Relationship between non-alcoholic fatty liver disease and coronary heart disease
2020-04-08UgurArslanMustafaYener
Ugur Arslan, Mustafa Yenerçağ
Ugur Arslan, Mustafa Yenerçağ, Department of Cardiology, University of Health Sciences Samsun Training and Research Hospital, Samsun 55400, Turkey
Abstract Non-alcoholic fatty liver disease (NAFLD) is the leading cause of chronic liver disease and considered a liver manifestation of metabolic syndrome. It is in close relationship with insulin resistance, obesity, diabetes mellitus, all of which increase risk of cardiovascular disease (CVD). Besides, many studies point out that NAFLD independently contributes to the development of atherosclerosis and CHD. On the other hand, CVDs are the leading cause of death in NAFLD patients.Many pathophysiological changes and molecular mechanisms play an important role in NAFLD for CVD formation. Atherosclerosis is common in NAFLD, which also mainly contributes to the CVD formation and CHD. Many studies linking atherosclerotic CHD and NAFLD are present in the literature. Subclinical CHD,mainly detected by coronary computed tomography views, have been detected more common in NAFLD patients. Presence of NAFLD has been found to be more common in patients with severe CHD and in stable CHD, NAFLD has been found to be associated with more diffuse disease. In acute coronary syndromes,especially in acute myocardial infarction, patients with NAFLD have been found to have poor prognosis when compared with NAFLD free patients. In this review,our aim is to evaluate the relationship between NAFLD and CHD in detail and go over the pathophysiological mechanisms underlying this relationship.
Key Words: Fatty liver; Hepatosteatosis; Coronary heart disease; Atherosclerosis;Cardiovascular; Artery
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) has an increasing prevalence in concordance with the increasing prevalence of diabetes mellitus and obesity and cardiovascular disease (CVD) is an important cause of mortality in NAFLD[1]. NAFLD is commonly considered as the hepatic expression of metabolic syndrome (MS)manifested by insulin resistance and endothelial dysfunction, both of the latter take place in the pathogenesis and complications due to diabetes mellitus and obesity.NAFLD has been also found to be associated with hypertension and dyslipidemia,which are counted as two of the five components of MS[2].
NAFLD as a systemic disorder is associated with other chronic diseases including diabetes mellitus and chronic renal disease, but the most important association is between NAFLD and CVDs, especially CHD, because the most common cause of death in this disorder is due to cardiovascular diseases. NAFLD may also be considered as an individual risk factor for CVDs because in several clinical studies, it has been found to be independently associated with CVDs after the effects other traditional risk factors and components of MS have been eliminated.
In this review, we have overviewed the molecular mechanisms and clinical conditions linking NAFLD with CHD.
NAFLD DEFINITION AND EPIDEMIOLOGY
NAFLD is a general term including different degrees of liver damage,i.e.simple steatosis to cirrhosis. The pathological picture is similar to alcohol-induced liver damage and hepatic accumulation of triglyceride (TG) in combination with steatohepatitis characterizes the findings in NAFLD. NAFLD is known as the most common chronic liver disease with a prevalence of 10%-24% in different series. Its prevalence increases with age and is higher in males than females[2,3].
The diagnosis of NAFLD relies on 4 criteria: (1) Hepatic steatosis should be found with different imaging modalities or directly with tissue biopsy; (2) Alcohol consumption should not be present in significant amounts; (3) Other etiologic factors causing NAFLD should be absent; and (4) Other accompanying causes of chronic liver disease should not be found. NAFLD severity is designated by degree of fibrosis and existence of steatohepatitis; diagnosis of which requires at least 5% hepatic steatosis with hepatocyte injury and inflammation. Categorization of fibrosis can be made from stage 1 with limited hepatic involvement to stage 4 known as cirrhosis. Although gold standard method for diagnosis of NAFLD is liver biopsy, non-invasive imaging methods like computed tomography, ultrasonography, and magnetic resonance imaging can be used safer and less costly, with good sensitivity and specificity[2,4]
Increasing evidence suggests that NAFLD is not only a potentially progressive liver disease, but also has systemic consequences. A sedentary lifestyle and poor eating habits are the main reason for the increase in prevalence, along with many metabolic diseases. The prevalence in obese people rises to 57.5%-74%[5]. The prevalence in patients with type-2 diabetes mellitus varies between 50%-75%[6]. In addition, NAFLD is considered the hepatic manifestation of metabolic syndrome (MS)[7]. NAFLD is closely associated with all features of MS, abdominal obesity, atherogenic dyslipidemia, hypertension, insulin resistance and impaired glucose tolerance. At least one of the components of MS can be found in 90% of patients with NAFLD and about one third of NAFLD patients meet the complete diagnostic criteria for MS, therefore NAFLD may be counted as the hepatic representation of MS[7,8]. As a result, NAFLD is closely related to the multiple potential risk factors of cardiovascular diseases and thought to be an independent risk factor for CVD and events.
NAFLD AND CARDIOVASCULAR DISEASES
It should be noted that both NAFLD and CVD share similar risk factors such as diabetes mellitus, dyslipidemia, and obesity. Therefore, it may be thought that both diseases develop simultaneously and NAFLD may seem to be a by-stander during the development of CVD. However, the fact is different. Despite scarce number of studies in the literature, many studies point out that NAFLD independently contributes to the development of atherosclerosis and CHD.
Many studies show that NAFLD is associated with subclinical [increased carotid intima-media thickness, coronary calcium score (CAC), abdominal aortic calcification(AAC), endothelial dysfunction and arterial stiffness] and clinical cardiovascular diseases (coronary artery disease, acute coronary syndrome, ischemic stroke) most of which are associated with atherosclerosis[9]. Complex and heterogeneous mechanisms which have not been completely elucidated take place in the causal relationship between NAFLD and cardiovascular diseases and they include different functional interactions of many systems at the same time. Genetics, insulin resistance, adipose tissue dysfunction, dyslipidemia, oxidative stress, inflammation and endothelial dysfunction are the most important connection points between NAFLD and cardiovascular diseases. These links may explain the relationship between the liver disease and cardio-metabolic complications[4].
Many meta-analyzes which strengthen the relationship between NAFLD and CV events have been conducted. In a meta-analysis of 34043 individuals from 16 studies,NAFLD patients have been shown to be more affected by cardiovascular events. In addition, 6 studies showed a higher increase in CV event risk in patients with higher NAFLD severity[10]. In their meta-analysis, Mahfood Haddadet al[11]found that the risk of clinical cardiovascular events in NAFLD patients was significantly higher than those withoutin 25867 patients. In another meta-analysis of approximately 165000 participants from 34 studies, NAFLD has been found to be associated with an increased risk of cardiovascular events and CVDs. Severity of illness appears to be associated with an increase in cardiovascular events[12]. These studies show an association between increased cardiovascular events, especially for severe NAFLD patients. While it has been shown that NAFLD may be associated with increased cardiovascular mortality in meta-analyses showing the relationship with cardiovascular mortality[13,14], this relationship has not been shown in a few of them[15,16]. This relationship is less pronounced in these meta-analyses, especially since there are discordant studies used in these ones. Accordingly, it is recommended that early intervention is necessary in NAFLD patients to reduce the risk of progression of the disease and improve the cardiovascular outcomes due to increased cardiovascular risk.
NAFLD AND ATHEROSCLEROSIS
Atherosclerosis (AS), known as the most common etiologic factor for CVD, is defined as a pathological plaque formation within blood vessels that initiates intimal thickening the earliest lesion in the arterial wall[17], hardening of the arteries, and narrowing of the lumen. According to the modified classification of the American heart association, many phenotypes of AS disease have been demonstrated[18,19].Classification includes intimal xanthoma, pathological intimal thickening, fibrocalcific plate, fine-fiber valve atheroma, and fibroadenoma. The best pathophysiology of AS is hypertension, dyslipidemia,etc.It is defined by the "endothelial damage theory",which shows that components of AS induce vascular intimal damage. In addition, AS is associated with many inflammatory cells and a systematic chronic inflammation[20].
NAFLD is closely related to many metabolic conditions that expose an increased risk of CV disease. Studies have also shown that an independent relationship between NAFLD and CVD is found when other metabolic risk factors for CVD are also counted in[21]. Therefore, NAFLD may be thought to contribute actively to the pathogenesis of AS besides its role as a marker for CVD[9]. Therefore, NAFLD is closely associated with AS and appears to be an early risk factor for AS. The high prevalence of NAFLD in patients with AS have made physicians get interested in the possible pathophysiologic role of the fatty liver in AS development.
Insulin resistance, defined as "first-hit" to the liver, disrupts cellular energy metabolism and damages peripheral tissues. The liver interferes with the reuptake and synthesis of fatty acid, causing its accumulation in liver, leading to insulin resistance,as the endogenous liver glucose production is not suppressed[22]. NAFLD patients develop hyperglycemia, hyperinsulinemia, hyperlipidemia and damage to vascular endothelial cells due to insulin resistance. It can also cause the proliferation of smooth muscle cells (SMCs). Therefore, insulin resistance contributes to the development of both NAFLD and AS.
Dilation and dysfunction of adipose tissue have an important place in cardiovascular complications. When overeating and excessive calorie intake exceed the expansion and storage capacity of adipose tissue, serum levels of free fatty acids (FFA)increase, and ectopic fat deposits form in the liver and other organs. NAFLD is associated with dyslipidemia, given that lipid intake, synthesis and regulation of metabolism are impaired in the liver of NAFLD patients due to enlarged fat mass. In NAFLD, low-density lipoprotein (LDL) receptors are down-regulated resulting in cholesterol uptake and very low-density lipoprotein synthesis in liver, causing an increase in TG[23]. Elevated TG levels may further impair the lipid profile by decreasing high-density lipoprotein cholesterol and increasing small and dense LDL particles and oxidized LDL[24]. In addition, as blood FFA levels increase due to increased energy intake and decreased FFA oxidation, it can be morphologically affected by interendothelial cell dilatation[25]. These changes directly contribute to AS and accelerate local atherosclerotic development.
As a "second hit" to the liver in NAFLD development, lipid peroxidation and oxidative stress may indicate the relationship between NAFLD and AS. Oxidative stress is a condition in which the body's reactive oxygen type (ROS) production is above ROS detoxification and causes tissue damage[26]. Increasing asymmetric dimethyl arginine levels in NAFLD, as an endogenous antagonist of nitric oxide synthase, results in a decrease in NO level. In addition, the formation of an inflammatory environment increases NO consumption and inhibits endotheliumdependent vasodilation, decreases the blood vessels elasticity, destroys the apoptosis of endothelial cells, promotes hyperplasia of vascular smooth muscle cells, contributes macrophages apoptosis in the atherosclerotic plaque and induces oxidized LDL through lipid peroxidation[19].
As a result of inflammation in NAFLD patients, levels of tumor necrosis factor-α,interleukin (IL)-6, monocyte chemoattractant protein-1 and C-reactive protein which were all known to be associated with AS, increase. Elevated expression of IL-6 in liver cells and elevated IL-6 in blood may increase partial liver damage and AS[27]. The insulin resistance that occurs with this systemic inflammation contributes to the development of AS. In addition, an elevation of matrix metalloproteinase levels has been also found in NAFLD[28], and this elevation may play a critical role in AS process by promoting sensitive atherosclerotic plaque formation.
The adipocytes secrete a molecule called adiponectin which increases insulin sensitivity in liver and other tissues to decrease serum fatty acid levels and increase fatty acid oxidation in muscle[29]. Adiponectin can reduce TG, total cholesterol and LDL-C concentrations[30], and it can stimulate vascular endothelial nitric oxide synthase and gradually reduce atherosclerotic lesions. Adiponectin levels were found to be low in NAFLD patients[31]. Produced mostly by adipose tissue, leptin plays a critical role in energy consumption and food intake. It is closely related to insulin resistance and shows a synergistic effect. Leptin was found to be higher in NAFLD patients in relation to disease severity[32]. Visfatin, a new adipocytokin expressed by visceral adipose tissue activity, is related with certain risk factors of AS including endothelial dysfunction, vascular endothelial proliferation, inflammation, and atherosclerotic plaque formation. Visfatin is thought to be related to the atherosclerotic process in NAFLD since it is closely related to the degree of NAFLD and increases in the foamy macrophages of AS plaques[19]. Resistin promotes SMC proliferation,enhances the migration capability of SMCs and induces inflammatory reaction under oxidative stress and dyslipidemia[33]. Therefore, resistin is also associated with NAFLD and functions as an indicator of AS severity.
The intestinal microbiota has been shown to be a risk factor contributing to the development of NAFLD[34]. The levels of lipopolysaccharide derived from the intestinal microbiota are increased in NAFLD patients and it shows endotoxic effects.When plasma endotoxin concentrations increase in the portal vein, this causes systemic endotoxemia and mild chronic inflammation[35]. Obese individuals develop an increased endotoxin load in the portal vein. Therefore, intestinal microorganisms may contribute to AS by indirect ways in patients with NAFLD.
Genetic factors associated with NAFLD's cardiovascular events are still undefined.PNPLA3 and transmembrane 6 superfamily 2 genes are related to lipid metabolism in the liver and atherogenic dyslipidemia has been associated in NAFLD patients[36,37].These genes may also contribute to the formation of AS.
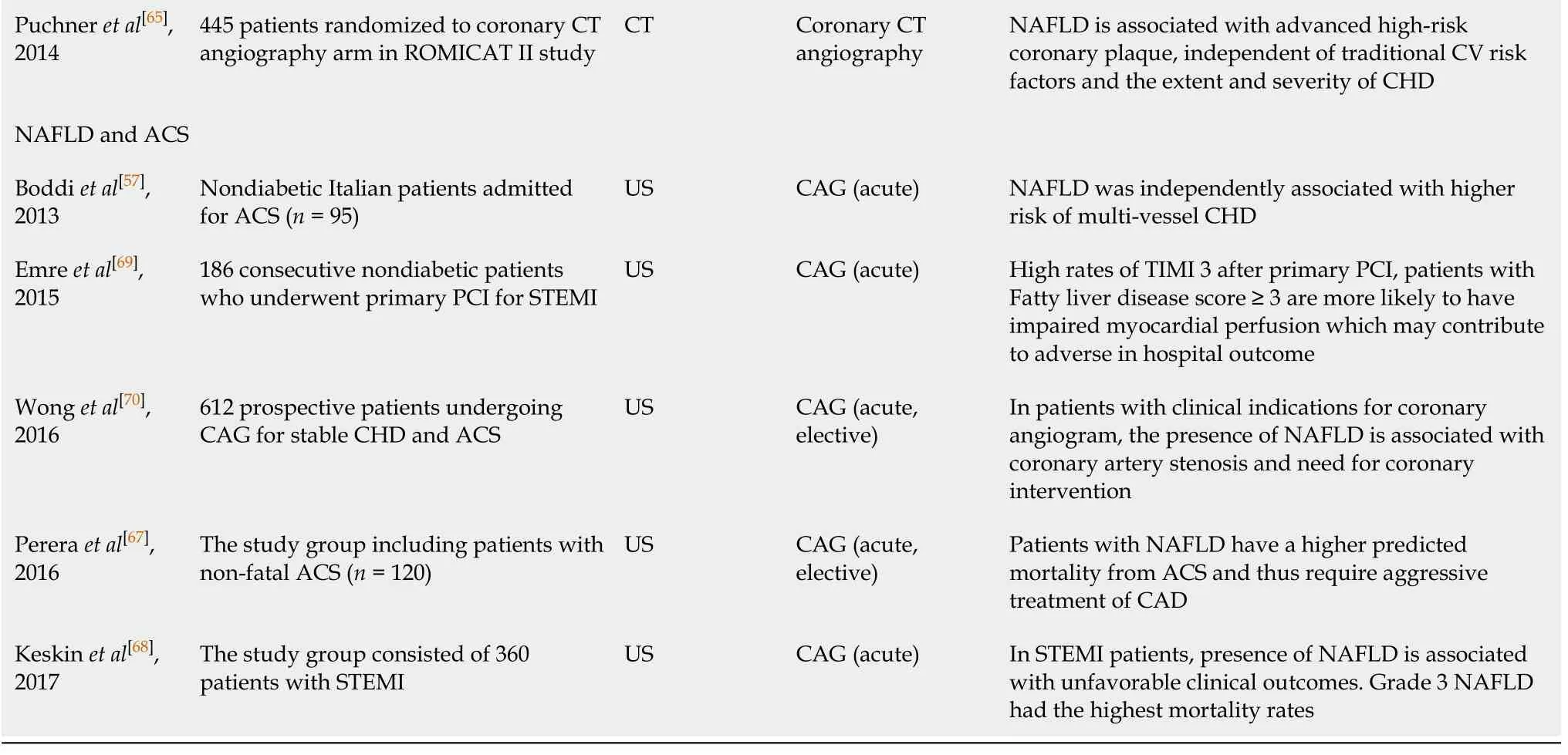
As a result, NAFLD is highly associated with cardio-metabolic syndromes and it is also highly related to AS. Pathophysiological changes occur in NAFLD patients, which predispose to AS formation. Clinical studies have shown the relationship between atherosclerotic cardiovascular diseases and NAFLD. NAFLD is closely related to carotid intima-media thickening, coronary artery atherosclerosis, and increased arterial stiffness[38]. Potential pathophysiological mechanisms responsible for increased CVD in NAFLD are shown in Figure 1.
NAFLD AND CORONARY HEART DISEASE
It is increasingly accepted that NAFLD and CHD are closely related, because presence of NAFLD may be an important risk factor for CHD development. NAFLD is closely related to CAC and the formation of risky coronary artery plaques. Cross-sectional studies examining the relationship between NAFLD and the presence and severity of CHD are shown in Table 1.
CAC which can be detected by multi-slice computed tomography (CT) is an important marker of subclinical CHD[39]. CAC represents the atherosclerotic load on the arterial wall, and there is a significant correlation between the presence of CHD and increased CV poor results[40]. In the study conducted by Sunget al[41],the CAC score measured with CT was independently associated with NAFLD. In a study of 3529 patients undergoing CT imaging showed that NAFLD was found to be related with subclinical markers of atherosclerosis, including calcium deposits in coronary arteries, independent from other metabolic risk factors[42]. In Table 1, other studies which investigate the relationship between CAC and NAFLD are summarized[43-51].
NAFLD has been shown to be associated with higher CHD prevalence regardless of other traditional risk factors[52]. In a prospective cohort study of 2088 adults, NAFLD was found to be significantly associated with CHD prevalence independent of other risk factors[53]. There is a strong correlation between CHD detected by continuously developing imaging methods and increasing NAFLD prevalence[40]. Both NAFLD and CHD share common risk factors and considering the increasing prevalence of obesity,metabolic syndrome and diabetes mellitus, it is possible that the prevalence of both diseases increase in parallel to each other, but, as we have already mentioned, many studies disclosed that NAFLD might be an independent risk factor the development of CHD.
NAFLD patients have an accelerated atherosclerotic process. Genetic susceptibility,insulin resistance, atherogenic dyslipidemia, oxidative stress, systemic inflammation,decreased adiponectin level, and procoagulant factors contribute to the acceleration of the atherosclerotic process. In their study, Wonget al[54]found more NAFLD in patients who underwent coronary angiography and who had significant coronary artery stenosis. Assyet al[53]found higher CHD in NAFLD patients compared to the control group in their study. Arslanet al[55]found the existence of NAFLD to be independently related to the presence of CHD in their study. Those studies indicate that NAFLD patients have an increased risk for atherosclerotic CHD.
NAFLD may also increase CHD severity. In a prospective study, it has been found that NAFLD is an independent risk factor affecting CHD severity[56]. In the study conducted by Boddiet al[57], it has been shown that the risk of moderate to severe NAFLD is closely associated with development of multi-vessel atherosclerosis. In their study, Wonget al[54]showed that NAFLD is associated with greater severity of angiographic CHD, independent of other CVD risk factors. Uncontrolled risk factors,insulin resistance and accelerated atherogenesis, already present in NAFLD patients,may all contribute to widespread plaque formation in coronary arteries and to more serious coronary artery stenosis. In Table 1, studies investigating the relationship between stable CHD and NAFLD have been summarized[54-65].
Another aspect of CHD is acute coronary syndromes (ACS). Several studies have been performed in the literature which investigated NAFLD in ACS[57,66-70]especially in acute myocardial infarction (AMI). In a study, AMI has been associated with significant cardiovascular mortality in NAFLD patients[66]. Pereraet al[67]showed that NAFLD patients had higher mortality when they experienced AMI. In their study,Keskinet al[68]demonstrated that the presence of NAFLD among ST segment elevation myocardial infarction patients had an independent effect on CHD severity and inhospital and long-term mortality. Emreet al[69]showed in their study that the presenceof NAFLD in non-diabetic ST segment elevation myocardial infarction patients may have abnormal myocardial perfusion and increase in-hospital major adverse cardiac events rates. These studies demonstrate the relationship between NAFLD and ACS development and poor outcomes in this patient group. Table 1 summarizes the studies in which NAFLD and ACS have been studied together. Disruption of microvascular circulation, increased inflammatory endothelial dysfunction, oxidative stress and prothrombotic environment in NAFLD patients may explain the poor clinical outcomes in AMI patients.
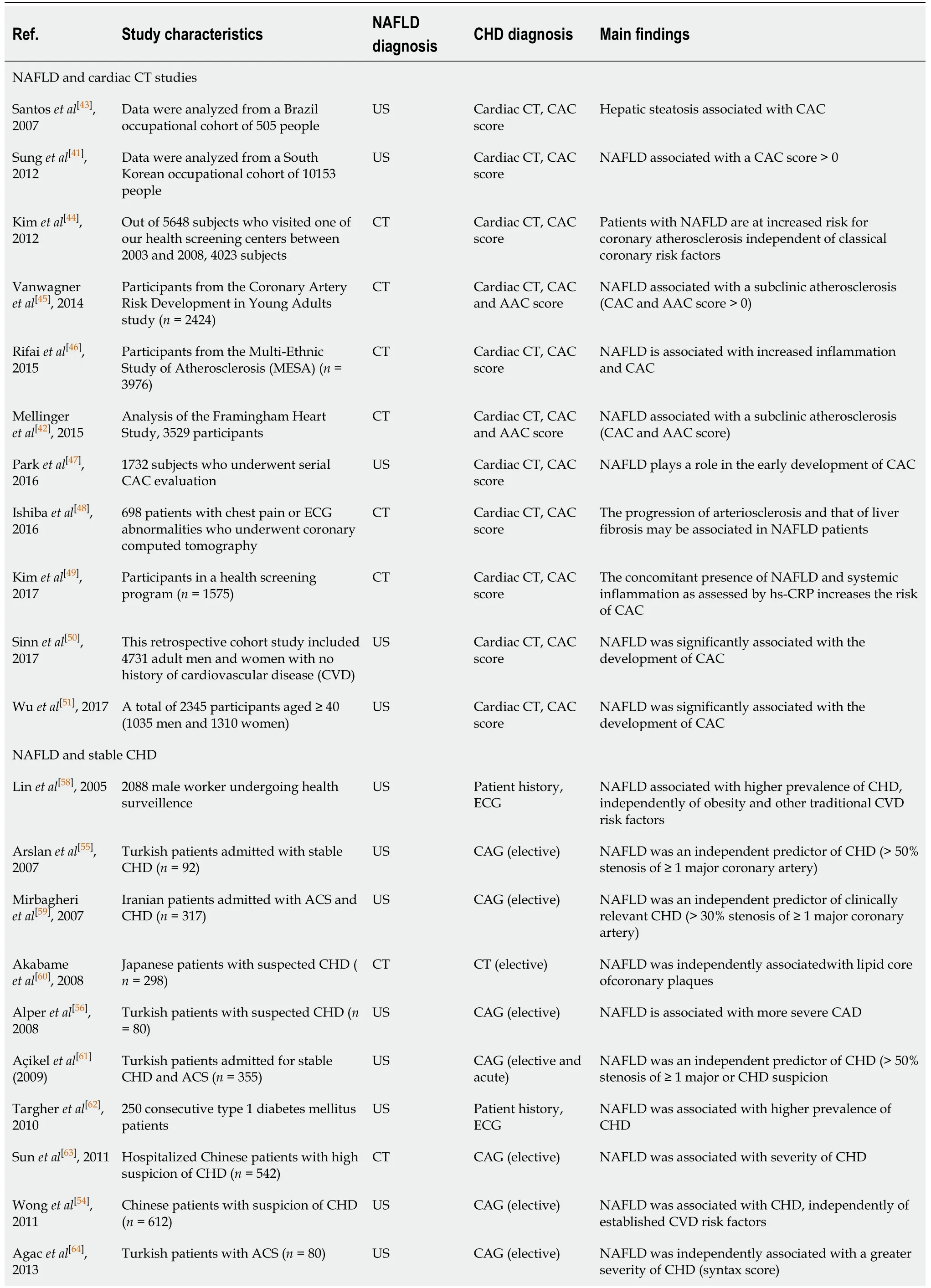
Table 1 Clinical studies examining the relationship between non-alcoholic fatty liver disease and the presence and severity of clinical coronary heart disease
ACS: Acute coronary syndrome; AAC: Abdominal aortic calcification; CAC: Coronary artery calcification; CAG: Coronary angiography; CHD: Coronary heart disease; CT: Computed tomography; DM: Diabetes mellitus; ECG: Electrocardiogram; NAFLD: Non-alcoholic fatty liver disease; PCI: Percutane coronary investigation STEMI: ST segment elevation miyocardial infarction; TIMI: Thrombolysis In myocardial infarction; US: Ultrasonography.
Coronary collateral circulation is an important protective mechanism for myocardial cells in case of an occlusion in any coronary artery such as in acute MI. Collateral development may be affected from several situations. Diabetes mellitus is known to be associated with poor collateral development, whereas severity and duration of CHD is positively correlated with collateralization. Poor collateral development has been also observed in patients with insulin resistance. Arslanet al[71]found that the presence of NAFLD in non-diabetic patients with significant CHD was also independently associated with poor coronary collateralization. This result has been thought to be due to inflammatory cytokine increase in the presence of NAFLD, prothrombotic environment, and endothelial dysfunction resulting from accelerated atherogenesis.Poor collateral circulation in NAFLD may explain the poor prognosis of acute MI patients with this disease.
The significant relationship between NAFLD and CHD has been shown in many studies some of which are discussed in the before-mentioned paragraphs. Many scoring systems are used to predict CVD risk in the general population. The Framingham risk score is a simple and commonly used tool to assess CAD risk level over 10 years. Furthermore, the Framingham risk score has been validated as a predictor of CVD in NAFLD. Since NAFLD patients have an increased risk of CHD,presence of NAFLD may be added to this scoring system for the prediction of CHD.
NAFLD AND CORONARY HEART DISEASE TREATMENT
Lifestyle change consisting of diet, exercise and weight loss plays an important role in the treatment of NAFLD and CAD. In addition to the Mediterranean diet, which is thought to have a beneficial effect on cardio-metabolic risk factors in terms of NAFLD and CAD, a low calorie (1200-1600 kcal/d), low fat (less than 10% of saturated fatty acid), low carbohydrate diet (total kcal of < 50%) is recommended[72]. Aerobic and resistance exercises should be done as physical activity. In particular, European Association for the Study of the Liver[73], National Institute for Health and Care Excellence[74]and American Association for the Study of Liver Diseases[2]guidelines on diet and physical activity propose programs targeting lifestyle changes. According to these guidelines, the goal of most lifestyle changes is a weight loss of 7%-10%.
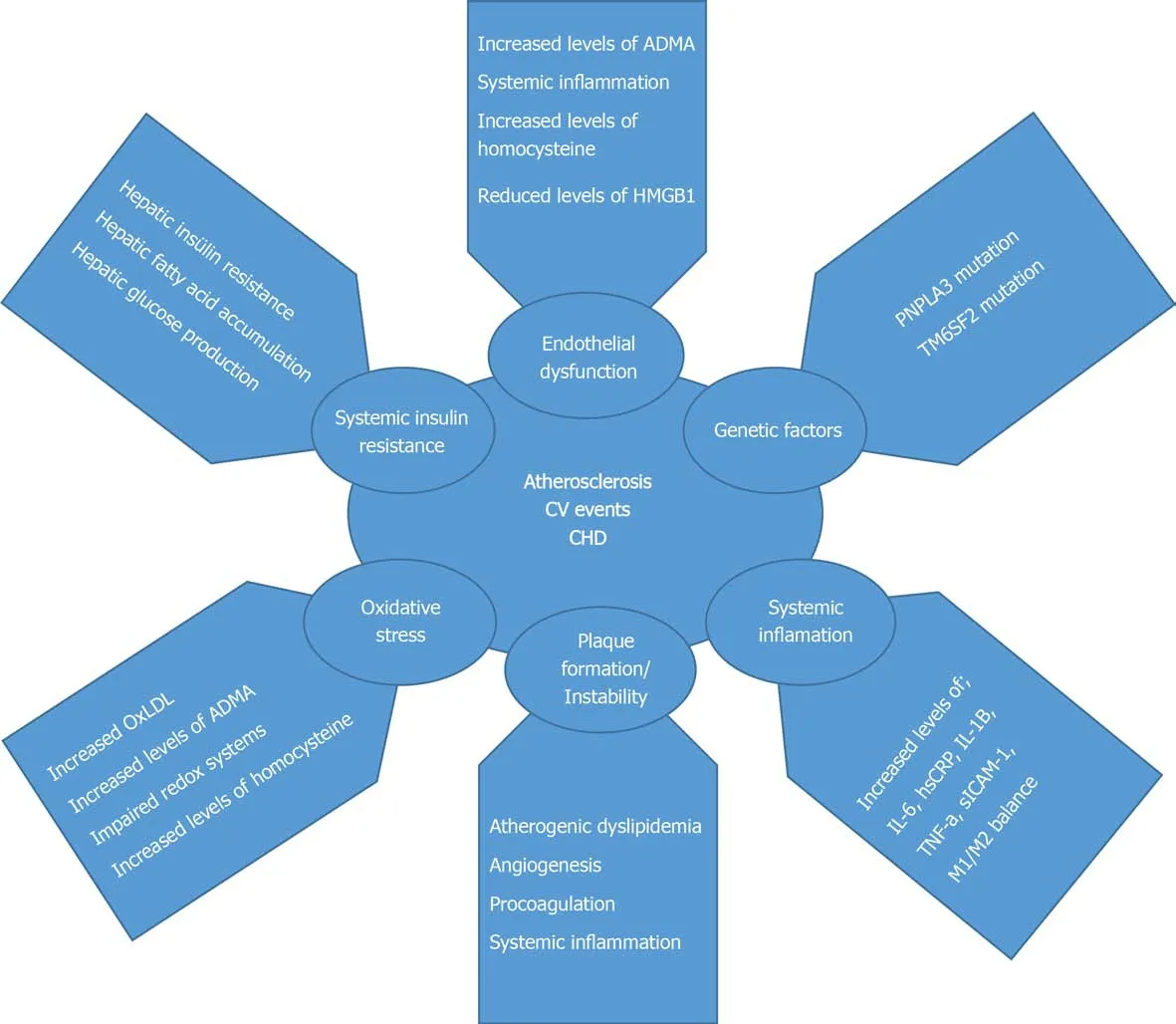
Figure 1 Potential pathophysiological mechanisms responsible for increased cardiovascular disease in non-alcoholic fatty liver disease.CHD: Coronary heart disease; TNF: Tumor necrosis factor; IL: Interleukin; CRP: C-reactive protein.
Insulin sensitizers are pharmacologically important for both NAFLD and CAD treatment. Metformin used in the treatment of type 2 DM has been proven to reduce the risk of hepatocellular carcinoma, but does not improve the histologic changes in liver of NAFLD patients. Currently, metformin is not recommended in the new guidelines specifically for liver disease in NAFLD patients[75]. Pioglitazone, a peroxisome proliferator-activated receptor gamma agonist with insulin sensitizing effects, improves insulin sensitivity, inflammation and steatosis in NAFLD patients and type 2 DM. Since heart failure may accompany in CAD, patients with NAFLD may be considered for type 2 DM treatment after heart failure is ruled out[76].Glucagon-like peptide-1 receptor agonists (exenatide, liraglutide, lixisenatide, and semaglutide) may reduce body weight by reducing appetite due to their hypoglycemic effects[77]. Sodium-glucose transporter 2 inhibitors (empagliposine, dapaglifosine,remoglyphosine etabonate) act with increased glycosuria by blocking renal glucose reabsorption. It has been shown that long-acting Glucagon-like peptide-1 receptor agonists (liraglutide and semaglutide) decrease major adverse cardiovascular events in patients with type 2 DM[78].
Statins are the most commonly used and effective lipid-lowering drugs for primary and secondary prevention of CVD and their use in NAFLD patients has proven safe despite the concerns about them for liver enzyme elevations. In studies, statins have been shown to improve liver enzymes, steatosis, and necroinflammation[79]. Ezetimibe,another lipid-lowering agent that reduces the intestinal uptake of dietary cholesterol,has been also shown to improve the histological findings in NAFLD. The benefits of the statin ezetimibe combination for CVD have been demonstrated[80]. Fibrates, by activating peroxisome proliferator-activated receptor-α, decrease serum TG levels while improving high-density lipoprotein-cholesterol levels simultaneously. However,fibrates have been shown to reduce CVD morbidity and mortality only in atherogenic dyslipidemia. Although fibrates are not demonstrated to improve histologic findings,they offer an effective and safe treatment for atherogenic dyslipidemia in NAFLD patients, particularly MetS and / or Type 2 DM patients[81].
Omega-3 polyunsaturated fatty acids may be also considered to treat hypertriglyceridemia in NAFLD patients. Given the joint role of oxidative stress in the pathogenesis of both NAFLD and atherosclerosis, antioxidants and specific vitamins(Vitamin E) may improve liver histology and reduce the risk of CVD, but their role in treatment of NAFLD and CHD has not been sufficiently proved yet.
CONCLUSION
The prevalence of NAFLD increases with cardiometabolic diseases. Insulin resistance,adipose tissue dysfunction, atherogenic dyslipidemia, oxidative stress, inflammation and endothelial dysfunction in NAFLD are the most important pathophysiological mechanisms in the formation of atherosclerotic CVD. Besides, NAFLD patients have an increased risk of CHD, independent of other traditional cardiovascular diseases.Subclinical and clinical CHDs, either in the acute or chronic settings, have been associated with NAFLD in several studies in the literature. Acute coronary syndromes can result in worse outcome in NAFLD patients. In addition, weaker coronary collateral circulation may be observed in NAFLD patients. Therefore, NAFLD patients should be followed closely for the development of CVDs, especially CHD. Whether medical and non-medical treatment of NAFLD prevents the development of CVD is a debate of question and should be investigated in randomized, prospective, long-term follow-up studies.
杂志排行
World Journal of Clinical Cases的其它文章
- Remission of hepatotoxicity in chronic pulmonary aspergillosis patients after lowering trough concentration of voriconazole
- Endoscopic submucosal dissection as alternative to surgery for complicated gastric heterotopic pancreas
- Observation of the effects of three methods for reducing perineal swelling in children with developmental hip dislocation
- Predictive value of serum cystatin C for risk of mortality in severe and critically ill patients with COVID-19
- Sleep quality of patients with postoperative glioma at home
- Early complications of preoperative external traction fixation in the staged treatment of tibial fractures: A series of 402 cases