Application of single balloon enteroscopy-assisted therapeutic endoscopic retrogradecholangiopancreatography in patients after bilioenteric Roux-en-Y anastomosis: Experience of multidisciplinary collaboration
2019-10-28WenGuangWuLuCuiQinXiaoLingSongMingNingZhaoWenJieZhangJunGuHaoWengYingBinLiuYiZhangChunYingQuLeiMingXuXueFengWang
Wen-Guang Wu, Lu-Cui Qin, Xiao-Ling Song, Ming-Ning Zhao, Wen-Jie Zhang, Jun Gu, Hao Weng,Ying-Bin Liu, Yi Zhang, Chun-Ying Qu, Lei-Ming Xu, Xue-Feng Wang
Abstract BACKGROUND Bilioenteric Roux-en-Y anastomosis is one of the most complicated approaches for reconstructing the gastrointestinal tract, and endoscopic retrograde cholangiopancreatography (ERCP) is technically challenging in patients after bilioenteric Roux-en-Y anastomosis. The optimal endoscopic strategies for such cases remain unknown.AIM To explore the feasibility and effectiveness of single balloon enteroscopy-assisted(SBE-assisted) therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis based on multi-disciplinary collaboration between endoscopists and surgeons as well as report the experience from China.METHODS This is a single center retrospective study. All of the SBE-assisted therapeutic ERCP procedures were performed by the collaboration between endoscopists and surgeons. The operation time, success rate, and complication rate were calculated.RESULTS Forty-six patients received a total of 64 SBE-assisted therapeutic ERCP procedures, with successful scope intubation in 60 (93.8%) cases and successful diagnosis in 59 (92.2%). All successfully diagnosed cases received successful therapy. None of the cases had perforation or bleeding during or after operation,and no post-ERCP pancreatitis occurred.CONCLUSION Based on multi-disciplinary collaboration, SBE-assisted therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis is relatively safe and effective and has a high success rate.
Key words: Bilioenteric Roux-en-Y anastomosis; Single balloon enteroscopy; Multidisciplinary cooperation; Hepaticojejunostomy; Pancreaticoduodenectomy
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a clinically important micro-invasive treatment for pancreatobiliary disease. For patients with normal anatomy, the ERCP success rate is generally more than 90%[1]. With the development and advancement of the ERCP technique, ERCP after upper gastrointestinal (GI)surgeries such as Biroth II is now possible and has been performed clinically[2].Bilioenteric Roux-en-Y anastomosis is one of the most complicated approaches for reconstructing the gastrointestinal tract. The change in the gastrointestinal anatomy,absence of the duodenal papilla, and angulation and adhesion of the small intestine,among others, make ERCP after bilioenteric Roux-en-Y anastomosis the most challenging operation. For these reasons, treatment with a conventional side-viewing duodenoscope is very difficult. More recently, single-balloon enteroscopy (SBE) has been used to improve the feasibility of ERCP after bilioenteric Roux-en-Y anastomosis[3-5]. Our center attempted ERCP treatment after re-construction surgery starting in 1998 and has gained some experience[6-9]. With the research at our center,this article aimed to explore the feasibility and effectiveness of SBE-assisted therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis based on multidisciplinary collaboration between endoscopists and surgeons and to report the experience from China.
MATERIALS AND METHODS
Patients
From March 2010 to May 2016, our general surgery department completed 64 cases of SBE-assisted therapeutic ERCP in 46 patients after bilioenteric Roux-en-Y anastomosis. The subjects included 27 males and 19 females with ages ranging from 11 years to 76 years. Their prior operation history included 18 cases of pancreaticoduodenectomy, 25 cases of bilioenteric Roux-en-Y anastomosis, and 1 case of total pancreatectomy. Two cases had undergone two prior operations, including 1 case of Billroth II gastroenterostomy + pancreatico-duodenectomy and 1 case of bilioenteric Roux-en-Y anastomosis + pancreatico-duodenectomy. The indications for ERCP included intrahepatic stones, anastomotic stricture of bilioenteric Roux-en-Y anastomosis, and foreign body remaining at the anastomotic site of a chodedochojejunostomy, among others (Table 1).
Major devices
Olympus CV-260 central unit, SIF-260 small balloon enteroscope (working length 200 cm, outer diameter 9.2 mm, biopsy channel 2.8 mm) and ST-SB 1 single use overtube(working length 132 cm, outer diameter 13.2 mm, internal diameter 11 mm), and OBCU balloon control unit were used. Cotton sphincterotome (COOK, 320 cm length,United States), Glo-Tip ERCP catheter (COOK, 320 cm, United States), Tracer Metro Direct wireguide (COOK, 600 cm length, United States), OASIS stent introducer(COOK, 320 cm length, United States), 5 Fr pushing catheter (COOK, 320 length,United States), Quantum TTC biliary balloon dilator (COOK, 320 cm length, United States), Tri-EX triple lumen balloon extractor (Cook, 275 cm length, United States),and other conventional ERCP devices were also employed.
Operation team task assignment and operating methods
The entire operation team included an endoscopist, a general surgeon, and nurse assistants (Figure 1). Before the operation, all team members got together and reviewed the patient's history, especially the prior history of upper GI surgeries. The general surgeon then drew the scope intubation schema of SBE-assisted ERCP, and all team members studied the drawing (Figure 2). The patient was placed in the prone position with airway intubation general anesthesia. SBE was operated by two operators; the endoscopist worked with the nurse to perform the operation. The process for slowly moving the scope forward included the use of a CO2supply,inflation scope and overtube, deflation and drag movements, which were repeated.During the operation, the general surgeon monitored the X-ray image to determine and guide the scope progress while searching for the bilioenteric Roux-en-Y anastomosis. The general surgeon completed the biliary duct cannulation,anastomosis dilation, stone extraction or biliary stent insertion, and subsequent ERCP operations (Figure 3). During the procedure, the enteroscope maneuver was performed by the endoscopist.
Outcome definitions
Enteroscopy success was defined as accessing the biliary-enteric anastomosis.Diagnostic success was defined as obtaining a cholangiogram. ERCP success was defined as completion of the intended ERCP intervention[10]. ERCP-related adverse events were categorized using the ERCP consensus guidelines[11].
RESULTS
Forty-six patients received a total of 64 SBE-assisted ERCP procedures. Among them,8 patients underwent the procedure twice, 2 patients underwent it 3 times, and 2 patients underwent it 4 times. Of the 64 procedures, 60 had successful endoscopic intubation with a successful scope intubation rate of 93.8%. Additionally, 59 resulted in a successful diagnosis with a successful diagnosis rate of 92.2%. Of all successful scope intubation cases, only 1 case had failure of bile duct cannulation because of anatomic stricture and 59 cases had successful ERCP with an ERCP success rate of 92.2%. All successfully diagnosed cases received successful therapy. None of the cases had perforation, bleeding during or after operation, or acute complications, such as post-operation pancreatitis (Table 2).
DISCUSSION
In terms of a standardized type of ERCP after GI tract surgery for better classification and treatment, there is no current commonly accepted classification method in China or internationally. However, there is a basic consensus on the factors that need to be considered in classifying the type of ERCP after GI tract surgery. They are summarized as follows: (1) The type of GI tract reconstruction[12], from the perspective of surgery, including Billroth I, Billroth II (including Braun anastomosis), total gastrectomy Roux-en-Y anastomosis, pancreaticoduodenectomy (including child anastomosis), and chodedochejejunostomy (Roux-en-Y anastomosis); (2) The presence of the native papilla is closely related to biliary cannulation; (3) Common bile duct stone extraction, biliary stent insertion, chole-dochojejunostomy anatomic stricture dilation, intrahepatic stone extraction, etc.[13]; and (4) Other factors, including the doctor's operation approach and specialty, among others, can have an influence. In other words, the more comprehensive the consideration, the more accurate the classification of factors that affect post-GI surgery ERCP, resulting in a higher success rate.
Our center started performing post-GI surgery ERCP in 1998, and it is one of the earliest centers to explore these techniques and methods in the field. With almost 20 years of experience, our center has established its own characteristics and specialties in post-GI surgery ERCP. From 2009 until now, our center has treated more than 300 cases of GI tract reconstruction, including Billroth I, Billroth II (including Braun), total gastrostomy Roux-en-Y anastomosis, pancreaticoduodenectomy, and choledochojejunostomy, and it is one of the centers with the highest volume of postsurgery ERCP cases.
Roux-en-Y bypass can present a significant challenge[14]. Because it is very rare in China, we did not cover it in our study. For post-gastrectomy patients who still have a native papilla structure, bile duct cannulation is needed in this type of post-surgery ERCP, which will affect the endoscope selection. Because native papilla cannulation of post-gastrectomy ERCP is difficult, our experience on this involves the use of a conventional side-viewing duodenoscope with an elevator as it has more advantages.By contrast, for choledochojejunostomy, directly cannulating the anastomosis is easier with a single balloon enteroscope.
The major biliary diseases of post-choledochojejunostomy patients include a foreign body at the anastomosis, anastomosis stricture, and intrahepatic stones[13]. This is very different from the post-gastrectomy (partial or total) patients. For postgastrectomy patients, the major diseases are common bile duct stricture and stones[15].In view of these differences, choledochojejunostomy is very different from other GI tract reconstructions in terms of the reconstruction route and ERCP operation characteristics. Therefore, in this report, we considered choledochojejunostomy as a special type of upper GI tract reconstruction for discussion and then analyzed and attempted ERCP in this patient group with the aim of offering these patients minimally invasive treatments.

Figure 1 The entire operation team, including the general surgeon (A), endoscopist (B), and nurse assistants(C).
For post-gastrectomy ERCP operation, the use of a conventional side-viewing duodenoscope always has a higher success rate of biliary cannulation and therapy;however, the intubation rate is lower than for the forward-viewing scope[16]. For the side-viewing duodenoscope, there should be more focus on the success rate of scope intubation. We recommend the use of the “retrieval balloon-assisted enterography”[6-9]combined with X-ray imaging to guide the scope progress and effectively improve the scope intubation rate. When using the forward viewing enteroscope, the intubation rate is generally higher, but forward viewing scope cannulation with the normal trans papilla biliary cannulation remains very difficult. For a forward viewing endoscope,there should be more focus on improving the success rate of biliary cannulation and therapy[17]. We chose to use a single balloon enterosope to assist ERCP. One reason is that the single balloon enteroscope is more slim and flexible than other scopes, and it has an overtube to assist with scope progress, which will have a higher scope intubation rate. Another reason is that intrahepatic stones often require the scope to enter the intrahepatic bile duct as well as relative procedures under direct monitoring.Therefore, a scope with a larger working channel is larger in diameter, which cannot go inside the intrahepatic bile ducts, making it unsuitable for stone clearance. At present, SBE-assisted ERCP compatible long length devices are under development and on sale. We use SBE to assist with post-pancreatic biliary surgery ERCP and have achieved satisfying results with a success rate above 90%. This result is superior to previous studies[10,18-22](Table 3).
The post-choledochojejunostomy ERCP operations in our center were all done with the collaboration of endoscopists and surgeons. The endoscopist operated the SBE intubation and relative endoscope maneuvers, while the surgeon was in charge of scope intubation guidance and relative treatments. The importance of this collaboration is one of the most important conclusions we have drawn from our work on post-GI tract reconstruction ERCP.
In addition, for treatment with post-choledochojejunostomy ERCP, we try to push the tip of the enteroscope into the intrahepatic bile duct via the choledochojejunostomy anastomosis, which allows for performance of the treatments under direct visualization. If there is an anastomosis stricture, we use balloon dilation to dilate the stricture and then let the scope enter the intrahepatic duct. Theoretically,performing enteroscopy via the anastomosis and entering the intrahepatic duct can allow for more direct, accurate, and comprehensive diagnosis as well as avoid missed diagnoses. Operations performed under these conditions, such as stone extraction under direct visualization, can be more accurate and avoid unnecessary injury. Large stones can also be removed after holmium laser lithotripsy under SBE direct visualization. Before completing the procedure, this approach can also directly visualize and confirm that the stones are all extracted and that there are no residual stones. If we only rely on X-ray, we cannot achieve the above goals. For this reason,we emphasize placing the enteroscope tip into the intrahepatic bile duct via the anastomosis and then performing treatment. This approach will be more comprehensive and effective and will reduce the need for repeated ERCPs after the operation.
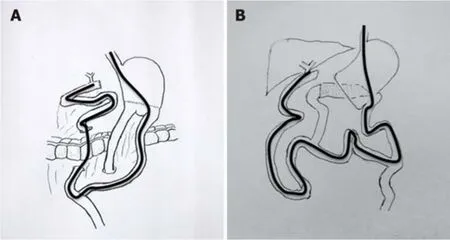
Figure 2 Schema of the operation procedure. A: Billroth II gastroenterostomy and pancreatico-duodenectomy; B:Bilioenteric Roux-en-Y anastomosis and pancreatico-duodenectomy.
The endoscopist is in charge of operating the enteroscope, while the surgeon is in charge of diagnosis and therapy. The enteroscope enters the choledochojejunostomy anastomosis and treats the disease under direct visualization. This is similar to the surgical choledochoscope maneuver. The surgeon is familiar with the anatomy of the intrahepatic duct and stone localization and extraction. As a result, in our opinion,surgeons will have a higher rate of success in performing the diagnosis and therapy.In view of this, SBE-assisted ERCP based on collaboration between the endoscopist and surgeon will be the first choice for patients after choledochojejunostomy.
SBE-assisted therapeutic ERCP is easier with a higher treatment success rate and lower complication rate than other endoscopic assisted operations. However, some limitations remain, including SBE-assisted ERCP compatible accessories that are awaiting further study and the metal stent delivery system that cannot go through the 2.8-mm working channel, etc. In view of this, there is progress on the development of a series of endoscopes and accessories[23]. This is systematic and complicated work,and true progress can only be made in medical practice. SBE-assisted ERCP based on the collaboration between an endoscopist and surgeon after choledochojejunostomy is relatively safe and effective and has a relatively high success rate. Although our results are encouraging for the support of SBE-assisted ERCP, further large prospective, multicenter studies to evaluate the efficacy of SBE-ERCP need to be conducted to confirm these findings[13]. However, ERCP after choledochojejunostomy and after upper GI tract surgery remains challenging. We are striving to make ERCP treatment in these patients safer, more effective, more standardized, easier to operate,and easier to generalize as a technique.
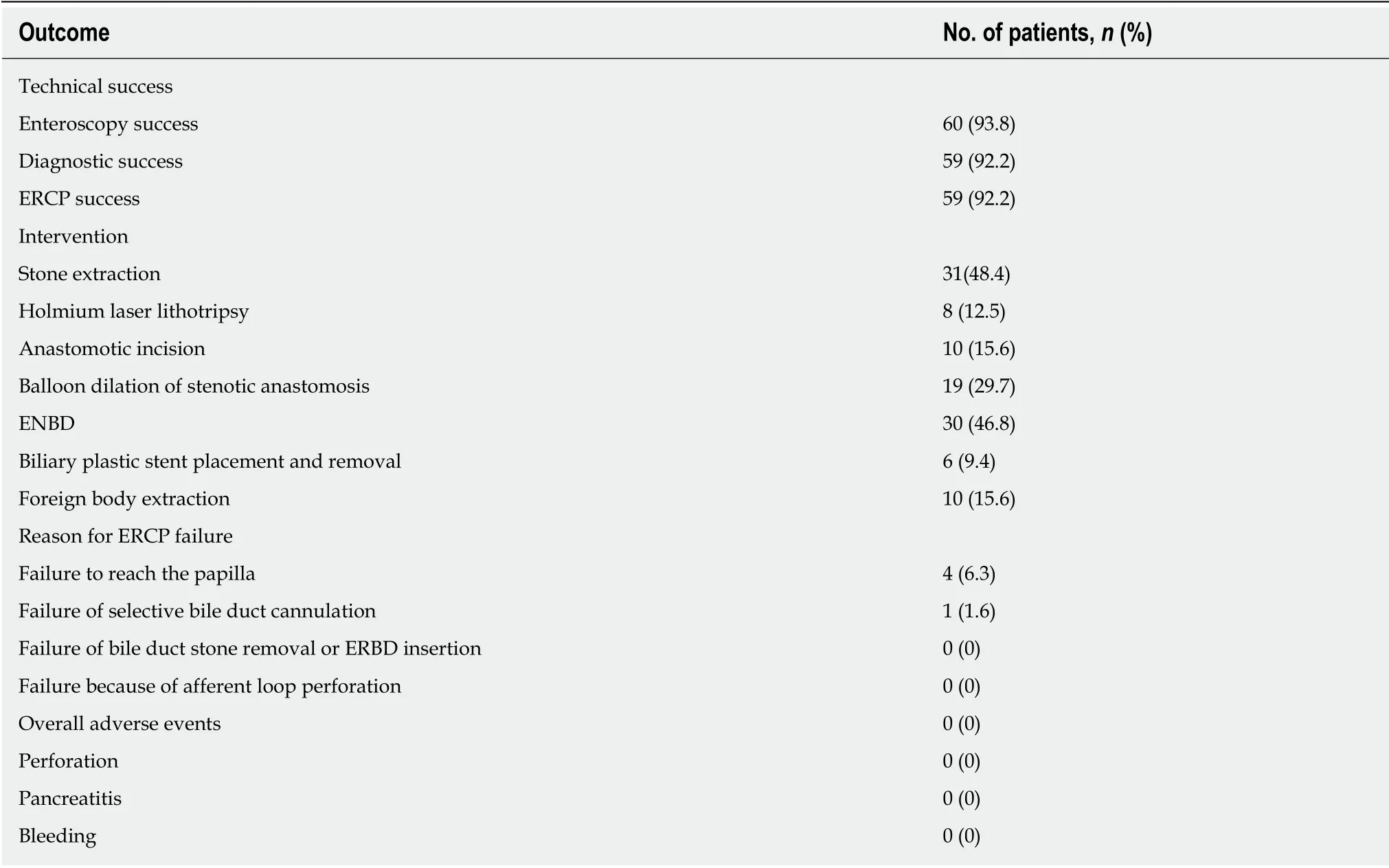
Table 2 Clinical outcomes of endoscopic retrograde cholangiopancreatography in the study cohort
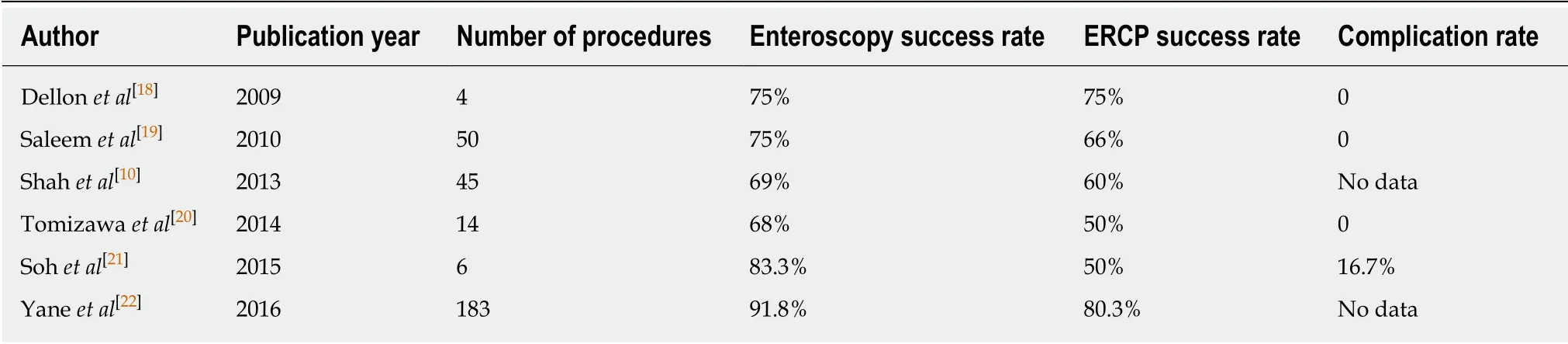
Table 3 Summary of reports of endoscopic retrograde cholangiopancreatography using single-balloon enteroscopy technique in patients with Roux-en-Y anastomosis
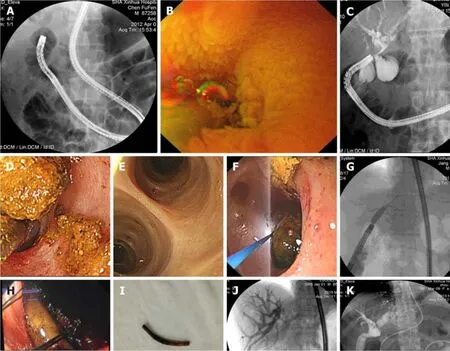
Figure 3 The operation procedure. A: The endoscopist collaborated with the nurse to inflate the scope and overtube as well as deflate and move the equipment,which were repeated to slowly advance the scope forward; B: Locating the bilioenteric Roux-en-Y anastomosis (Endoscopic view); C: Completion of the biliary duct cannulation and cholangiogram, revealing intrahepatic bile duct stones; D: Intrahepatic bile duct stones were extracted successfully; E: Operations such as stone extraction under direct visualization can be more accurate. Before completing the procedure, visualizing and confirming that the stones are all extracted and that there are no residual stones are possible; F: Large stones can also be extracted after holmium laser lithotripsy under SBE direct visualization; G: Bilioenteric Roux-en-Y anastomotic stricture was treated by balloon dilatation; H: Foreign body at the anastomotic site (endoscopic view); I: The foreign body was extracted successfully; J:Bilioenteric Roux-en-Y anastomosis malignant stenosis was treated by balloon dilatation and stenting; K: Successful endoscopic nasobiliary drainage via a single balloon enteroscope.
ARTICLE HIGHLIGHTS
Research background
Bilioenteric Roux-en-Y anastomosis is one of the most complicated approaches for reconstructing the gastrointestinal tract, and endoscopic retrograde cholangiopancreatography (ERCP) is technically challenging in patients with bilioenteric Roux-en-Y anastomosis. The optimal endoscopic strategies for such cases remain unknown.
Research motivation
The motivation of this research was to explore the feasibility and effectiveness of single balloon enteroscopy-assisted (SBE-assisted) therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis based on multi-disciplinary collaboration between endoscopists and surgeons.
Research objectives
To explore the feasibility and effectiveness of SBE-assisted therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis based on multi-disciplinary collaboration between endoscopists and surgeons as well as report the experience from China.
Research methods
This is a single center retrospective study. All of the SBE-assisted therapeutic ERCP procedures were performed by the collaboration between endoscopists and surgeons. The operation time,success rate, and complication rate were calculated.
Research results
Forty-six patients received a total of 64 SBE-assisted therapeutic ERCP procedures, with successful scope intubation in 60 (93.8%) cases and successful diagnosis in 59 (92.2%). All successfully diagnosed cases received successful therapy. None of the cases had perforation or bleeding during or after operation, and no post-ERCP pancreatitis occurred.
Research conclusions
Based on multi-disciplinary collaboration, SBE-assisted therapeutic ERCP in patients after bilioenteric Roux-en-Y anastomosis is relatively safe and effective and has a high success rates.
Research perspectives
Our results are encouraging for the support of SBE-assisted ERCP, and further large prospective,and multicenter studies to evaluate the efficacy of SBE-ERCP need to be conducted to confirm these findings.
ACKNOWLEDGEMENTS
We thank our endoscopy assistants, Lei Zang, Yan-Ming Duan, Yu-Feng Li, Li-Li Xu,Fei Shen, and Chao Ting, who assisted with the examinations and worked out the procedural standards for preparation, assistance, and post-processing of the procedure. They were invaluable for performing this study.
杂志排行
World Journal of Gastroenterology的其它文章
- Chinese guidelines on management of hepatic encephalopathy in cirrhosis
- Sexual health and fertility for individuals with inflammatory bowel disease
- High mobility group box-1 release from H2O2-injured hepatocytes due to sirt1 functional inhibition
- Zinc-α2-glycoprotein 1 attenuates non-alcoholic fatty liver disease by negatively regulating tumour necrosis factor-α
- Clostridium butyricum alleviates intestinal low-grade inflammation in TNBS-induced irritable bowel syndrome in mice by regulating functional status of lamina propria dendritic cells
- CARMA3/NF-κB signaling contributes to tumorigenesis of hepatocellular carcinoma and is inhibited by sodium aescinate
