不同手术入路全髋关节置换术对髋臼发育不良的疗效对比研究
2019-10-03贾健成凯
贾健 成凯


【摘要】 目的:對比不同手术入路全髋关节置换术对髋臼发育不良的疗效。方法:选择2016年8月-2018年9月在本院行全髋关节置换术的髋臼发育不良患者62例,采用随机数字表法分为对照组与观察组,每组31例。两组均由同一组具有5年以上临床经验的医护人员在全麻下进行手术,对照组行常规后侧入路全髋关节置换术,观察组行直接前侧入路全髋关节置换术。对比两组临床疗效、炎性反应指标及髋臼假体位置。结果:观察组治疗总有效率(96.77%)与对照组(93.55%)比较,差异无统计学意义(P>0.05)。术后两组C反应蛋白(CRP)、白细胞介素-1(IL-1)、肿瘤坏死因子-α(TNF-α)及肌酸激酶(CK)水平均明显高于术前(P<0.05),且对照组CRP、IL-1、TNF-α及CK均高于观察组(P<0.05)。两组髋臼前倾角与外展角比较,差异均无统计学意义(P>0.05)。结论:直接前侧入路与常规后侧入路行全髋关节置换术对髋臼发育不良患者的疗效相当,且髋臼假体位置差别不大,但直接前侧入路全髋关节置换术能够减轻患者炎性反应。
【关键词】 手术入路; 全髋关节置换术; 髋臼发育不良
Comparative Study of the Effects of Total Hip Arthroplasty in Different Surgical Approaches on Acetabular Dysplasia/JIA Jian,CHENG Kai.//Medical Innovation of China,2019,16(23):00-010
【Abstract】 Objective:To compare the effects of total hip arthroplasty through different surgical approaches on acetabular dysplasia.Method:A total of 62 patients with acetabular dysplasia underwent total hip arthroplasty in our hospital from August 2016 to September 2018 were selected.They were divided into control group and observation group by random number table method,31 cases in each group.The two groups were operated under general anesthesia by the same group of medical staff with more than 5 years of clinical experience.The control group was treated with routine posterior approach total hip arthroplasty.The observation group was treated with direct anterior approach total hip arthroplasty.The clinical efficacy,inflammatory response index and acetabular prosthesis position were compared between the two groups.Result:The total effective rate of the observation group(96.77%)was compared with that of the control group(93.55%),the difference was not statistically significant(P>0.05).The levels of C-reactive protein(CRP),interleukin-1(IL-1),tumor necrosis factor-α(TNF-α)and creatine kinase(CK)in both groups after operation were significantly higher than those before operation(P<0.05),and the levels of CRP,IL-1,TNF-α and CK of the control group were higher than those of the observation group (P<0.05).There was no significant difference in acetabular anteversion angle and abduction angle between the two groups(P>0.05).Conclusion:The effect of direct anterior approach is comparable to that of the conventional posterior approach for total hip arthroplasty in patients with acetabular dysplasia and there is little difference in the position of acetabular prosthesis,but the direct anterior approach total hip arthroplasty can reduce the inflammatory response in patients.
【Key words】 Surgical approaches; Total hip arthroplasty; Acetabular dysplasia
First-authors address:Linfen Peoples Hospital,Linfen 041000,China
doi:10.3969/j.issn.1674-4985.2019.23.002
发育性髋关节发育不良(过去也称为先天性髋关节脱位)是以髋关节发育过程中空间及时间上不稳定为特征的一组病变的总称,主要包括髋关节脱位、半脱位及髋臼发育不良,其中以髋臼发育不良较为常见[1-2]。该病可引起患儿步态异常,相邻关节发育异常而导致脊柱发育畸形,成年后出现腰痛及髋关节退行性病变而引起的疼痛等,目前对于该病的病因尚未完全明确,大部分学者认为与力学因素、遗传移速、性别及环境差异有关,治疗以手术治疗为主[3]。多项研究显示,全髋关节置换术对髋臼发育不良患者疗效确切,但传统的全髋关节置换术以后侧入路为主,此入路对患者的外侧结构可造成破坏而增加假体脱位的发生率,不仅给患者带来巨大的痛苦,还对患者家庭经济造成不小的负担[4-5]。直接前侧入路可通过阔筋膜张肌及股直肌间隙入路对患者外侧稳定结构无破坏作用,且稳定性较高。目前对于不同手术入路全髋关节置换术对髋臼发育不良疗效对比主要集中于临床观察方面,对于两种术式对患者实验室指标与髋臼位置方面的影响方面鲜有相关报道,因此本研究旨在通过对比两种手术入路对髋臼发育不良患者炎性反应指标及髋臼假体位置方面的影响进行分析,以期为临床上全髋关节置换术治疗髋臼发育不良提供新的思路。现报道如下。
1 资料与方法
1.1 一般资料 选择2016年8月-2018年9月在本院行全髋关节置换术的髋臼发育不良患者62例进行研究。纳入标准:(1)经临床诊断,影像学检查确诊为CroweⅠ、Ⅱ型的髋臼发育不良者;(2)初次行全髋关节置换术;(3)髋关节活动度良好;(4)BMI指数在30 kg/m2以下;(5)神志清醒,智力正常,可与医护人员进行正常交流者。排除标准:(1)既往髋部手术者;(2)股骨严重畸形者;(3)近期出现血栓性疾病者;(4)恶性肿瘤者;(5)严重骨质疏松症者。采用随机数字表法将患者分为对照组与观察组,每组31例。所有患者及家属均知情同意并签署知情同意书,本研究已经医院伦理委员会批准。
1.2 方法 两组均由同一组具有5年以上临床经验的医护人员在全麻下进行手术。(1)对照组行常规后侧入路全髋关节置换术,麻醉后患者侧卧,对术区常规消毒、备皮、铺巾,在髋关节后外侧作一长约10 cm的切口,逐层切开皮肤、皮下筋膜后暴露阔筋膜张肌及臀大肌。切开阔筋膜对大粗隆上滑膜组织进行钝性分离,以Hoffman拉钩牵开臀中肌,将外旋肌群充分暴露,在大转子止点将梨状肌、上、下孖肌等短外旋肌群切断后保留腱性组织。以骨膜剥离器对关节囊进行钝性分离,将关节囊进行T形切开,并将后方关节囊部分切除,行股骨颈截骨,保留1 cm股骨距,将股骨头完整取出。采用髋臼锉对髋臼至髋臼壁进行逐层打磨至均匀渗血,打磨过程中注意对前后方骨质的保留,选择合适的骨臼杯进行安装,前倾角控制在10°~15°,外展角控制在40°~45°,髋臼前后壁骨质损伤严重者可植入1~3枚松质骨螺钉固定,安装内衬。屈曲、内旋下降骨髓腔显露,保持小腿在手术创面垂直,扩髓后对术区进行脉冲冲洗,插入股骨柄假体,选择合适的股骨头假体进行安装,髋关节复位后再次进行脉冲冲洗,留置负压引流管,关闭切口后通过引流管注射10%氨甲环酸注射液(生产厂家:贵州圣济堂制药有限公司,批准文号:国药准字H20063068,规格:5 mL︰0.5 g)20 mL及0.75%罗哌卡因(生产厂家:宜昌人福药业有限责任公司,批准文号:国药准字H20103636,规格:10 mL︰100 mg)10 mL。(2)观察组行直接前侧入路全髋关节置换术,麻醉后取健侧卧位,常规消毒、铺巾。在髂前上棘下、外侧2 cm处向Gerdy方向作一10~11 cm的切口,逐层切开并分离组织,钝性分离阔筋膜及下层肌肉将Smith-Peterson间隙充分暴露,将旋股外侧动脉升支切段并结扎,钝性分离骨直肌与阔筋膜张肌,并将关节囊上方脂肪组织去除以充分暴露关节囊。切开关节囊将股骨颈完全暴露后行双道截骨,取出股骨头及断颈,将股骨头圆韧带及髋臼周围增生骨赘清除以充分暴露髋臼,采用髋臼锉逐渐对其进行打磨直至骨质断面有新鲜血液渗出,冲洗后以前倾角5°~10°,外展角35°~45°标准进行臼杯安装,视髋臼杯稳定性决定是否使用螺钉,安装内衬。将患肢外旋、后伸,在股骨近端插入直骨撬与侧角骨撬,以电刀对股骨近段软组织进行电刀松解以暴露髓腔,扩髓后对术区进行脉冲冲洗,插入股骨柄假体,安装股骨头假体后复位髋关节,再次对术区进行冲洗,留置负压引流管,关闭切口,术后处理同对照组。
1.3 观察指标与判定标准 对比两组临床疗效、血清学指标及髋臼假体位置。(1)疗效评价标准:在术前、术后24周采用髋关节Harris评分对患者髋关节功能进行评估,计算髋关节评分改善率,髋关节评分改善率=(术后评分-术前评分)/术后评分×100%,根据计算结果进行疗效评估,显效:髋关节评分改善超75%;有效:髋关节评分改善50%~75%;好转:髋关节评分改善30%~50%;无效:髋关节评分改善不足30%[6]。总有效=显效+有效+好转。(2)炎性反应指标:在术前及术后1周抽取患者空腹外周静脉血4 mL,以3 000 r/min转速离心15 min,分离血清后对肿瘤坏死因子-α(TNF-α)、白細胞介素-1(IL-1)、C反应蛋白(CRP)及肌酸激酶(CK)进行检测,均采用酶联免疫吸附试验进行检测,试剂盒购于美国R&D公司,操作由专业人员严格按说明书进行。(3)髋臼假体位置:在术后第1天对患者进行骨盆正位X线片检查,对髋臼前倾角与外展角进行检测,以拍摄X线片后参照文献[7]进行计算前倾角与外展角。
1.4 統计学处理 采用SPSS 22.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用t检验,组内比较采用配对t检验;计数资料以率(%)表示,比较采用字2检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 对照组,男14例,女17例;年龄34~65岁,平均(50.18±6.94)岁;BMI 20.16~29.15 kg/m2,平均(26.17±3.02)kg/m2;CroweⅠ型18例,Ⅱ型13例。观察组男12例,女19例;年龄33~66岁,平均(50.29±7.02)岁;BMI 20.09~29.26 kg/m2,平均(26.05±3.11)kg/m2;CroweⅠ型16例,Ⅱ型15例。两组性别、年龄、BMI等一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
2.2 两组治疗效果比较 观察组治疗总有效率为96.77%与对照组的93.55%比较,差异无统计学意义(字2=0.350,P=0.554),见表1。
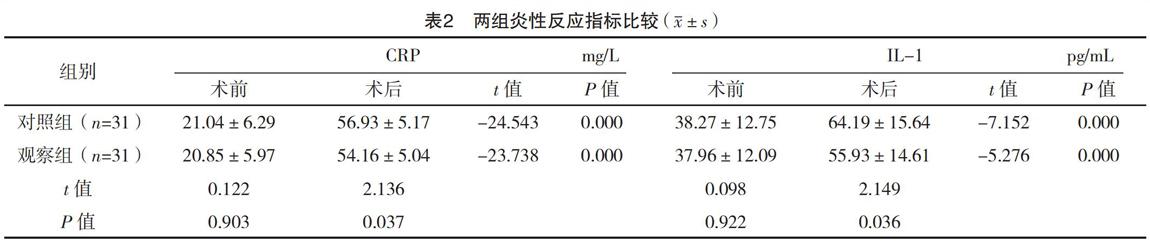
2.3 两组炎性反应指标对比 术后,两组CRP、IL-1、TNF-α及CK水平均明显高于术前,差异均有统计学意义(P<0.05);且对照组CRP、IL-1、TNF-α及CK水平均高于观察组,差异均有统计学意义(P<0.05)。见表2。
2.4 两组髋臼前倾角与外展角比较 两组髋臼前倾角与外展角比较,差异均无统计学意义(P>0.05),见表3。
3 讨论
髋臼发育为一种严重的髋关节疾病,目前对于该病的治疗方法主要有骨盆截骨、股骨截骨、髋关节融合及全髋关节置换术等,目前人工髋关节置换术被公认为是治疗髋臼发育不良的有效方法。临床上根据X线片检查结果将股骨头移位距离与股骨头高度比例分为四个亚型,其中CroweⅠ、Ⅱ型位置变异较小,本研究选取此类患者进行研究,因CroweⅢ、Ⅳ型患者股骨变异较大,同时合并有股骨畸形、骨赘增生、髋关节活动度小等问题在行直接前入路全髋关节置换术时手术风险明显升高,故暂时不对此类患者进行研究[8-10]。
髋关节置换术后关节功能受多方面因素的影响,包括收缩操作、假体设计、假体植入的正确性、手术入路的选择等[11-13]。随着髋关节的置换术在临床的开展后,大量学者对其手术入路进行了研究,主要有直接前侧入路、外侧入路、后侧入路、后外侧入路等,其中以后侧入路与直接前侧入路较为常用[14-16]。过去主要以后侧入路为主,随着全髋关节置换术研究的不断深入直接前侧入路逐渐被人们所认识,该入路最早在18世纪末由美国学者Carl Hueter所提出,后在1917年经S Perterson报道后才被逐渐认识,因此该入路又被称为Smith-Peterson入路[17]。本研究结果显示:观察组治疗总有效率为96.77%,与对照组的93.55%比较,差异无统计学意义(P>0.05)。两组髋臼前倾角与外展角比较,差异均无统计学意义(P>0.05),提示两种手术入路对患者疗效相当。髋臼假体位置时临床上判断人工全髋关节置换术成功与否的重要指标,髋臼假体位置不佳可对假体的稳定性造成影响而影响关节功能的恢复[18]。研究显示前倾角在0°~15°时随着前倾角的增加假体稳定性增加,但前倾角过大可增加拖尾的风险,同时前倾角增大还可增加髋臼屈曲范围但却缩小了后伸的活动范围,另外前倾角的增加使关节接触面积下降而使局部应力增大,加速关节的磨损。大量研究证实外展角(40±10)°、前倾角(20±5)°为髋臼假体安全区域[19],本研究发现两种手术入路前倾角及外展角均在此范围内,具有较高的安全性。IL-1、CRP、TNF-α为临床上常用于检测炎性反应的炎症因子,研究显示IL-1在髋关节置换及膝关节损伤中有重要的作用,且可协同TNF-α协同促进炎症的发展,CRP为急性时相反应蛋白,在感染、炎症、外科手术后均可明显升高,为一种非特异性的炎症标志物。本研究结果显示:术后两组CRP、IL-1、TNF-α及CK水平均比术前明显升高,且对照组均高于观察组(P<0.05),可能与直接前侧入路对患者软组织创伤更小,可有效保护肌肉组织,后侧入路虽然手术操作方便,容易学习掌握,但该入路需要劈开臀大肌,且还需将梨状肌与部分外旋肌切断,对髋关节后方关节囊及周围的肌肉组织均造成较大的损伤,因而炎性反应更剧烈[20]。
综上所述,直接前侧入路与常规后侧入路行全髋关节置换术对髋臼发育不良患者疗效相当且髋臼假体位置差别不大,但直接前侧入路全髋关节置换术能够减轻患者炎性反应。
参考文献
[1] Kaneuji A,Sugimori T,Ichiseki T,et al.Rotational Acetabular Osteotomy for Osteoarthritis with Acetabular Dysplasia:Conversion Rate to Total Hip Arthroplasty within Twenty Years and Osteoarthritis Progression After a Minimum of Twenty Years[J].
J Bone Joint Surg Am,2015,97(9):726-732.
[2] Gromov K,Greene M E,Huddleston J I,et al.Acetabular Dysplasia and Surgical Approaches Other Than Direct Anterior Increases Risk for Malpositioning of the Acetabular Component in Total Hip Arthroplasty[J].J Arthroplasty,2016,31(4):835-841.
[3] Gray B L,Stambough J B,Baca G R,et al.Comparison of contemporary periacetabular osteotomy for hip dysplasia with total hip arthroplasty for hip osteoarthritis[J].Bone Joint J,2015,97(10):1322-1327.
[4] Kalore N V,Cheppalli S P,Jiranek W A.Acetabular Dysplasia in Middle-Aged Patients:Periacetabular Osteotomy or Total Hip Arthroplasty?[J].J Arthroplasty,2016,31(9):1894-1898.
[5] Yuasa T,Maezawa K,Nozawa M,et al.Total hip arthroplasty after previous rotational acetabular osteotomy[J].Eur J Orthop Surg Traumatol,2015,25(6):1057-1060.
[6] Iwase T,Morita D,Ito T,et al.Favorable Results of Primary Total Hip Arthroplasty With Acetabular Impaction Bone Grafting for Large Segmental Bone Defects in Dysplastic Hips[J].
J Arthroplasty,2016,31(10):2221-2226.
[7]劉宇,桑伟林,姜亚飞,等.直接前方入路与后外侧入路行人工全髋关节置换术对髋臼假体位置影响的比较研究[J].中国修复重建外科杂志,2017,31(7):790-793.
[8] Ito H,Takatori Y,Moro T,et al.Total Hip Arthroplasty After Rotational Acetabular Osteotomy[J].J Arthroplasty,2015,30(3):403-406.
[9] Hara D,Hamai S,Komiyama K,et al.Sports Participation in Patients After Total Hip Arthroplasty vs Periacetabular Osteotomy:A Propensity Score-Matched Asian Cohort Study[J].J Arthroplasty,2018,33(2):423-430.
[10] Takada R,Jinno T,Miyatake K,et al.Longitudinal morphological change of acetabular subchondral bone cyst after total hip arthroplasty in developmental dysplasia of the hip[J].Eur J Orthop Surg Traumatol,2018,28(4):621-625.
[11] Oe K,Iida H,Kawamura H,et al.Long-term results of acetabular reconstruction using three bulk bone graft techniques in cemented total hip arthroplasty for developmental dysplasia[J].Int Orthop,2015,40(9):1949-1954.
[12] Osawa Y,Hasegawa Y,Seki T,et al.Significantly Poor Outcomes of Total Hip Arthroplasty After Failed Periacetabular Osteotomy[J].J Arthroplasty,2016,31(9):1904-1909.
[13] Osawa Y,Hasegawa Y,Okura T,et al.Total Hip Arthroplasty After Periacetabular and Intertrochanteric Valgus Osteotomy[J].
J Arthroplasty,2017,32(3):857-861.
[14] Zha G C,Sun J Y,Guo K J,et al.Medial Protrusio Technique in Cementless Total Hip Arthroplasty for Developmental Dysplasia of the Hip:A Prospective 6-to 9-Year Follow-Up of 43 Consecutive Patients[J].J Arthroplasty,2016,31(8):1761-1766.
[15] Verettas D A,Chloropoulou P,Xarchas K,et al.Small diameter acetabulum and femoral head in total hip arthroplasty for developmental dysplasia of the hip,with no femoral osteotomy[J].Hip Int,2015,25(3):209-214.
[16] Ohmori T,Kabata T,Maeda T,et al.Selection of a surgical approach for total hip arthroplasty according to the depth to the surgical site[J].Hip Int,2017,27(3):273-280.
[17] Miller L E,Gondusky J S,Kamath A F,et al.Influence of surgical approach on complication risk in primary total hip arthroplasty[J].Acta Orthopaedica,2018,89(3):289-294.
[18] Kawarai Y,Iida S,Nakamura J,et al.Does the surgical approach influence the implant alignment in total hip arthroplasty?Comparative study between the direct anterior and the anterolateral approaches in the supine position[J].Int Orthop,2017,41(12):2487-2493.
[19] Engdal M,Foss O A,Taraldsen K,et al.Daily Physical Activity in Total Hip Arthroplasty Patients Undergoing Different Surgical Approaches:A Cohort Study[J].Am J Phys Med Rehabil,2017,96(7):473-478.
[20] Kj?rgaard N,Kj?rsgaard J B,Petersen C L,et al.Thresholds for the Oxford Hip Score after total hip replacement surgery:a novel approach to postoperative evaluation[J].J Orthop Traumatol,2017,18(4):401-406.
(收稿日期:2019-05-28) (本文編辑:田婧)
