Laparoscopic dissection of the hepatic node: The trans lesser omentum approach
2020-01-16OffirBenIshay
Offir Ben-Ishay
Offir Ben-lshay, Department of General Surgery, Rambam Health Care Campus, Haifa 35254,Israel
Abstract
Key words: Lymph node; Diagnosis; Lymphoma; Laparoscopy; Biopsy; Retroperitoneum
INTRODUCTION
Diagnosis of lympho-proliferative diseases is sometimes challenging. Based upon the current international guidelines[1,2], a surgically excised tissue biopsy is widely accepted as the gold standard for the diagnosis of lymphoma. An excisional biopsy of a lymph node (LN) allows assessment of the micro-architecture and provides adequate material for immunocytochemistry, flow cytometry, fluorescencein situhybridization studies, and extraction of DNA and RNA for molecular diagnostics. The major disadvantages of surgical biopsies are the probable need for general anesthesia and deferrals due to the need of a surgical consult and operating room time. These issues are addressed through percutaneous and endoscopic core needle biopsies or fine needle aspiration with cellblock techniques.
When possible, a superficial LN, most often from the groin or axilla, should be excised, and this can be done simply under local anesthesia in day care setup. Often though this is not possible, and an intra-abdominal LN must be obtained.
The intra-abdominal lymphatic system is complex, and lymphadenopathy is often retroperitoneal, along the celiac axis and in the pelvis. Traditionally, laparoscopic biopsies of retroperitoneal or celiac nodes are considered complicated. Lymph nodes that are distributed along the celiac trunk include the root of the left gastric (station 7),the proper hepatic artery (station 8), and the splenic artery (station 9).
The hepatic node is the lymph node lying on the proper hepatic artery right above the neck of the pancreas. This node is quite often enlarged and has an abnormal fluorodeoxyglucose uptake on positron emission tomography (Figure 1).
Approach to the supra-pancreatic area is complex; the current study presents our experience with six patients who underwent laparoscopic excision of the hepatic node(LEBHN) through a trans lesser omentum approach.
MATERIALS AND METHODS
Surgical technique
After general anesthesia was induced, the patient was placed in a lithotomy position,and the operating table was maintained in 20°into the reverse Trendelenburg position. The surgeon was located between the legs of the patient, while the first assistant and the camera operator were placed to the left and the right side of the patient respectively.
After insufflation of the abdomen with CO2through a veres needle, a 10 mm trocar was placed above the umbilicus. The camera was than inserted, and an exploration of the abdomen was performed. A second 10 mm trocar was placed in mid left abdomen,and three 5 mm trocars were placed sub-xifoide, mid right quadrant, and left upper quadrant.
The left lobe of the liver was retracted upwards towards the diaphragm, and the lesser omentum with its pars flaccida was exposed. The pars flaccida was excised, the supra-pancreatic area was exposed, and the hepatic node was then observed (Figure 2A). The peritoneal layer above the hepatic node was carefully dissected with an electric cautery, and the node was than dissected carefully with bipolar energy(Figure 2B).
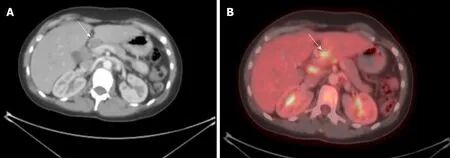
Figure 1 Abnormal FDG uptake on positron emission tomography.
Data collection
Data of all patients undergoing LEBHN over a period of 1 year were collected retrospectively within the array of the surgical oncology service of the Department of general surgery at the Rambam Health Care Campus. Data included demographics,preoperative data including number of previous biopsies, previous biopsy methods used, and operative and post-operative data. Operative and postoperative complications were recorded.
RESULTS
Six patients were operated in this technique during the time frame of the study, 66.6%(n= 4) were females, and the median age was 55 years (25-72). Two patients had a suspected recurrence of a previously treated lymphoma. Three patients had one previous attempt for tissue diagnosis, and one had three of them. One patient had percutaneous attempt for biopsy, four had endoscopic biopsies trough endoscopic ultrasound, and one patient had a mediastinoscopy with mediastinal biopsy. Table 1 depicts the demographic operative and post-operative characteristics of the entire cohort. All patients were operated in a laparoscopic approach with no conversions to laparotomy. All patients had an uneventful operation with no operative or postoperative complications. Mean length of hospital stay was 1 d, and morbidity and mortality were nil.
DISCUSSION
Retroperitoneal lymphadenopathy occurs in various hematologic and granulomatous diseases. Approximately 5% of patients will have abdominal lymphadenopathy without enlargement of LN in superficial areas[4]. Advancements in percutaneous and endoscopic techniques allow diagnosis through minor ambulatory procedures.Laparoscopic abdominal and retroperitoneal lymph node biopsy was previously proven to be feasible and safe in the diagnosis of lympho-proliferative diseases[3-13].Biopsy of celiac nodes or hepatic nodes though has been described occasionally in the literature. The current study describes six patients that underwent a laparoscopic celiac node biopsy in a trans lesser omentum approach. The advantages of this technique over other endoscopic approaches are the high chances for a definitive diagnosis, a better diagnostic yield, and early instigation of treatment.
The approach to the supra-pancreatic area is possible through dissection of the gastro-colic ligament and entrance to the lesser sac, this technique allows full exposure of the pancreas, splenic artery, and hepatic artery. Pisanoet al[4]used this approach in four cases. This technique carried some disadvantages as mobilization of the large curvature of the stomach increases the rate of complications, such as intraoperative hemorrhage and injury to the stomach, and significant increases the operating time.
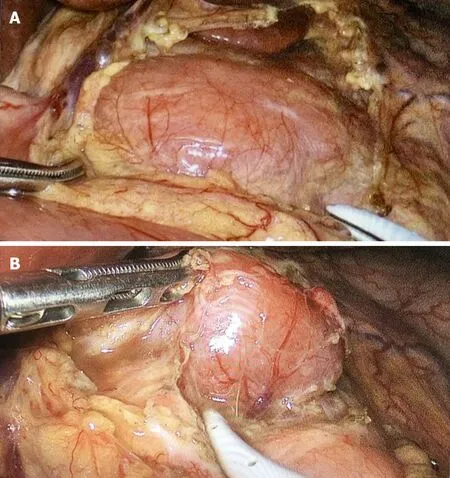
Figure 2 The left lobe of the liver is retracted upwards towards the diaphragm and the lesser omentum with its pars flaccida is exposed.
In our small case series, there were no conversions to laparotomy. The outcomes of operative time, blood loss, and complications were acceptable. All patients received an accurate diagnosis without any false-negative results.
Although the results of this current patient series are good, the small sample size does not permit firm conclusions.
In conclusion, LEBHN seems to be feasible and safe, and surgeons may use this simple approach to a fairly complicated anatomical area to patients who do not have access to superficial lymph nodes.
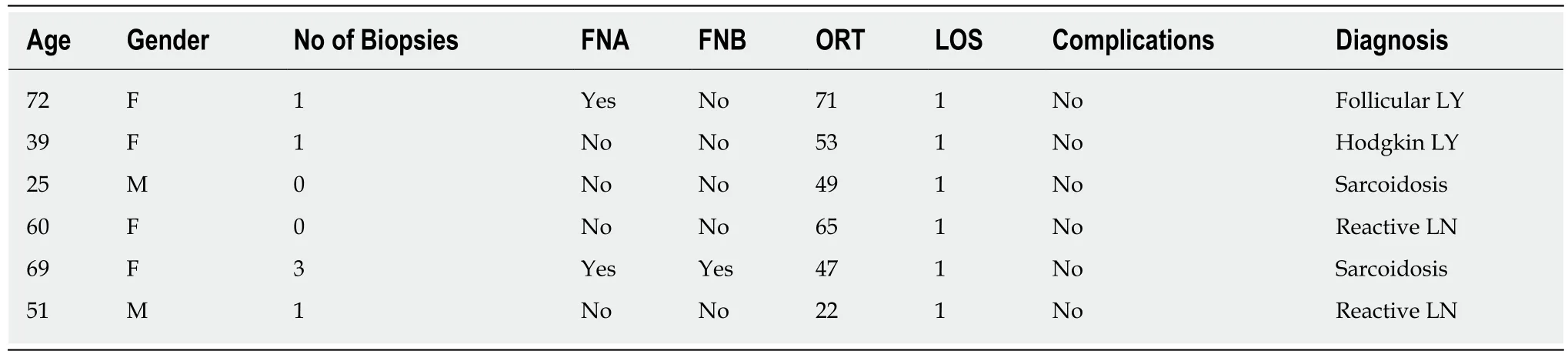
Table 1 Patients’ demographic and operative characteristics
ARTICLE HIGHLIGHTS
Research background
Diagnosis of lympho-proliferative diseases is challenging. Although an excisional biopsy of a complete lymph node is the gold standard for diagnosis, endoscopic or percutaneous techniques are often used due to the surgical challenge the location of the lymph node imposes.
Research motivation
The current study describes a small case series of laparoscopic dissection of the hepatic node through a trans lesser omentum approach. This approach is rarely discussed in the English literature.
Research objectives
The study describes the clinical and surgical results of this novel technique.
Research methods
A single center, retrospective evaluation of patients undergoing laparoscopic dissection and excisional biopsy of the hepatic node.
Research results
During the time frame of the study, six patients were operated using this novel technique, with no conversions to laparotomy, no intra and post-operative complications and acceptable operating time. Most importantly, surgery yielded a definite diagnosis in all patients, and there was no need for further investigation.
Research conclusions
Laparoscopic dissection of the hepatic node seems to be feasible and safe, and surgeons may use this simple approach to a fairly complicated anatomical area in highly selected patients who do not have access to superficial lymph nodes.
Research perspectives
This study suggests that approach to the hepatic node and the celiac axis is easily and safely performed through a trans lesser omentum approach. This may facilitate future discussion on how to achieve the diagnosis of lympho-proliferative disease in patients who do not have enlarged and pathological superficial lymph nodes.
杂志排行
World Journal of Gastrointestinal Oncology的其它文章
- Precision medicine for gastrointestinal cancer: Recent progress and future perspective
- Digestive tract reconstruction options after laparoscopic gastrectomy for gastric cancer
- lnterpretation of the development of neoadjuvant therapy for gastric cancer based on the vicissitudes of the NCCN guidelines
- ldentification of candidate biomarkers correlated with pathogenesis of postoperative peritoneal adhesion by using microarray analysis
- Abnormal CD44 activation of hepatocytes with nonalcoholic fatty accumulation in rat hepatocarcinogenesis
- Multi-institutional retrospective analysis of FOLFlRl in patients with advanced biliary tract cancers
