Nasal mucosa pyoderma vegetans associated with ulcerative colitis:A case report
2020-04-08ShuXiaYuXianKuiChengBinLiJingHuaHao
Shu-Xia Yu, Xian-Kui Cheng, Bin Li, Jing-Hua Hao
Shu-Xia Yu, Bin Li, Jing-Hua Hao, Department of Gastroenterology and Hepatology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan 250021, Shandong Province, China
Xian-Kui Cheng, Department of Pathology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan 250021, Shandong Province, China
Abstract BACKGROUND Pyoderma vegetans (PV) is not a common extra-intestinal manifestation of ulcerative colitis (UC), while nasal mucosa PV associated with UC is particularly rare.CASE SUMMARY We report a 28-year-old female with a history of UC and pyoderma gangrenosum who presented with nasal pain. A nasal lesion could be observed in her nose, and histopathological examination was indicative of PV. The patient was treated with oral prednisone (40 mg per day) with good response and became symptomatically free. There was no recurrent attack after 1 year of follow-up.CONCLUSION Inflammatory bowel disease patients presenting with nasal pain should be further investigated to rule out the coexistence of nasal mucosa PV.
Key Words: Pyoderma vegetans; Extra-intestinal manifestations; Ulcerative colitis; Nasal lesion; Case report
INTRODUCTION
Pyoderma vegetans (PV) is not a common extra-intestinal manifestation of ulcerative colitis (UC), while nasal mucosa PV associated with UC is particularly rare. We present herein a rare case of PV with nasal pain that evolved in a patient with UC.
CASE PRESENTATION
Chief complaints
A 28-year-old female presented to the hospital in January 2018 for the first time. She complained of six to seven bowel movements per day with pus and blood for 1 mo.Associated symptoms included cramping abdominal pain before bowel movements,nausea, anorexia, and a 3 kg weight loss. She had no fevers or night sweats.
History of present illness
Colonoscopy was performed, and she was diagnosed as UC limited to her left colon with a Mayo endoscopic subscore of 3 (severe disease, Figure 1). With treatment of mesalazine for 10 d, she was improving but developed skin lesions on her legs and right inguinal region, which appeared as skin pustules and then became burrowing ulcers between 2 cm and 10 cm in diameter. The skin lesions were finally diagnosed as pyoderma gangrenosum (Figure 2) by histology.
History of past illness
She had a history of hemorrhoids for more than 10 years. She had no family history of cancers or inflammatory bowel disease.
Laboratory examinations
On admission, laboratory investigations revealed a drop in hemoglobin to 73 g/L and increases in C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin to 63.38 mg/L, 61 mm/h, and 249.05 μg/g, respectively. The patient had a very low albumin at 22.2 g/L. Stool studies revealed numerous leukocytes and red blood cells but were negative for infectious etiology, includingClostridium difficile.
Medical management
The patient was then started on intravenous methylprednisolone. Daily medications with fibroblast growth factor gel and sodium fusidate ointment were also given to the patient for the treatment of pyoderma gangrenosum. At 1 wk after the steroid treatment, a clear improvement of the cutaneous lesions was observed with downtrending C-reactive protein and erythrocyte sedimentation rate. The patient was hereby transitioned to oral prednisone and discharged home.
One year later, the patient returned to the hospital and reported compliance with oral mesalamine and had been doing well since tapering off steroids 3 mo prior. At 1 wk before admission, she had defecation with mild bleeding two to three times daily and had severe nasal pain. She had no fever or abdominal pain. On physical examination, her vital signs were within the normal range. The only remarkable findings were old skin scars on her extremities. A colonoscopy was performed and revealed mild-to-moderate left-sided colitis consistent with a Mayo endoscopic subscore of 2, which was improved from her previous colonoscopy in May 2018.
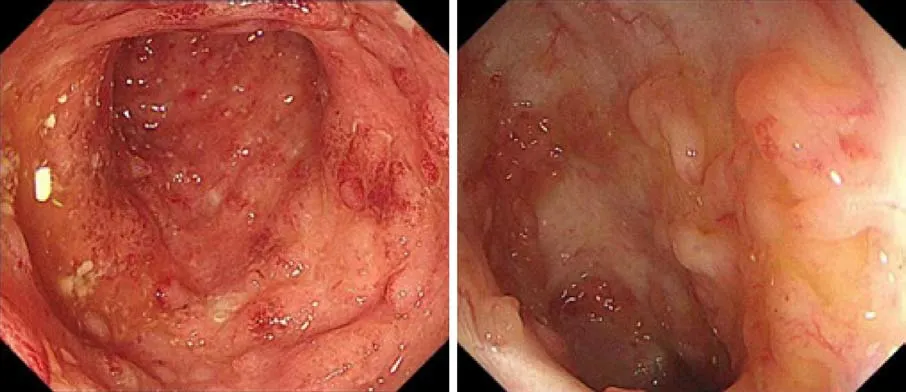
Figure 1 Colonoscopy showed severe ulcerative colitis.

Figure 2 Skin lesions on the legs.
She was then referred to an otolaryngologist. Her nasal mucosa was hyperemic, and nasal septum mucosa was remarkably thickened (Figure 3). Biopsies from left nasal septum mucosa revealed plasma cell and eosinophils infiltration, some neutrophil and lymphocyte infiltration, interstitial edema of mucosa, and fibrocyte and fibroblast hyperplasia (Figure 4). Based on the clinical and pathological findings, the patient was diagnosed with PV.
FINAL DIAGNOSIS
The final diagnosis of this case is nasal mucosa PV.
TREATMENT
The patient was hereby given oral prednisone (40 mg/d).
OUTCOME AND FOLLOW-UP
The bowel movements of this patient became normal in 1 wk. Notably, her nasal pain disappeared quickly. The patient was recovered from PG, and the skin lesions completely cleared after steroid treatment. Steroids were tapered off in 4 mo, and there were no recurrent attacks after 1 year of follow-up.

Figure 3 The patient’s nasal mucosa was hyperemic and nasal septum mucosa became remarkably thickened.
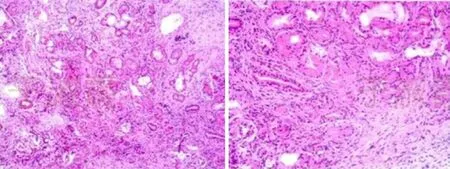
Figure 4 Photomicrograph of hematoxylin and eosin stain (× 20) showing plasma cell and eosinophil infiltration, some neutrophil and lymphocyte infiltration, interstitial edema of mucosa, and fibrocyte and fibroblast hyperplasia.
DISCUSSION
Extra-intestinal manifestations (EIMs) in patients with inflammatory bowel disease(IBD) are quite common. The organs most commonly involved are the skin, joints, the biliary tract, and the eyes. A Swiss IBD Cohort Study showed that 31% of UC patients developed EIMs, such as arthritis, uveitis, pyoderma gangrenosum, erythema nodosum, aphthous stomatitis, ankylosing spondylitis, primary scleroscholangitis,etc[1].
PV is a rare benign cutaneous, chronic, inflammatory, pustular condition clinically characterized by raised, erythematous, exudative, vegetating plaques. This disease of unknown etiology is often associated with bacterial infections in immunocompromised patients[2]. The association of PV and UC has rarely been reported in the literature[3].
Nearly one quarter of EIM affected IBD patients suffers from a combination of several EIM. More than one organ involved may suggest a common pathogenic pathway[4]. However, the underlying mechanisms are not completely understood yet.As for this patient, PG was first diagnosed in her legs and right inguinal region, and her nasal mucosa subsequently suffered from PV. Till now, there is only one case report of nasal mucosa PVs in a patient with UC[5].
PV can heal spontaneously but usually recurs and becomes chronic. There are no standard treatment modalities. Systemic steroids and local wound care could control the disease[6]. Considering the patient had severe UC accompanied with EIM, we suggested using infliximab, which is an appropriate option for the patient who does not respond to routine treatments. However, the patient refused the infliximab treatment due to the expensive cost. Finally, the patient got improved with the treatment of systemic steroids. Luckily, she had no recurrent attacks after 1 year of follow-up.
CONCLUSION
This case highlights that IBD patients presenting with nasal pain should be further investigated to rule out the coexistence of nasal mucosa PV.
杂志排行
World Journal of Clinical Cases的其它文章
- Relationship between non-alcoholic fatty liver disease and coronary heart disease
- Remission of hepatotoxicity in chronic pulmonary aspergillosis patients after lowering trough concentration of voriconazole
- Endoscopic submucosal dissection as alternative to surgery for complicated gastric heterotopic pancreas
- Observation of the effects of three methods for reducing perineal swelling in children with developmental hip dislocation
- Predictive value of serum cystatin C for risk of mortality in severe and critically ill patients with COVID-19
- Sleep quality of patients with postoperative glioma at home