Sexual health and fertility for individuals with inflammatory bowel disease
2019-10-28RomainLeenhardtPaulineRivirePatrickPapazianIsabelleNionLarmurierGuillaumeGirardDavidLahariePhilippeMarteau
Romain Leenhardt, Pauline Rivière, Patrick Papazian, Isabelle Nion-Larmurier, Guillaume Girard,David Laharie, Philippe Marteau
Abstract The impact of a chronic disease such as inflammatory bowel disease (IBD) on sexual functioning and body image can significantly impair the quality of life of patients. This review considers the sexual and fertility aspects of IBD patients and their daily management. Modern IBD healthcare management should include appropriate communication on sexuality and consider psychological,physiological, and biological issues. Patients with IBD have less children than the general population, and voluntary childlessness is frequent. The most influential factors reported by IBD patients who experience fertility alteration are psychological and surgery-related problems. Pregnancy is a major concern for patients, and any pregnancy for IBD patients should be closely followed-up to keep the chronic disease in a quiescent state. Preconceptional consultation is of great help.Key words: Inflammatory bowel disease; Crohn's disease; Ulcerative colitis; Fertility;Pregnancy; Sexuality
INTRODUCTION
Crohn's disease (CD) and ulcerative colitis (UC) have a high burden on a patient's quality of life (QoL)[1]. QoL and patient-related outcomes are the treatment targets for managing patients who are suffering from inflammatory bowel disease (IBD)[2]. Sexual health is a main determinant of QoL and is negatively impacted in patients with IBD[3,4]. IBD patients expect more open listening and better information from care providers[5]. Fertility can be affected by IBD[6], and voluntary childlessness is more frequent in IBD patients than in the general population, sometimes because of improper medical knowledge and/or communication[7].
In this review, we summarize the knowledge on the impact of IBD on sexual health and fertility and what gastroenterologists should do to better meet patients'expectations regarding these often-neglected topics.
Data sources and searches
An electronic search of the literature was conducted using MEDLINE (PubMed). The search was restricted to English language. The search strategy used the following MeSH and text words: “Sexual dysfunction”, “Inflammatory Bowel disease”,“Fertility”, “Psychological”, “Crohn's Disease” and “Ulcerative colitis”.
SEXUAL HEALTH
Sexual health and sexual function: definitions
Sexual health is defined by the World Health Organization as “a state of physical,emotional, mental and social wellbeing in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity”[8]. Sexual health has five dimensions:physical, emotional, social, mental, and spiritual. Along with body image, it is an important aspect of psychosocial functioning and has a significant impact on overall QoL[9].
Assessing sexual function is a quantitative approach toward sexual health that considers the domains of desire, arousal, orgasm and satisfaction, erectile function for men, and lubrication and pain for women. Specific questionnaires on sexual function have been designed and validated in healthy men and women and in diseased populations. The most used auto-questionnaires are the Female Sexual Function Index(FSFI) for women[10]and the International Index Erectile Function (IIEF) for men[11].Within these questionnaires, sexual dysfunction has been defined as an FSFI score below 26.55 and IIEF score below 42.9. There is no specific tool for IBD patients, but some QoL questionnaires designed for these patients include questions on sexual health[12-14].
Impact of the disease and frequency of sexual dysfunction
Body image and intimacy are some of the major concerns of IBD patients but rarely are spontaneously expressed[15]. In the IMPACT study, a wide-ranging European study including 4990 IBD patients recruited by patients' associations, 40% reported that their disease prevented them from pursuing intimate relationships[1]. Indeed,sexual dysfunction rates are higher in patients with IBD than in the general population[16]; it is indeed by reported 45%-60% of IBD women and 15-25% of IBD men[3,16,17], compared with 30% of women and 5% of men in the general population[16].Around 40% of IBD men suffer from erectile dysfunction versus 15% of men of the same age in the general population[3,16,18]. A study based on the Danish medical register and that included 31498 IBD and 314980 non-IBD men showed that erectile dysfunction treatments were more often used by IBD patients [12% vs 10%, HR 1.22(1.18-1.27)][18]. In IBD men, a reduction of sexual desire is also more frequent than in the general population[16]. Body image is lower in 70% of patients, especially in women who have had a surgery[19]. The sexual activity rate of IBD patients appears similar to healthy individuals, indicating that IBD patients engage in sexual relationships but that their satisfaction is below that of the general population[16,21].
Receptive anal sexuality in IBD
Receptive anal sexuality (RAS) is not an exceptional practice but is still a taboo topic in health care. General population studies in North America and Europe show that around 10% of women engage in frequent RAS and 35% have experienced it[22,23].Around 5%-15% of men report regular RAS and 10%-45% lifetime RAS[23,24]. The consequences of RAS in IBD patients when it comes to rectal symptoms and lesions,susceptibility of inflamed mucosa to sexually transmitted infectious agents, anal dysplasia, and anal carcinoma risks have been poorly studied[25]. Anal carcinoma prevalence is increased in patients with anoperineal CD[26]and is associated with human papilloma virus (HPV) infection and immunosuppressive therapy[27].Currently, there are no guidelines on screening for sexually transmitted infections or proposing HPV vaccinations for IBD patients[28]. Dibley et al[29]showed that IBD men having sexual relationships with other men are reluctant to disclose their sexual practices because of fear of medical judgment. However, patients would benefit from an open discussion with medical staff and information about their ability to engage in RAS.
Factors associated with sexual dysfunction
Sexual health is multidimensional. In patients with IBD, sexual dysfunction in IBD is associated with anxiety, depression, impaired QoL, and fatigue but not with disease activity[3,16-18,30,31]. In a study by Bel et al[3], the univariate association of IBD activity on sexual function was totally explained by depression. This is consistent with other observations showing that in IBD patients psychosocial factors are more significant predictors of overall QoL than disease activity[9,32]. Depression and anxiety are frequent psychological comorbidities in IBD and are the major drivers of sexual dysfunction[3,16,17]. Depression is found in as many as 20%-30% of IBD patients in remission and anxiety in 10%-30%[32]. Psychological burden may be not only a cause,but also aggravated by sexual dysfunction.
Little data exist on the impact of surgery on sexual function in IBD men. In a French study on 166 IBD men, a history of abdominal surgery was an independent predictor of erectile dysfunction with an odds ratio of 2.24 (95% confidence interval 1.04-4.92, P= 0.04)[16]. Studies on the impact of ileal pouch anal anastomosis (IPAA) in UC patients provided conflicting results. Postoperative screening found the frequency of sexual dysfunction in men after IPAA as varying from 4%-30%[33,34]. Prospective studies comparing pre- and postoperative scores showed an improvement in the overall QoL and sexual function[35,36]. Prospective and follow-up data are needed to evaluate the risk of erectile dysfunction and retrograde ejaculation after pelvic surgery and abdominal surgery in IBD men. For the moment, the ECCO guidelines recommend discussing sperm banking with the patient before IPAA[37]. In women, surgery has been found to be associated with a poorer body image[19]and dyspareunia[38].
In the literature, the majority of IBD drugs appear to have very limited influence on sexual dysfunction whereas other medications like psychotropic drugs are known to induce sexual dysfunction[39,40]. However, the statistical power of previous studies is limited, and rare side effects could not be properly evaluated. In a study by Marín et al[17]on 202 IBD women, corticosteroids were independently associated with sexual dysfunction, which may be because of their impact on body image. Hypogonadism and decreased levels of testosterone have also been shown in IBD men[41]and could be responsible of sexual dysfunction. Methotrexate has been reported to be associated with erectile dysfunction in a few cas reports with a very low level of evidence[42,43].Concerning the use of biological agents, the study by Marín et al[17]showed its use was an independent factor of sexual dysfunction on 153 IBD men. However, no data on sexual dysfunction were reported in the systematic literature review by Semet et al[44](Table 1).
Management of sexual dysfunction
The management of sexual dysfunction is a complex bio-psycho-social process (Figure 1). Most IBD patients expect their gastroenterologist to provide information about the disease of their impact on their sexuality as early as diagnosis[17]and to ask them regularly about their sexual health[16]. However, it seems that this topic is rarely addressed in daily practice. One study found that only 8% of patients had been askedabout their sexual health in the past[29]. Among 69 gastroenterologists participating in a recent French survey, only 16% addressed the topic, even though 93% considered it would be a good thing to do so[45]. The main reason not to tackle the subject was the feeling of a lack of knowledge regarding sexual dysfunction management (45%),reluctance to shame patients (29%), discomfort from the doctor (19%) and, finally, lack of time (9%). Proctologic surgeons addressed the subject more often (55% vs 9%, P <0.001).
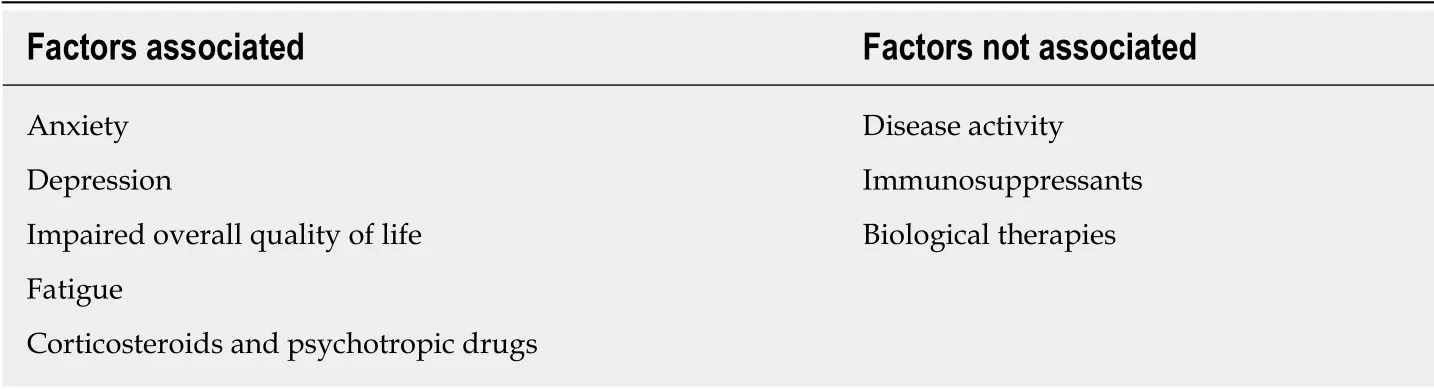
Table 1 Factors associated with sexual dysfunction and erectile dysfunction in inflammatory bowel disease patients
The first step would be to screen patients for impaired sexual function.Questionnaires such as the IIEF and FSFI are rarely used in daily practice. A specific index for IBD patients could be an interesting tool and should also evaluate psychological comorbidities such as depression and anxiety.
The benefit of psychoeducational sessions on sexual health has never been evaluated in IBD patients. However, this approach has proven to be effective in patients suffering from irritable bowel syndrome or those who have been treated for a nongastroenterological disease[46]. Regarding medications, a randomized controlled study in patients with erectile dysfunction after IPAA showed a 79% response rate for the patients treated with sildenafil vs 17% for those in the placebo group[47].
Referral to a sexologist should be considered in several situations. The first is when a problem is discovered by the screening questions and when the gastroenterologist is reluctant to tackle the subject. Patients should also be referred in the case of the failure of a first-line management (to a sexologist helping to inform and prescribe erectile dysfunction medication), in persistent sexual dysfunction, and/or couple suffering.The referral process represents a strong signal for the patient that his/her suffering has been heard.
FERTILITY
Fertility is the capacity to produce a child[48], differing from fecundability, which is the probability of pregnancy per month with unprotected intercourse. Approximately 80% of couples will conceive in the first 6 months of attempting pregnancy[49].Infertility is defined as the failure to achieve a pregnancy after 12 months of unprotected intercourse. Table 2 shows the main causes of infertility in the general population and a few IBD-specific situations. What the gastroenterologist should do in this context is summarized in Table 3. Pregnancy outcomes in the general population compared with IBD patients are shown in Table 4. IBD typically affects young patients during their reproductive years. Thus, fertility is a major concern for IBD patients. Patients with quiescent IBD have similar fertility rates compared with the general population. However, because of voluntary childlessness, IBD patients have fewer children than the general population[7]. Apprehension about fertility,potentially adverse pregnancy outcomes, risk of IBD in the offspring, and medication safety may be the causes for the fear and doubts during preconception. Moreover, in cases of IBD, patients' perceptions about fertility are often associated with negative views[50].
Influence of disease activity on fertility in females and males
Many series assessed the impact of disease activity on fertility in females and males,and there is no evidence that UC or inactive CD affect fertility[51]. Tavernier et al[6]showed that the infertility rates are similar between women with quiescent IBD and no prior pelvic surgery (5%-14%) and the general population. Nevertheless, in cases of active disease, peritoneal inflammation might be responsible for intra-abdominal adherences and hence a decrease in the fertility rate. Moreover, decreased libido,dyspareunia, chronic abdominal pain, and anxiety/depression disorders can lead to increased infertility for IBD patients[30].
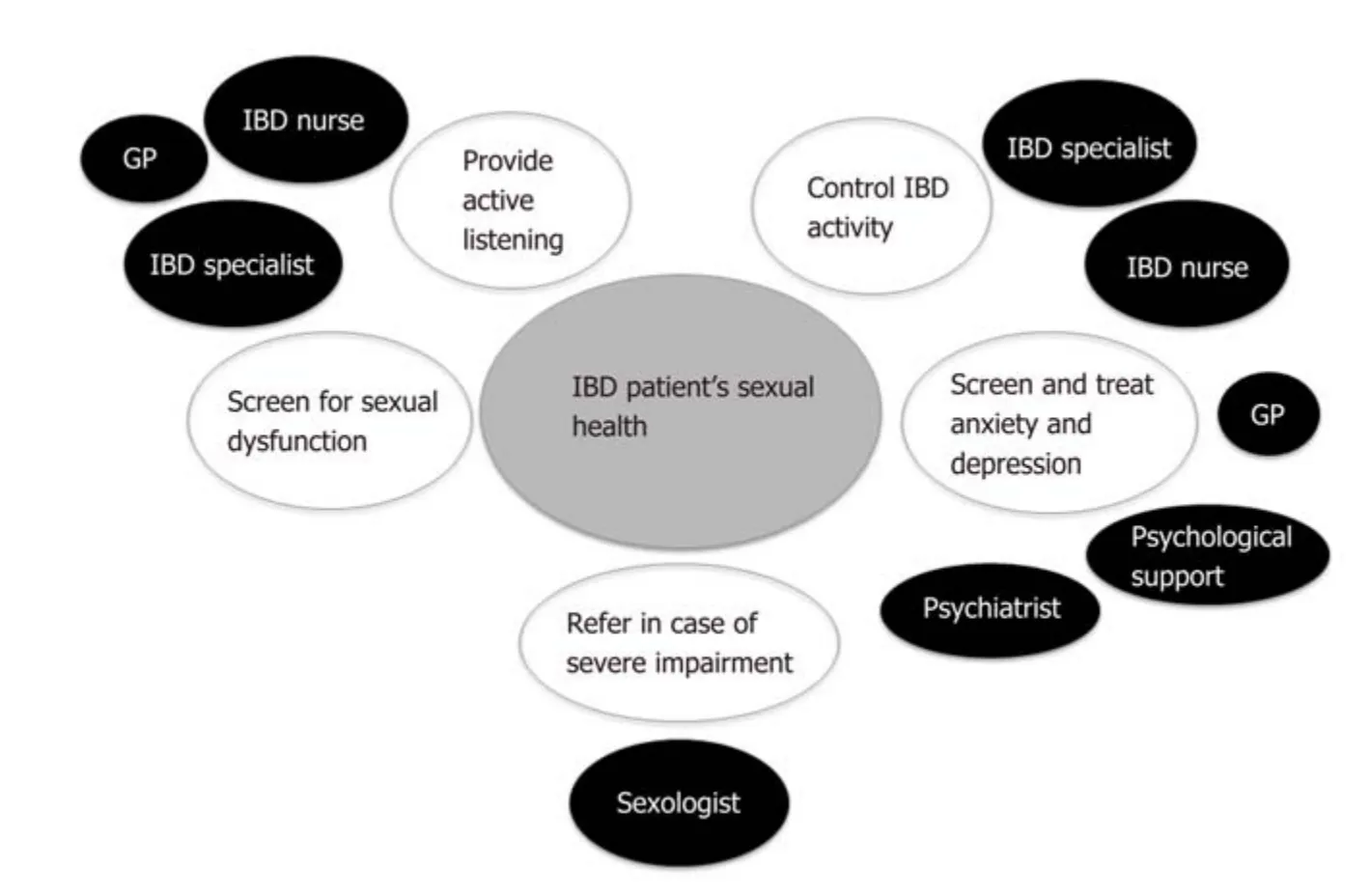
Figure 1 Proposals for the management of sexual dysfunction. GP: General practitioner; IBD: Inflammatory bowel disease.
The disease activity at conception or during pregnancy is considered one of the most significant risk factors for adverse pregnancy outcomes[52]. Moreover, women affected by IBD and who are considering pregnancy often stop their treatment without informing their doctors[53]. Studies from the Netherlands have demonstrated that a systematized preadvisory information program[54]improved the birth rate and reduced the risk of relapse of IBD during pregnancy. These positive effects can be attributed to the beneficial impacts of preconceptual care on pregnancy planification during remission, to the IBD treatment adherence, and to smoking cessation during pregnancy. Thus, counseling should be considered a crucial aspect in the management of all IBD patients and should be implemented in IBD centers.
IBD medications and fertility
Most medical treatments for IBD have no effect on the patient's ability to conceive[55].Sulfasalazine is an exception, though, because it increases the risk of subfertility in men by altering the spermogram[44]; it reduces sperm motility and increases the proportion of abnormal forms[56]. Birnie et al[57]performed a sperm analysis in 21 patients receiving sulfasalazine treatment for IBD and reported that 86% and 72% of the patients had abnormal semen and oligospermia, respectively. A switch to 5-aminosalicylic acid (mesalazine) generally restores fertility and spermogram anomalies. There is still some debate regarding the effects of thiopurines on fertility.Dejaco et al[58]showed that the sperm quality of 18 IBD patients was not altered after 3 months of using azathioprine. In a cohort of 40 IBD men[59], thiopurines did not decrease sperm quality but was sometimes associated with the impairment of sperm motility. Methotrexate (MTX) can be responsible for oligospermia and is reversible after stopping usage; this drug is contraindicated for both women and men because it is embryotoxic[60]. Corticosteroids and cyclosporine seem to have no effects on fertility.However, there is some debate about the effect of infliximab on fertility. In studying a small series of 10 IBD patients, Mahadevan et al[61]reported a trend toward decreased sperm motility with infliximab therapy. However, Villiger et al[62]reported that the sperm quality of 26 men treated with infliximab for spondylarthritis was similar to that of healthy controls. Data on the impact of adalimumab, vedolizumab, and ustekinumab on human fertility are insufficient.
Surgery-related problems
Surgery-related problems can alter fertility, and patients should be informed prior to all surgical procedures. A meta-analysis showed that IPAA increases the risk of infertility in women with UC by approximately threefold[63]. The mechanisms likely responsible for this important increase of the subfertility rate have been related to postsurgical abdominal adhesions and also to tubal obstructions[64]. However, Beyer-Berjot et al[65]demonstrated that infertility rates after laparoscopic IPAA surgery appears to be lower than after open surgery.
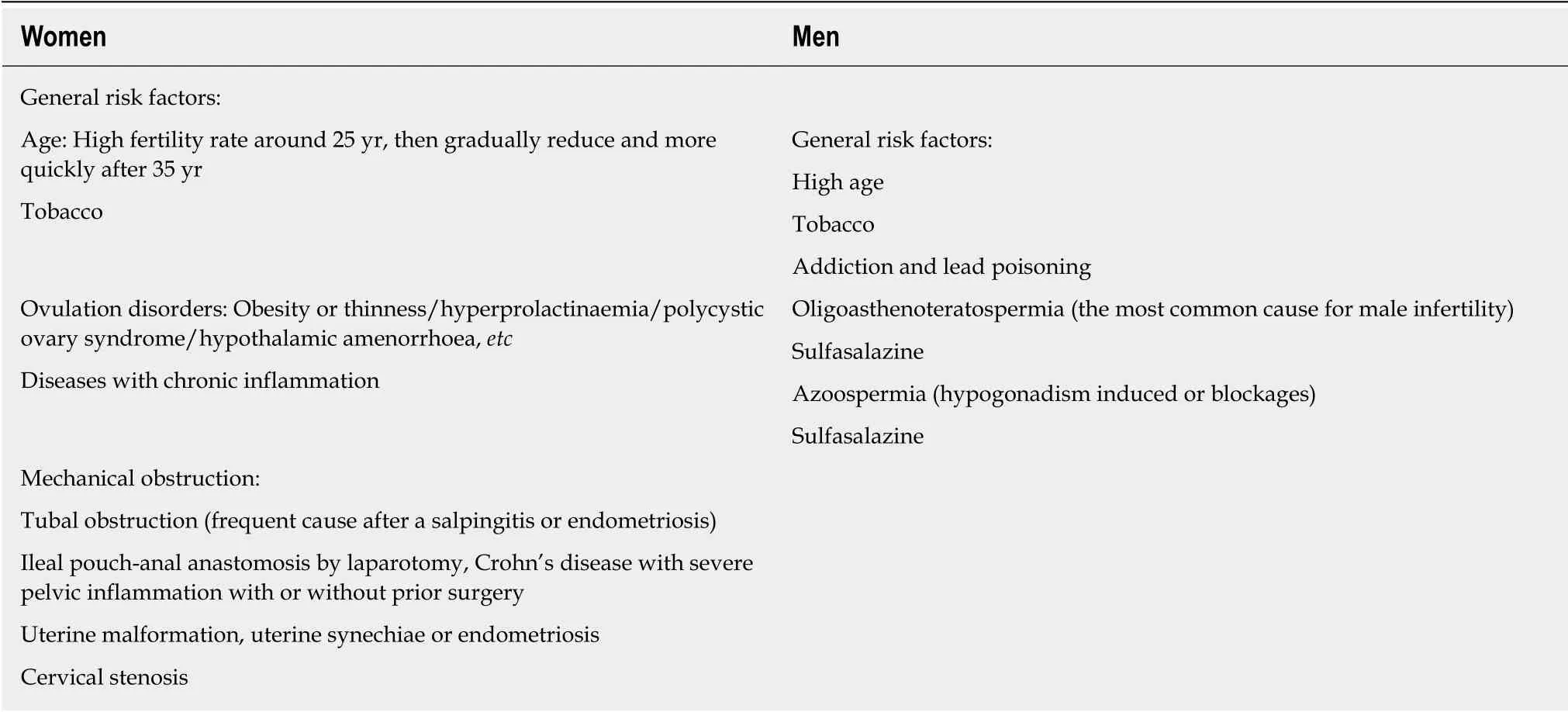
Table 2 Summary of the major causes of infertility in the general population and a few specific situations related to inflammatory bowel disease
Nonsurgery-related problems
In CD, perineal disease and fallopian tube inflammation may occur and, in rare cases,may induce a reduction in the fertility rate. A systematic review by Tavernier et al[6]showed a decrease in Crohn's women fertility rates between 17% and 44% when compared with controls; however, most of these studies did not distinguish voluntary childlessness from involuntary infertility. Thus, regarding involuntary infertility,women with CD tend to have similar rates compared with control patients.Concerning women with UC, most studies have not found any difference in the fertility rates compared with the general population[66,67].
A few studies have assessed the anti-Mullerian hormone (AMH), which is considered an accurate hormonal marker of ovarian reserve. In a retrospective case control study including 50 women with CD, Fréour et al[68]showed that women older than 30 years of age and with a colonic location could present an accelerated alteration of the ovarian reserve when compared with control healthy women. The authors hypothesized that the proximity between the colon and the ovaries may be responsible for the higher level of chronic inflammation and, thus, an alteration of the ovarian reserve. Another case control study showed that 35 patients with CD had significantly lower levels of serum AMH than the matched controls and that disease activity was inversely correlated to the AMH levels[69].
Male fertility
The medical literature has shown that advanced age, consumption of tobacco and alcohol, and psychological stress are risk factors for male infertility[70]. Moreover, a large meta-analysis from Sermondade et al[71]indicated that there was a correlation between body mass index and the prevalence of azoospermia or oligozoospermia.However, there is some controversy about the impact of IBD in men's fertility. Two population-based studies on men with UC did not show any reduction in fertility rate,whereas a recent medical literature overview indicated that active inflammation, poor nutrition, alcohol use, smoking, medications, and surgery may cause infertility in men with IBD[72]. There is no evidence of any impact of IBD surgery on male fertility,except from the debated risk of erectile dysfunction (see the section titled “Associated factors to sexual dysfunction”).
Couple infertility and IBD
Voluntary childlessness and psychological factors: Voluntary childlessness is more frequent in IBD patients than in the general population; it was estimated in two studies in the United States and Great Britain to be at 14% to 18% vs 6% in the general population[73,74]. This situation is thought to be mostly because of fears of the potential negative impact of pregnancy on the disease activity and also on transmitting IBD to the patient's child[66,74]. Moller et al[75]studied the estimation of the familial risk of IBD in the entire Danish population from 1977 to 2011. The risk of CD and UC in the firstdegree relatives of a CD and UC case was eightfold and fourfold increased,respectively, compared with families without IBD history. Laharie et al[76]reportedthat when the two parents were affected by IBD, the children had a 30% risk of developing IBD. Several studies have shown a significant association between voluntary childlessness and a low level of knowledge about IBD compared with controls, indicating that education could reassure some patients and allow them to consider pregnancy by correcting misconceptions[74]. This again stresses the importance of patient counseling before pregnancy. However, Nørgård et al[77]suggested that women with IBD were not so worried about their disease as they reported similar elective abortion rates compared with healthy women.

Table 3 What the gastroenterologist should do in the case of infertility for a patient with inflammatory bowel disease
How to treat infertility
The first step to treat infertility is to provide accurate counseling to positively impact preconceptual care. The optimization of nutritional status, vitamins supplementation(vitamin D and zinc) and the cessation of tobacco and alcohol are necessary. Overall,how to control the disease activity must be obtained and maintained. IBD couples facing infertility should be referred to specialized gynecology centers. However, the medical literature is scarce on infertility treatment in IBD patients. Assisted reproductive technology (ART) such as in vitro fertilization, intracytoplasmic sperm injection, and frozen embryo replacement can be proposed to infertile IBD couples.Friedman et al[78]showed a significant decrease of the live birth rate within 18 mo after the beginning of ART for women with prior CD surgery compared with non-IBD women. Moreover, in the case of women affected by UC, prior surgery before ART did not affect the chance of a live birth[79]. In cases of persistent infertility for IBD patients, an overall recommendation could be to consider ART earlier than in the general population (for example after 6 mo) because it might be more tedious to succeed.
CONCLUSION
In IBD patients, more than 50% of women suffer from sexual dysfunction and 45% of men from erectile dysfunction. Psychological comorbidities, body image, and disease perception are strongly associated with poor sexual health in IBD patients. Because of this, patients are calling for more information on IBD and sexuality from their care providers. Open discussions, psychoeducational sessions, and referrals to a sexologist when needed would improve the QoL of patients. Fertility is another major concern among IBD patients. Inactive IBD has little to no impact on fertility rates, but psychological comorbidities and misconceptions about the disease lead to voluntary childlessness among IBD patients. Finally, patient counseling before and during pregnancy could be helpful in the patient's reproductive years.

Table 4 Pregnancy outcomes in the general population compared with inflammatory bowel disease patients
杂志排行
World Journal of Gastroenterology的其它文章
- Chinese guidelines on management of hepatic encephalopathy in cirrhosis
- High mobility group box-1 release from H2O2-injured hepatocytes due to sirt1 functional inhibition
- Zinc-α2-glycoprotein 1 attenuates non-alcoholic fatty liver disease by negatively regulating tumour necrosis factor-α
- Clostridium butyricum alleviates intestinal low-grade inflammation in TNBS-induced irritable bowel syndrome in mice by regulating functional status of lamina propria dendritic cells
- CARMA3/NF-κB signaling contributes to tumorigenesis of hepatocellular carcinoma and is inhibited by sodium aescinate
- Laparoscopy-assisted pylorus-preserving gastrectomy for early gastric cancer: A retrospective study of longterm functional outcomes and quality of life
