detect the expression levels of NF-κB, IκB mRNA and protein in liver tissues. Results Changes in liver histopathology and ALT and AST levels suggest liver damage. Compared with the baseline group, the mRNA and protein levels of NF-κB in the HRZ group showed an increasing trend, and the mRNA and protein levels of IκB gradually decreased. Conclusions The NF-κB pathway is activated in mouse models of first-line anti-tuberculosis drug-induced liver injury.
Key words Anti-tuberculosis drug; Liver injury; NF-κB; Mice
異烟肼(INH)、利福平(RFP)和吡嗪酰胺(PZA)为一线抗结核药物,但治疗过程常常会发生抗结核药物性肝损伤(ADLI)。毫无疑问,ADLI是多因子介导的疾病,其发生机制尚不明确。有研究发现,氧化应激可显著影响ADLI的发生[1]。抗结核治疗期间会产生大量可与肝酶或膜受体结合致细胞代谢和功能紊乱的活性氧(ROS)[2]。核因子(NF)-κB是被证实可由ROS激活的真核细胞转录因子,ROS和NF-κB通过相互激活表现出正反馈效应[3]。静息状态时,胞质中NF-κB因与IκB结合而处于非活性状态。当细胞受到氧化剂等外界因素刺激时,IκB磷酸化,被释放的NF-κB发生核易位,进而参与基因表达的调控[4,5]。有研究表明,在乙醇引起的肝损伤中,肝细胞内NF-κB活性显著增加,与肝损伤程度呈高度正相关[6]。虽然NF-κB被证明与多种肝脏疾病有关,但NF-κB与ADLI之间的关系仍需要进一步研究。目前,临床上常用INH、RFP和PZA三种药物联合作为抗结核化疗方案,有研究表明药物间的相互作用会增加肝毒性[7]。但是,三种药物抗结核药物联合致肝损伤的机制仍不明确。
本研究在INH、RFP和PZA联合致小鼠肝损伤模型中观察肝组织中的NF-κB和IκB的mRNA和蛋白表达水平变化情况,进而探讨NF-κB在ADLI发生过程中的作用,为揭示ADLI的发生机制提供参考。
1 材料方法
1.1 动物模型
在中国阜康生物技术有限公司购买48只SPF级昆明小鼠(动物许可证号:SCXK(北京)2009-0004),雌雄各半,随机分为基线组和药物组(INH+RFP+PZA 90mg/Kg.d+135mg/Kg.d+315mg/Kg.d),于灌胃3d、5d、7d、10d、15d后处死。基线组8只小鼠,在开始灌胃之前一天处死。实验获得了动物伦理委员会的批准(批准号:14-016)。
1.2 检测指标
1.2.1 组织病理学改变
取肝组织,用福尔马林固定,脱水后包埋、切片,进行HE染色。使用光学显微镜观察肝组织病理变化。
1.2.2 检测小鼠血清ALT、AST水平
ELISA试剂盒(南京建成生物工程研究所)检测血清ALT、AST水平。
1.2.3 检测肝组织中NF-κB和IκB mRNA表达水平
TRIzol法提取总RNA,逆转录和RT-PCR使用试剂盒(Invitrogen公司),RT-PCR条件为94℃ 30s,63℃ 30s,72℃ 30s,35个循环。
1.2.4检测肝组织中NF-κB和IκB蛋白含量
肝组织和盐水按照1:4制成匀浆,离心并收集上清液。ELISA试剂盒(南京建成生物工程研究所)检测NF-κB和IκB蛋白含量。
1.3 统计分析
SPSS22.0处理数据,计量资料采用“均数±标准差”表示,多组间均数比较采用方差分析,两两比较采用LSD法,P<0.05为差异有统计学意义。
2 结果
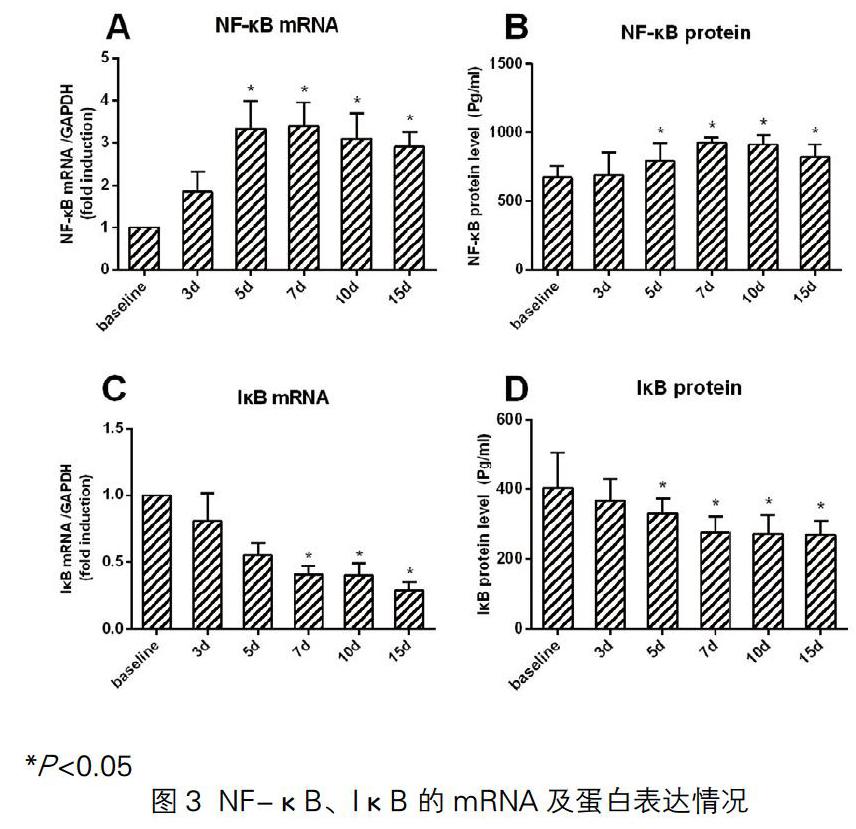
2.1 肝组织病理改变
基线组肝细胞无明显形态变化。HRZ组在3d开始表现出明显的形态学变化,肝细胞肿胀,炎性细胞增多,胞质空泡化,核皱缩,到15d损伤程度最为严重(图1)。
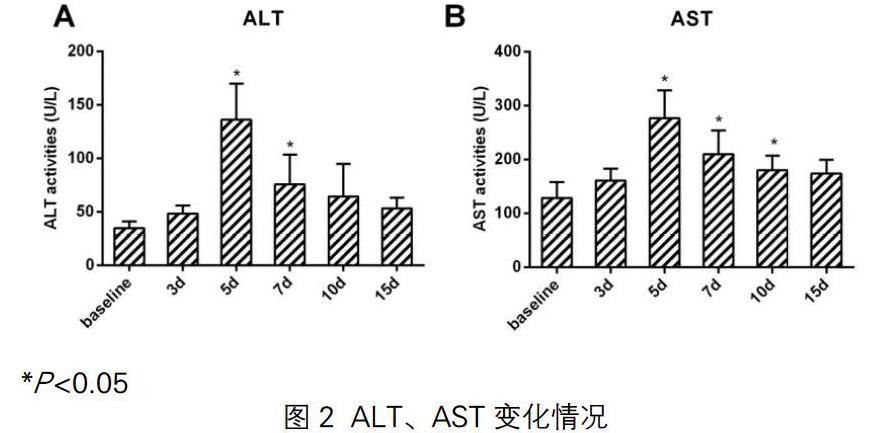
2.2 小鼠血清ALT、AST水平
与基线组相比,HRZ组的ALT和AST指标在第5天出现显著变化(均P <0.05),并且随着给药时间的延长,ALT和AST水平呈先升高后降低趋势(均P <0.05)(图2)。
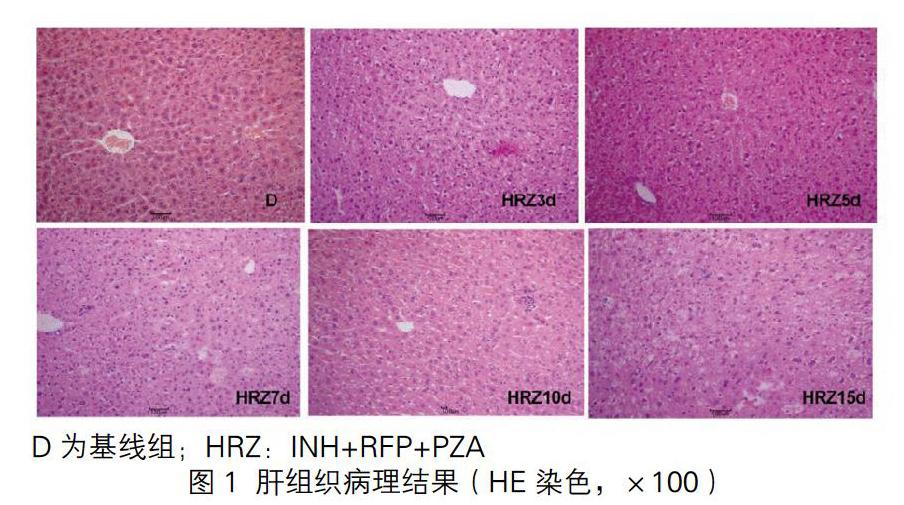
2.3 小鼠肝组织NF-κB 和IκB mRNA及蛋白表达
与基线组相比,HRZ组NF-κB的mRNA及蛋白表达在第5天出现显著变化,呈现先升高后略降低趋势(均P <0.05)。IκB的mRNA和蛋白水平从第1天至第15天逐渐下降(均P <0.05),且在第7天出现显著变化(均P <0.05)(图3)。
3 讨论
静息状态时,胞质中NF-κB因与IκB结合而处于非活性状态[8,9]。当细胞受到氧化应激刺激时,氧化应激可导致IκB降解并與NF-κB分离[10]。活化的NF-κB易位入核与炎症介质靶基因启动子区域的κB位点结合,导致炎症介质基因的过表达[11,12]。本研究中,NF-κB和IκB的基因表达水平发生显著变化,表明NF-κB通路被激活。此外,我们发现HRZ组中NF-κB的表达水平先升高后略有下降。有研究表明,RFP的免疫调节作用可抑制NF-κB活化并减少促炎因子的产生[13,14]。此外,用PZA处理的人单核细胞和小鼠可抑制NF-κB的活化[15,16]。因此,我们可以推测HRZ组中INH通过诱导氧化应激然后激活NF-κB途径来诱导肝损伤。而RFP和PZA可以引起肝毒性并诱导氧化应激诱导NF-κB活化,但同时也可能发挥免疫调节作用来抑制NF-κB活化,但具体机制有待进一步探索。
总之,我们的结果表明,NF-κB通路在一线抗结核药物INH、RFP和PZA诱导的小鼠肝损伤中被激活。尽管现代医学迅速发展,但是几乎没有可靠的药物可以保护肝脏不受损害或促进肝细胞再生。因此,终止活化的NF-κB信号通路可能成为未来的研究重点。
参考文献
[1] Li S, Tan HY, Wang N, et al. The Role of Oxidative Stress and Antioxidants in Liver Diseases. Int J Mol Sci. 2015; 16: 26087-26124.
[2] Gupta SC, Sundaram C, Reuter S, Aggarwal BB. Inhibiting NF-kappaB activation by small molecules as a therapeutic strategy. Biochim Biophys Acta. 2010; 1799: 775-787.
[3] Morgan MJ, Liu ZG. Crosstalk of reactive oxygen species and NF-kappaB signaling. Cell Res. 2011; 21: 103-115.
[4] Bakkar N, Guttridge DC. NF-kappaB signaling: a tale of two pathways in skeletal myogenesis. Physiol Rev. 2010; 90: 495-511.
[5] Liu B, Sun L, Liu Q, et al. A cytoplasmic NF-kappaB interacting long noncoding RNA blocks IkappaB phosphorylation and suppresses breast cancer metastasis. Cancer Cell. 2015; 27: 370-381.
[6] Wang M, Shen G, Xu L, et al. IL-1 receptor like 1 protects against alcoholic liver injury by limiting NF-kappaB activation in hepatic macrophages. J Hepatol. 2017.
[7] Miglani S, Patyar RR, Patyar S, Reshi MR. Effect of goat milk on hepatotoxicity induced by antitubercular drugs in rats. J Food Drug Anal. 2016; 24: 716-721.
[8] Rao P, Hayden MS, Long M, et al. IkappaBbeta acts to inhibit and activate gene expression during the inflammatory response. Nature. 2010; 466: 1115-1119.
[9] Chen S, Maini R, Bai X, Nangreave RC, Dedkova LM, Hecht SM. Incorporation of Phosphorylated Tyrosine into Proteins: In Vitro Translation and Study of Phosphorylated IkappaB-alpha and Its Interaction with NF-kappaB. J Am Chem Soc. 2017; 139: 14098-14108.
[10] Zuo T, Zhu M, Xu W, Wang Z, Song H. Iridoids with Genipin Stem Nucleus Inhibit Lipopolysaccharide-Induced Inflammation and Oxidative Stress by Blocking the NF-kappaB Pathway in Polycystic Ovary Syndrome. Cell Physiol Biochem. 2017; 43: 1855-1865.
[11] Kastl L, Sauer SW, Ruppert T, et al. TNF-alpha mediates mitochondrial uncoupling and enhances ROS-dependent cell migration via NF-kappaB activation in liver cells. FEBS Lett. 2014; 588: 175-183.
[12] Lian YH, Fang J, Zhou HD, Jiang HF, Xie KJ. Sufentanil Preconditioning Protects Against Hepatic Ischemia-Reperfusion Injury by Suppressing Inflammation. Med Sci Monit. 2019; 25: 2265-2273.
[13] Wang X, Grace PM, Pham MN, et al. Rifampin inhibits Toll-like receptor 4 signaling by targeting myeloid differentiation protein 2 and attenuates neuropathic pain. FASEB J. 2013; 27: 2713-2722.
[14] Zhu L, Kang H, Guo CA, et al. Rifampin suppresses osteoclastogenesis and titanium particle-induced osteolysis via modulating RANKL signaling pathways. Biochem Biophys Res Commun. 2017; 484: 64-70.
[15] Manca C, Koo MS, Peixoto B, Fallows D, Kaplan G, Subbian S. Host targeted activity of pyrazinamide in Mycobacterium tuberculosis infection. PLoS One. 2013; 8: e74082.
[16] Sakala IG, Eickhoff CS, Blazevic A, Moheno P, Silver RF, Hoft DF. Dipterinyl calcium pentahydrate inhibits intracellular mycobacterial growth in human monocytes via the C-C chemokine MIP-1beta and nitric oxide. Infect Immun. 2013; 81: 1974-1983.
[2020-01-07收稿]